Full Text
Introduction
Refractive errors like myopia and astigmatism are considered the main cause of visual impairment worldwide [1]. Myopia is when the light rays which are parallel come to a focus in front of the retina when the eye is at rest. Basically it means the person can see objects at a short distance clearly, but the far off objects do not appear clear. Astigmatism is a condition of refraction where the point of focus of light cannot be formed upon the retina causing the patient to see blurred or distorted images [2].
Myopia is the most common type of refractive error which has a worldwide prevalence of 15 to 49% [3]. The World Health Organization has grouped myopia and uncorrected refractive error with cataract, macular degeneration, infectious disease, and vitamin A deficiency among the leading causes of blindness and vision impairment in the world [4].
The treatment modalities of myopia include spectacle correction, contact lenses, and various surgical procedures.
Photorefractive keratectomy is a procedure where the ultraviolet range energy generated by an argon fluoride (ArF) excimer laser is applied to the anterior corneal stroma to change its curvature and thus to correct the refractive error. The physical process of remodelling the corneal stroma by ultraviolet (193 nm wavelength) high-energy photons is known as photoablation [5].
We compared the visual outcome between the two procedures. We compared the post-operative complications namely corneal haze and pain in the two procedures.
Methodology
Prospective, randomized, interventional study conducted at a tertiary eye care centre in south India. Patients with mild to moderate myopia with or without astigmatism who underwent photorefractive keratectomy between Nov 2019 and May 2021 were enrolled. Patients were divided into two groups; in Group 1 the patients underwent alcohol assisted photorefractive keratectomy and in Group 2 excimer laser assisted epithelial removal photorefractive keratectomy was performed. The study protocol was approved by the institutional ethics committee and a signed informed consent was obtained from all patients. Patients were excluded if they failed to meet any of the above inclusion criteria or for the following reasons, patients with corneal ectasia like keratoconus, pellucid marginal degeneration, any previous ocular intervention involving corneal procedures, corneal herpetic disease or any corneal scar, history of ocular trauma, pregnancy, and patients not willing to give informed consent.
All patients had a complete preoperative eye examination including uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA) assessment, manifest and cycloplegic refraction, slit lamp biomicroscopy to evaluate the anterior segment, applanation tonometry and a detailed fundus examination.
All surgical procedures were performed by a single surgeon. After a povidone iodine scrub to the lashes and eyelids, a closed loop lid speculum was placed. One drop of proparacaine 0.5% was instilled in the eye. In excimer laser assisted epithelial removal photorefractive keratectomy, laser was applied using Zeiss Mel 90 ArF excimer laser at 193 nm wavelength and the epithelium is removed by keeping the settings at 55 microns for ablation depth with optical zone of 8mm. In the conventional alcohol assisted photorefractive keratectomy. 20% ethyl alcohol is placed on the cornea for 40 seconds and then a dry polyvinyl alcohol sponge was used to peel off the epithelium. Area is dried and then laser is applied after fixing the centration and completing fluence test to ablate the stroma to correct the refractive error. In both the procedures, wash was given with balanced salt solution to remove the debris. Following which 0.2 percent mitomycin C was instilled over the ablated area. For every dioptre error, mitomycin was exposed to the ablated area for 10 seconds. A thorough wash was given with balanced salt solution. Bandage contact lens was used to cover the raw area. Topical antibiotic 0.5% moxifloxacin eye drop, was instilled before closing.
Post operatively, patients were followed up on post-operative day 1 (POD1), then POD7, after 1 month, after 3 months and then after months. The bandage contact lens was removed on the 7th post-operative day. Patients were treated with 0.5% moxifloxacin eye drops and started on low dose steroid namely 0.1% fluromethalone 4 times a day till the epithelium heals. Steroids were tapered over 2 months. Along with these artificial tears, namely 0.1% sodium hyalauronate, was also used. BCVA was checked on POD1, POD7, after a month, after 3 months and after 6 months.
The patient was also evaluated postoperatively, on POD1 and POD7 for corneal haze by slit lamp biomicroscopy proposed by Fantes et al., (0 = no haze; 0.5 = trace haze on oblique illumination; 1 = corneal cloudiness not interfering with the visibility of fine iris details; 2 = mild effacement of fine iris details; 3 and 4 = details of the lens and iris not discernible) [6]. Immediately after surgery to evaluate the pain level a 5 point present pain intensity (PPI) scale of the standard long form McGill pain questionnaire (LF-MPQ) was used on POD1 and POD7. Pain severity score is as follows, 1=mild, 2= discomforting, 3= distressing, 4= horrible and 5= excruciating.
Statistical analysis
All the data was compiled and analyzed using Microsoft Excel and SPSS software. The data collected was analyzed statistically using descriptive statistics namely mean, standard deviation, percentage. Chi-Square test was used to determine association between the qualitative variables, namely sex. Student t test was used to determine significant difference between two groups. P <0.05 is considered statistically significant.
Sample size estimation
Based on the previous study, Naderi et al., pain score in transepithelial photorefractive keratectomy = 2.30±0.5 and pain score in alcohol assisted photorefractive keratectomy=3.3±0.7. Minimum expected difference = 0.5 [7].
Sample size calculation:

where Zα= standard table value for 95% CI = 1.9 .
Z1-β= standard table value for 80% power = 0.84
σ =standard deviation=0.4
d = effect size =0.5
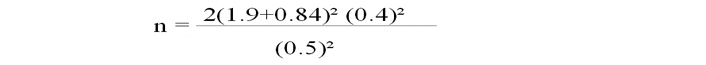
n = 25 each group
Results
During the study period from September 2019 to May 2021, a total of 50 patients were evaluated and were deemed fit to undergo refractive surgery. The patients have undergone either alcohol assisted photorefractive keratectomy or excimer laser assisted epithelial removal photorefractive keratectomy using the randomization software. In the post-operative period, the visual outcome, corneal haze and pain scale were noted and the data was analysed. In both groups, the mean age was almost similar with alcohol assisted photorefractive keratectomy being 25.80 ± 4.37 and the excimer laser assisted epithelial removal photorefractive keratectomy group being at 25.32 ± 4.52. The statistical method used here was student t test table.
Among the alcohol assisted group, 52 % were males and among the excimer laser assisted epithelial removal photorefractive keratectomy group 72% were females. But this is of no statistical significance as the patients were randomly divided based on randomization software.
The mean pre-operative UCVA was 0.81 ± 0.31 and 0.97 ± 0.35 in the alcohol assisted photorefractive keratectomy group and excimer laser assisted epithelial removal photorefractive keratectomy group respectively. The BCVA between two groups showed slight difference during the post-operative period with alcohol assisted photorefractive keratectomy being slightly better than the excimer laser assisted epithelial removal photorefractive keratectomy, but it was not statistically significant. The BCVA after 6 months for all patients irrespective of the group was 0.00 logmar units.
The corneal haze was comparable in both groups on Day one post operatively. But by day 7 after surgery, there was no haze in either group. Pain score, on POD1 was marginally better in the excimer laser assisted epithelial removal photorefractive keratectomy than the alcohol group, but it was not statistically significant. But by the end of 1wk, there is no pain in either groups.
1. Best corrected visual acuity
The best corrected visual acuity was measured on POD1, POD7, after 1 month, after 3 months, and after 6 months (Table 1) (Figure 1).
Table 1: Best corrected visual acuity of the two groups of study participants.
|
|
Alcohol assisted photorefractive keratectomy
|
Excimer laser assisted epithelial removal photorefractive keratectomy
|
P value
|
|
Mean ± SD
|
Mean ± SD
|
|
Baseline
|
0.03 ± 0.0
|
0.03 ± 0.08
|
0.50
|
|
POD1
|
0.11 ± 0.07
|
0.14 ± 0.07
|
0.033
|
|
POD7
|
0.10 ± 0.07
|
0.12 ± 0.07
|
0.119
|
|
1 Month
|
0.0002 ± 0.04
|
0.009 ± 0.03
|
0.217
|
|
3 Months
|
-0.008 ± 0.03
|
0
|
0.41
|
|
6 Months
|
0
|
0
|
--
|
2. Corneal haze
Corneal haze seen commonly in the post-operative period was quantified and analyzed. We deduced that the corneal haze was more in the alcohol assisted photorefractive keratectomy procedure than its counterpart on post-operative day but it was not statistically significant (Table 2).
Table 2: Corneal haze seen in the two groups post operatively.
|
|
Alcohol assisted photorefractive keratectomy
|
Excimer laser assisted epithelial removal photorefractive keratectomy
|
P value
|
|
Mean ± SD
|
Mean ± SD
|
|
Corneal Haze at Day1
|
0.98 ± 0.09
|
0.94 ± 0.1
|
0.143
|
|
Corneal Haze at Day7
|
0
|
0
|
--
|
3. Pain score
The pain score was more for the alcohol assisted group over the excimer laser assisted group, but was not statistically significant (Table 3).
Table 3: Pain score saw post-operatively in the two groups of study participants.
|
|
Alcohol assisted photorefractive keratectomy
|
Excimer laser assisted epithelial removal photorefractive keratectomy excimer laser assisted
|
P value
|
|
Mean ± SD
|
Mean ± SD
|
|
POD 1
|
3.08 ± 0.80
|
2.9 ± 0.
|
0.419
|
|
POD 7
|
0
|
0
|
--
|
Using student t test, the statistical analysis was done. We observe that the according to the pain score, it was marginally better on post-operative day one in the excimer laser assisted epithelial removal photorefractive keratectomy than the alcohol group, but it was not statistically significant. But by day 7, there is no pain.
Discussion
Myopia being a very common refractive error seen worldwide, requires more research into treatment modalities. With the emergence of refractive surgery, the dependence on contact lenses and spectacles has come down. photorefractive keratectomy, being a surface ablative procedure is making a comeback into the clinical practice with its high safety index and cost effective treatment.
Age
The mean age of our study was 25.80 ± 4.37 for the alcohol assisted photorefractive keratectomy group and 25.32 ± 4.52 for the excimer laser assisted epithelial removal photorefractive keratectomy group (p= 0.704). The minimum age to do refractive surgery is taken as 18 years.
Visual acuity
In our study the UCVA for the excimer laser assisted epithelial removal photorefractive keratectomy group was 0.97 ± 0.35 with the post-operative BCVA of 0.00 after months, whereas the UCVA for the alcohol assisted photorefractive keratectomy group was 0.81 ± 0.31 with the post-operative BCVA of 0.00 at 6 months.
In a prospective, non-randomized trial by Naderi et al., 170 patients divided equally into two groups and were treated by transepithelial photorefractive keratectomy and conventional photorefractive keratectomy [7]. BCVA of 0.00 was achieved in both groups, hence there was no significant difference between the two procedures (p=0.09).
In study by Kaluzny et al., 148 patients underwent transepithelial photorefractive keratectomy and 55 patients underwent alcohol assisted photorefractive keratectomy, the BCVA was 0.00 in 97 % of the cases in the transepithelial group and 0.00 in 94 % in the alcohol assisted group initially (p=0.45), at the end of 3 months both groups had similar results [8].
In a randomized prospective study by Clinch et al., they had taken 278 eyes of 173 patients and subjected to either transepithelial debridement or mechanical debridement during photorefractive keratectomy and they concluded that there was no significant difference between the BCVA of the two groups after 12 months after surgery [9].
In a randomized controlled trial by Carones et al., 25 patients underwent either mechanical debridement photorefractive keratectomy or alcohol assisted photorefractive keratectomy [10]. They concluded that the BCVA between the two groups was comparable (p=0.22).
In a retrospective matched controlled study by Gimbel et al., they concluded that there was tendency towards greater correction at months on the laser ablated epithelium photorefractive keratectomy, although it was not statistically significant [11].
In a randomized controlled trial by Ghoreishi et al., which included 25 patients undergoing photorefractive keratectomy where assigned either alcohol assisted photorefractive keratectomy or mechanical epithelial removal photorefractive keratectomy group [12]. The study concluded that there was no significant difference in the BCVA in the two groups (p= 0.08).
A prospective paired study by Abad et al. was done where 18 patients underwent alcohol assisted photorefractive keratectomy in one eye and the mechanical debridement of epithelium photorefractive keratectomy in the other eye [13]. They concluded that there was a no significant difference in trend of visual recovery in the alcohol treated eyes.
In an open, prospective, non-randomized clinical trial done by Balakrishnan et al in Singapore, they studied the efficacy, predictability, stability and safety of photorefractive keratectomy for the myopic correction [14]. They concluded that excimer laser photorefractive keratectomy is effective, safe and stable as a surgical modality for the treatment. Initial overcorrection in all patients was seen which regressed in 4 months.
In a study done by Luger et al., 33 patients were treated where one eye was subjected to transepithelial photorefractive keratectomy and one eye to alcohol assisted photorefractive keratectomy [15]. They concluded that the BCVA values are comparable in both the groups, and transepithelial photorefractive keratectomy is faster to perform than the alcohol assisted photorefractive keratectomy counterpart.
Post-operative corneal haze
In our study the post-operative corneal haze, for the excimer laser assisted epithelial removal photorefractive keratectomy group on POD1 was 0.94 ± 0.1 and was 0 at POD7 whereas in the alcohol assisted photorefractive keratectomy group it was 0.98 ± 0.09 and was 0 at POD1 and POD 7 respectively (p=0.143). Hence it is comparable in both the groups.
In the study conducted by Naderi et al., they found that the post-operative haze was 4.7% in the alcohol assisted photorefractive keratectomy and 4.1% in the transepithelial photorefractive keratectomy [7].
Similar results were seen in a prospective nonrandomized cohort study by Ashraf M. Bakhsh et al done on 200 eyes of 100 patients in Security Forces Hospital, Riyadh, Saudi Arabia [16]. The postoperative corneal haze incidence is less in the transepithelial photorefractive keratectomy group than the alcohol assisted photorefractive keratectomy group on all the follow up days, but by the end of months there is no significant difference. In conclusion the post-operative complications were more in alcohol assisted photorefractive keratectomy than in transepithelial photorefractive keratectomy, but both are highly effective and safe procedures.
In a randomized study by Ghanavati et al., 80 eyes of 40 patients were subjected to either mechanical debridement photorefractive keratectomy or transepithelial photorefractive keratectomy, and the postoperative corneal haze was evaluated and was not clinically severe in either group and was not significant difference between the two groups (p=0.72) after months [17].
In the randomized study by Carones et al., 93 eyes underwent alcohol assisted photorefractive keratectomy and 97 eyes underwent the mechanical debridement photorefractive keratectomy [10]. They concluded that the corneal haze was lesser in the alcohol assisted photorefractive keratectomy group versus the mechanical debridement photorefractive keratectomy group (p=0.04).
In the study by Abad et al., they concluded that the post-operative corneal haze was comparable in both groups which was not statistically significant [13].
Post-operative pain score
In our study the pain score used was 5 point present pain intensity (PPI) scale of the standard long form McGill pain questionnaire (LF-MPQ). On post-operative day one, mean pain score was 2.9 ± 0. In excimer laser assisted epithelial removal photorefractive keratectomy group and 3.08 ± 0.80 in alcohol assisted photorefractive keratectomy group, which was not statistically significant (p=0.143).
In the study by Naderi et al., the procedure was better tolerated by patients who underwent transepithelial photorefractive keratectomy versus the patients who underwent alcohol assisted photorefractive keratectomy (p=0.04) [7].
In a prospective double-masked randomized study included 5 eyes of 28 myopic patients who received traditional photorefractive keratectomy in one eye and advanced surface ablation in the contralateral eye, by Blake et al., they concluded that the advanced surface ablation eyes had more pain than the traditional photorefractive keratectomy eyes, though it was not statistically significant ( p= 0.3337) [18].
In a randomized study by Ghanavati et al., 80 eyes of 40 patients were subjected to either mechanical debridement photorefractive keratectomy or transepithelial photorefractive keratectomy [17]. Patients reported more pain in the transepithelial photorefractive keratectomy group (p=<0.001) in the first week, along with tearing, photophobia, and foreign body sensation. By the second week it subsided and was not statistically significant.
In the study by Ghoreishi et al., it was concluded that there was not much difference in the pain score between the two groups [12].
In a study by Gharieb et al, they concluded that pain was higher in the transepithelial photorefractive keratectomy than in the alcohol assisted photorefractive keratectomy [19].
Post-operative corneal haze was mainly tackled using antimetabolite mitomycin C which needs to be titrated so as to prevent regression and scarring. Pain was present in both procedures which is expected in photorefractive keratectomy, making it one of drawbacks of the procedure as compared to LASIK or SMILE. There was no statistical significant difference in pain perception between two groups.
Limitations of our study
Coming to the limitations of the study, we have taken only 50 patients in this study. To establish a more rigid comparison we need to increase our sample size. In the excimer laser assisted epithelial removal photorefractive keratectomy we set the ablation depth at a fixed value of 55 microns. The normal epithelium can be between 48-55 microns. Patients undergoing excimer laser assisted epithelial removal photorefractive keratectomy are subjected to the excimer laser which ablates the epithelium at a fixed thickness of 55 microns. Hence a small margin of over or under correction can be seen. To improve the precision here, epithelial mapping can be done pre operatively to get the exact thickness of the epithelium we need to ablate.
Conclusion
Two-step excimer laser assisted epithelial removal photorefractive keratectomy and conventional photorefractive keratectomy performed on regular corneas produce very similar results months after the surgery. The findings in this study even though are not statistically significant, shows good unaided postoperative visual acuity in both the procedures with an excellent safety profile. Overall patient satisfaction in both the types of procedures is high with Mel 90 laser system. These procedures are predictable, effective, and safe for correction of myopia and compound myopic astigmatism. However a larger sample size may be required to establish a significant difference between the procedures.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Xi L, Zhang C, He Y. Clinical outcomes of Transepithelial photorefractive keratectomy to treat low to moderate myopic astigmatism. BMC ophthalmology. 2018; 18(1):115.
[2] Daniel S. The Practice of Refraction| Stewart Duke-Elder Sir, The Practice of Refraction., eighth, Mosby, St. Louis (199), pp. 94–102.
[3] Guo H, Hosseini-Moghaddam SM, Hodge W. Corneal biomechanical properties after smile versus flex, lasik, lasek, or photorefractive keratectomy: a systematic review and meta-analysis. BMC Ophthalmol. 2019; 19(1):17.
[4] Pararajasegaram R. Vision 2020—the right to sight: from strategies to action. Am J Ophthalmol 1999; 182:359–370.
[5] Mc-Donald M. Surgical technique for RK. Highlights of ophthalmology. World Atlas Series of Ophthalmic Surgery Vol 1. 1993:111–120.
[6] Fantes FE, Hanna KD, Waring GO, Pouliquen Y, Thompson KP, et al. Wound healing after excimer laser keratomileusis (photorefractive keratectomy) in monkeys. Archives of Ophthalmology. 1990; 108(5):5–75.
[7] Naderi M, Jadidi K, Mosavi SA, Daneshi SA. Transepithelial photorefractive keratectomy for low to moderate myopia in comparison with conventional photorefractive keratectomy. J Ophthalmic Vis Res. 2016 ; 11(4):358–362.
[8] Kaluzny BJ, Cieslinska I, Mosquera SA, Verma S. Single-step transepithelial PRK vs alcohol-assisted PRK in myopia and compound myopic astigmatism correction. Medicine (Baltimore). 2016; 95(6):e1993.
[9] Clinch TE, Moshirfar M, Weis JR, Ahn CS, Hutchinson CB, Jeffrey JH. Comparison of mechanical and transepithelial debridement during photorefractive keratectomy. Ophthalmology. 1999; 10(3):483–489.
[10] Carones F, Fiore T, Brancato R. Mechanical vs. alcohol epithelial removal during photorefractive keratectomy. J Refractive Surg. 1999; 15(5):556–562.
[11] Gimbel HV, DeBroff BM, Beldavs RA, Westenbrugge JA, Ferensowicz M. Comparison of laser and manual removal of corneal epithelium for photorefractive keratectomy. J Refractive Surg. 1995; 11(1):36–67.
[12] Ghoreishi M, Attarzadeh H, Tavakoli M, Moini HA, Zandi A, et al. Alcohol-assisted versus mechanical epithelium removal in photorefractive keratectomy. J Ophthalmic Vis Res. 2010; 5(4):223.
[13] Abad JC, Talamo JH, Vidaurri-Leal J, Cantu-Charles C, Helena MC. Dilute ethanol versus mechanical debridement before photorefractive keratectomy. J Cataract Refract Surg. 1996; 22(10):1427-1433.
[14] Balakrishnan V, Lim AS, Low CH, Lee CP, Tseng PS, et al. Excimer laser photorefractive keratectomy in Singapore--a new treatment modality for myopia. Singapore Med J. 1993; 34(4):309–312.
[15] Luger MH, Ewering T, Arba-Mosquera S. Consecutive myopia correction with transepithelial versus alcohol-assisted photorefractive keratectomy in contralateral eyes: one-year results. J Cataract Refract Surg. 2012; 38(8):1414–1423.
[16] Bakhsh AM, Elwan SA, Chaudhry AA, El-Atris TM, Al-Howish TM. Comparison between transepithelial photorefractive keratectomy versus alcohol-assisted photorefractive keratectomy in correction of myopia and myopic astigmatism. J Ophthalmol. 2018; 2018:5376235.
[17] Zarei-Ghanavati S, Shandiz JH, Abrishami M, Karimpour M. Comparison of mechanical debridement and trans-epithelial myopic photorefractive keratectomy: A contralateral eye study. J Curr Ophthalmol. 2019; 31(2):135–141.
[18] Blake CR, Cervantes-Castañeda RA, Macias-Rodríguez Y, Anzoulatous G, Anderson R, et al. Comparison of postoperative pain in patients following photorefractive keratectomy versus advanced surface ablation. J Cataract Refract Surg. 2005; 31(7):1314–1319.
[19] Gharieb HM, Mo’mena Ahmad A, Ahmed AA, Othman IS. Transepithelial laser versus alcohol assisted photorefractive keratectomy safety and efficacy: 1-year follow-up of a contralateral eye study. Korean J Ophthalmol. 2021; 35(2):142.