Case Report
2014
June
Volume : 2
Issue : 2
Aggressive fibromatosis – Case report and brief review of literature
Pratap Reddy T, Shitalkumar Surana, Lalitha, Jagadishwar Goud G, Sailaja M
Pdf Page Numbers :- 68-71
Pratap Reddy T1,*, Shitalkumar Surana1, Lalitha1, Jagadishwar Goud G2 and Sailaja M3
1 Department of Radiation Oncology, Krishna Institute of Medical sciences, Minister Road, Secunderabad - 500003, AP, India
2 Department of Surgical Oncology, Minimal Inavasive and Robotic assisted Laparoscopy, Krishna Institute of Medical sciences, Minister Road, Secunderabad - 500003, AP, India
3 Department of Laboratory Medicine, Krishna Institute of Medical sciences, Minister Road, Secunderabad - 500003, AP, India
*Corresponding author: Dr. Pratap Reddy, M.D.(RT), FUICC(USA), Head of the department, Radiation Oncology, Krishna Institute of Medical sciences, Minister Road, Secunderabad - 500003, AP, India. Email: thammipratap@rediffmail.com
Received 30 January 2014; Revised 6 March 2014; Accepted 12 March 2014
Citation: Pratap Reddy T, Shitalkumar Surana, Lalitha, Jagadishwar Goud G, Sailaja M (2014) Aggressive fibromatosis – Case report and brief review of literature. J Med Sci Res 2(2):68-71. DOI: http://dx.doi.org/10.17727/JMSR.2014/2-013
Copyright: © 2014 Pratap Reddy T et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Aggressive fibromatosis is a benign tumor which arises from deep musculoaponeurotic structures and can occur anywhere in the body. It is characterized by local invasion and recurrence. It has been reported to occur in the head and neck (H & N) region, with 179 cases documented between 1968 and 2008.
Full Text
Introduction
Aggressive fibromatosis is a benign tumor which arises from deep musculoaponeurotic structures [1] and can occur anywhere in the body. It is characterized by local invasion and recurrence. It has been reported to occur in the head and neck (H & N) region, with 179 cases documented between 1968 and 2008. Annual occurrence is 0.2 – 0.4 per 100,000, with origins in the head and neck accounting for 10– 25%. Since 1954 only 97 cases of paediatric head and neck fibromatosis are reported [2]. Head and neck region fibromatosis tends to be more aggressive and is associated with significant morbidity because of close proximity to the vital vascular and neurological structures. The current evidence suggests that surgery alone has a consistently high rate of local recurrence in managing extra-abdominal tumors. Radiation therapy in combination with surgery improves local control rates [3]. A case is reported an H & N fibromatosis in a 13-year-old girl.
Case report
13-year-old girl presented with 2 months history of firm, non-tender swelling in right upper neck just beneath the mandible. Mild deviation of tongue was noted by parents since the age of 2 years for which no medical advice was sought. There was no history of recent trauma. Family history was non-contributory. There was no history of pain or other associated sensory symptoms. On physical examination, mass was felt in submandibular and sublingual area which was firm and immobile. There was no restriction of mouth opening, overlying skin and intraoral mucosa was normal. MRI neck was done which revealed ill-defined hypo intense mass with areas of intensity, approximately 5 x 5.2 x 5.3 cm in size, in right sublingual, submandibular region extending to parapharyngeal space cranially upto base of skull with widening of foramen lacerum and medial aspect of greater wing of sphenoid. Lesion was found causing mass effect over posterior tongue and oropharynx. Lesion did not show enhancement after contrast administration.
Fine needle aspiration cytology (FNAC) from the lesion was suggestive of lipoma. After work up, patient underwent surgery with excision of tumour and right neck lymphadenectomy on in June 2012. Per-operative findings suggested 5 x 5 cm mass lesion in right submandibular region adherent to right carotid sheath at bifurcation & compressing right hypoglossal nerve. Post operative histopathology was reported as intramuscular lipoma.
Follow up MRI was done 6 months later in February 2013 which showed heterogenous signal with mild irregularity of margin involving genioglossus on right side and involvement of myeloglossus muscle. FNAC and biopsy of the mass did not show any malignant tumour. Immunohistochemistry was suggestive of fibromatosis. MRI was repeated in April 2013 which showed 5 x 5 x 4.5 cm sized lesion involving right posterior tongue with extension into subcutaneous soft tissues suggesting recurrence. Patient was advised re-excision but did not undergo surgery and tried alternative medicine for 6 months.
Patient again presented with increase in the size of swelling and slurring of speech 6 months later in Dec 2013. Clinically right submandibular area swelling with deviation of tongue was noted. MRI neck revealed progression of the recurrent lesion with size approximately 7.9 x 6.4 x 8 cm.
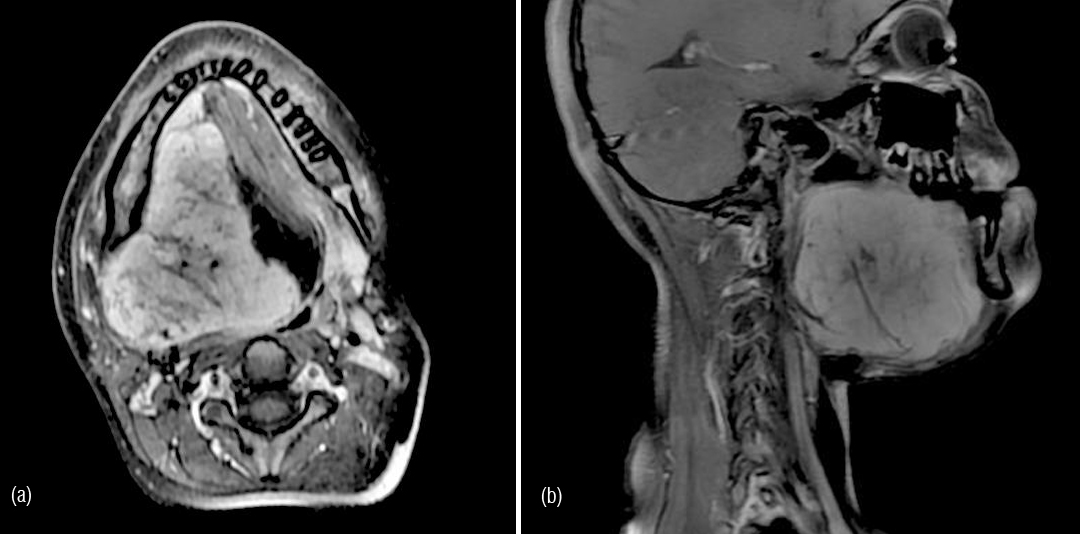
Figure 1a,b: MRI axial and saggital - lesion in right sublingual and submandibular region.
Patient underwent re-excision of the mass with mandibular osteotomy, reconstruction and temporary tracheostomy. Post operative histopathology showed circumscribed unencapsulated abundance of oval to spindle cells. Focal mild to moderate nuclear atypia was seen with rare mitotic figures noted in cellular areas. In the periphery, infiltration was seen in adjacent skeletal muscle bundle consistent with fibromatosis.

Figure 2a,b: Spindle shaped cells with no atypia.
Immunohistochemistry on spindle cells showed focal cytoplasmic positivity with SMA, diffuse nuclear positivity with beta-catenin and negativity for Desmin confirming the diagnosis of fibromatosis.
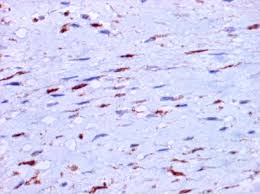
Figure 3: IHC with B-catenin showing focal positivity.
Post operatively patient recovered well and tracheostomy was closed. Patient was advised adjuvant treatment with radiation therapy using Image Guided Rapid Arc Technique.
Discussion
Aggressive fibromatosis in children is a rare, benign condition that is locally infiltrative and destructive. Dupuytren first described fibromatosis in 1839, regarding children he observed with palmar nodules. However, it was not fully recognized or published until 1954 when it was reported by Stout [4]. The literature suggests that pathogenesis of aggressive fibromatosis is most likely multifactor and genetic predisposition, endocrine factors, and trauma may play some role in the causation of these lesions. There has been association with gardner’s syndrome and familial adenomatous polyposis [5, 6].
Regression of fibromatosis has been described at menarche and tamoxifen, an anti-estrogen drug has been shown to have an inhibitory effect on aggressive fibromatosis suggesting the role of endocrine factor in etiology [7].
Head and neck fibromatosis represents around 12–15% of all lesions of which mandible and submandibular area shows almost half of the lesions [2]. It often presents as a rapidly growing, painless lump in the head and neck region. Excision biopsy is required for diagnosis in majority of cases. Beta catenin (β-catenin is a dual function protein, regulating the coordination of cell–cell adhesion and gene transcription) expression helps in diagnosing this condition [8].
Histologically, fibromatosis is a tumor of low cellularity which, according to the World Health Organization (WHO) classification, belongs between benign and malignant neoplasms. The tumors are composed of long, poorly defined fascicles of spindle-shaped fibroblasts in a rich collagen matrix. No atypical cells are seen, and mitoses are always few. Lymphocytes and macrophages may exist in the periphery.
Surgical excision with clear margins is the treatment of choice. Although spontaneous regressions are seen rarely even without therapy, clinical behaviour remains unpredictable with local recurrences seen even after seemingly complete excision with negative margins.
There have been some reports suggesting the role of cytotoxic chemotherapy in aggressive fibromatosis utilizing drugs such as methotrexate, vinblastine/ vinorelbine. Therapeutic responses also have been observed after noncytotoxic drugs such as anti-estrogens or non-steroidal anti-inflammatory drugs (NSAIDs).
Use of radiation therapy in inoperable, unresectable recurrent cases has been published in earlier studies [9, 10, 11, 12] with good local control rates. In a comparative review of 22 articles [13] local control after radiation or surgery combined with radiation was found to be superior to that of surgery alone. Adjuvant radiation therapy (RT) reduces local recurrence rates compared with surgery alone. With total RT dose of more than 50 Gy, the local recurrence rate decreases from 60% to 80% while with surgery alone rate reduces to 10% to 30% after adjuvant RT [14].
According to the patterns of case study done in Germany on the use of radiotherapy 59% were irradiated for locally recurrent or unresectable lesions out of the 345 patients subjected to evaluation. The long-term local control rate was 81.4% after primary radiotherapy of nonresectable lesions and 79.6% after adjuvant radiotherapy.
Conclusions
Aggressive fibromatosis remains a difficult disease to diagnose and treat. Aggressive surgical resection, with an attempt at negative margins is the standard treatment. Adjuvant therapy, such as radiation or chemotherapy is usually reserved for those cases that are either inoperable, or unresectable recurrences. Head and neck fibromatosis though rare, present a difficult problem as they are often recurrent aggressive tumours and invade local bone, nerve and muscles and may cause unacceptable cosmetic deformity. Due to its aggressive behaviour and tendency to invade local structures and recur, a multi-modality management strategy has to be employed. Radiation Therapy is indicated in inoperable cases, after R2 resection (resection with gross positive margins/ incomplete resection) and R1 resection (surgery with microscopic positive margins). If repeated surgery has failed further surgery may cause unacceptable deformity [14].
Acknowledgement
Acknowledgements are due to department of Radiology and Imaging, KIMS, Secunderabad.
Conflict of interest
The authors wish to express that they have no conflict of interest.
References
1. Sze H, Yeung MW. Fibromatosis of the neck. Hong Kong Med J. 2009; 15:221–223.
2. Peña S, Brickman T, StHilaire H, Jeyakumar A. Aggressive fibromatosis of the head and neck in the pediatric population. Int J Pediatr Otorhinolaryngol 2014, 78(1):1-4.
3. Wood TJ, Quinn KM, Farrokhyar F, Deheshi B, Corbett T, et al. Local control of extra-abdominal desmoid tumors: systematic review and meta-analysis. Rare Tumors 2013; 5(1):e2.
4. A.P. Stout. Juvenile fibromatoses. Cancer 1954, 7 (5):953–978.
5. Sharma A, Ngan BY, Sándor GK, Campisi P, Forte V. Pediatric aggressive fibromatosis of the head and neck: a 20-year retrospective review. J Pediatr Surg. 2008; 43(9):1596-1604.
6. Cristina Meazza. Aggressive Fibromatosis in Children and Adolescents. Cancer 2010; 116:233–240.
7. Carr RJ, Zaki GA, Leader MB, Langdon JD, Infantile fibromatosis with involvement of the mandible. Br J Oral Maxillofac Surg. 1992; 30(4):257-262
8. Flucke U, Tops BB, van Diest PJ, Slootweg PJ, Desmoid-type fibromatosis of the head and neck region in the paediatric population: a clinicopathological and genetic study of seven cases. Histopathology 2013; Nov 7.
9. Rüdiger HA, Ngan SY, Ng M, Powell GJ, Choong PF. Radiation therapy in the treatment of desmoid tumours reduces surgical indications. Eur J Surg Oncol. 2010; 36(1):84-88.
10. Park HC, Pyo HR, Shin KH, Suh CO. Radiation treatment for aggressive fibromatosis: findings from observed patterns of local failure. Oncology 2003; 64(4):346-352.
11. El-Haddad M, El-Sebaie M, Ahmad R, Khalil E, Shahin M, et al . Treatment of aggressive fibromatosis: the experience of a single institution. Clin Oncol. (R Coll Radiol). 2009; 21(10):775-780.
12. Guadagnolo BA, Zagars GK, Ballo MT. Long-term outcomes for desmoid tumors treated with radiation therapy. Int J Radiat Oncol Biol Phys. 2008; 71(2):441-447.
13. Nuyttens JJ. Surgery versus radiation therapy for patients with aggressive fibromatosis or desmoid tumors: A comparative review of 22 articles. Cancer. 2000; 88(7):1517-1523.
14. Perez, Brady's. Principles and Practice of Radiation Oncology. 6th Edition.