Case Report
2022
June
Volume : 10
Issue : 2
A case of primary antiphospholipid antibody syndrome with intermittent cerebral venous sinus thrombosis manifested with recurrent epilepsy
Tanwar VS, Singh AA, Tank R, Saini A, Jatana S, Singh S
Pdf Page Numbers :- 105-108
Vikram Singh Tanwar1,*, Anurag Ambroz Singh1, Rakesh Tank1, Anjali Saini1, Sugam Jatana1 and Shobhit Singh1
1Department of Medicine, Shaheed Hasan Khan Mewati Government Medical College, Nalhar-122107, India
*Corresponding author: Dr. Vikram Singh Tanwar, Associate Professor, Department of Medicine, Shaheed Hasan Khan Mewati Government Medical College, Nalhar-122107, India. Email: drvikrampgi@gmail.com
Received 1 February 2022; Revised 9 March 2022; Accepted 18 March 2022; Published 28 March 2022
Citation: Tanwar VS, Singh AA, Tank R, Saini A, Jatana S, Singh S. A case of primary antiphospholipid antibody syndrome with intermittent cerebral venous sinus thrombosis manifested with recurrent epilepsy. J Med Sci Res. 2022; 10(2):105-108. DOI: http://dx.doi.org/10.17727/JMSR.2022/10-20
Copyright: © 2022 Tanwar VS et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Antiphospholipid syndrome (APS) is an acquired autoimmune clinical disorder characterized by persistently raised levels of anti-phospholipid antibodies and clinical feature of hypercoagulability (recurrent vascular thrombosis and pregnancy morbidities). Primary APS is idiopathic in nature though secondary APS is associated with other connective tissue diseases like SLE. Here, we present an instance of primary APS with recurrent cerebral venous sinus thrombosis in a youthful unmarried female who clinically presented with generalized epilepsy. Level of anti-cardiolipin (aCL) and anti-beta 2 GP1 antibodies were found elevated on two occasions 12 weeks apart. The patient was treated with anticoagulation therapy along with anti-epileptic therapy and she responded well to the therapy. This case report highlights that clinicians should always suspect APS in female patients who had history of seizures and ischemic or thrombotic lesions on brain imaging, irrespective of presence of pregnancy comorbidities.
Keywords: antiphospholipid syndrome; cerebral venous; sinus thrombosis; epilepsy
Full Text
Introduction
Antiphospholipid syndrome (APS) is a complex clinical condition, which describes the clinical association between antiphospholipid antibodies (aPL) and a syndrome of hypercoagubility [1]. In 1983 it was first described by Prof. Graham RV Hughes as a clinical syndrome that encompasses recurrent pregnancy loss, arterial or venous thrombosis and thrombocytopenia associated with aPL detected in serum [2]. It is described as primary if there is no associated connective tissue disease or secondary if there is [3, 4]. The clinical presentation of APS is heterogeneous and the manifestation depends on the organs involved. Venous thromboses are the presenting feature in up to 30% of patients with APS [5]. APS related thrombosis commonly involves upper and lower extremity deep veins and less commonly involves superior and inferior vena cava, hepatic veins (Budd Chiari Syndrome), portal vein and renal veins, and rarely involves cerebral venous sinuses and retinal veins [1, 2]. Female patients with APS generally present with RPL however, thrombosis of cerebral venous sinuses (CVT) may occur on rare instances. The risk of APS related CVT is greatly increased during late pregnancy and, even more so, during the puerperium [6]. APS related CVT is a quite uncommon manifestation in a patient without obstetric problem. APS-related pregnancy morbidities include premature births, spontaneous abortions, and fetal death [7]. We here presenting a unique case of APS related recurrent CVT in a young female patient without any pregnancy related morbidity and other stigmata of hypercoagubility who presented with multiple episodes of generalized epilepsy.
Case presentation
A sixteen years old unmarried female was brought to our emergency department with complaints of multiple episodes of abnormal body movements followed by altered sensorium since 2 hours. There was history of frothing from mouth, tongue bite and involuntary micturition during the episode present. Abnormal body movements involved both lower limbs in the beginning followed by rapid involvement of upper limbs, face and trunk and were tonic-clonic in nature. There was significant history of single episode of seizure 2 months back for which she didn't receive any treatment. There was no history of associated fever, preceding headache, abnormal behavior and any trauma to the head. There was no history of drug allergy, photosensitivity, skin rashes, oral ulceration and joint pain present. At admission, she was partially conscious, disoriented to time and place. Planter reflex on both side showed extensor response. Rest sensory and motor examination couldn’t be performed due to poor mental status of the patient. Cardiac examination was normal. Hemodynamic parameters including blood pressure and pulses were normal.
The initial treatment including anti-epileptic drug was given to abort and prevent further seizure episodes. After stabilization of the patient, MRI brain was done which revealed multiple small acute infarctions in bilateral basal ganglia, and bilateral centrum semiovale along with vasogenic edema and swelling in bilateral thalami likely secondary acute venous infarctions and edema (Figure 1). Encephalomalacia and gliosis in both parietal lobes, chronic lacunar infarct in the right basal ganglia and gliosis in the posterior corpus callosum along with atrophy of left hippocampus suggestive of sequel previous vascular insult (Figure 1). Hence, MR venography brain was done that revealed complete loss of flow related enhancement in the right transverse and sigmoid sinuses, internal cerebral veins, thalamostriate veins and veins of Rosenthal suggestive of thrombosis of sinuses and deep veins (Figure 2).
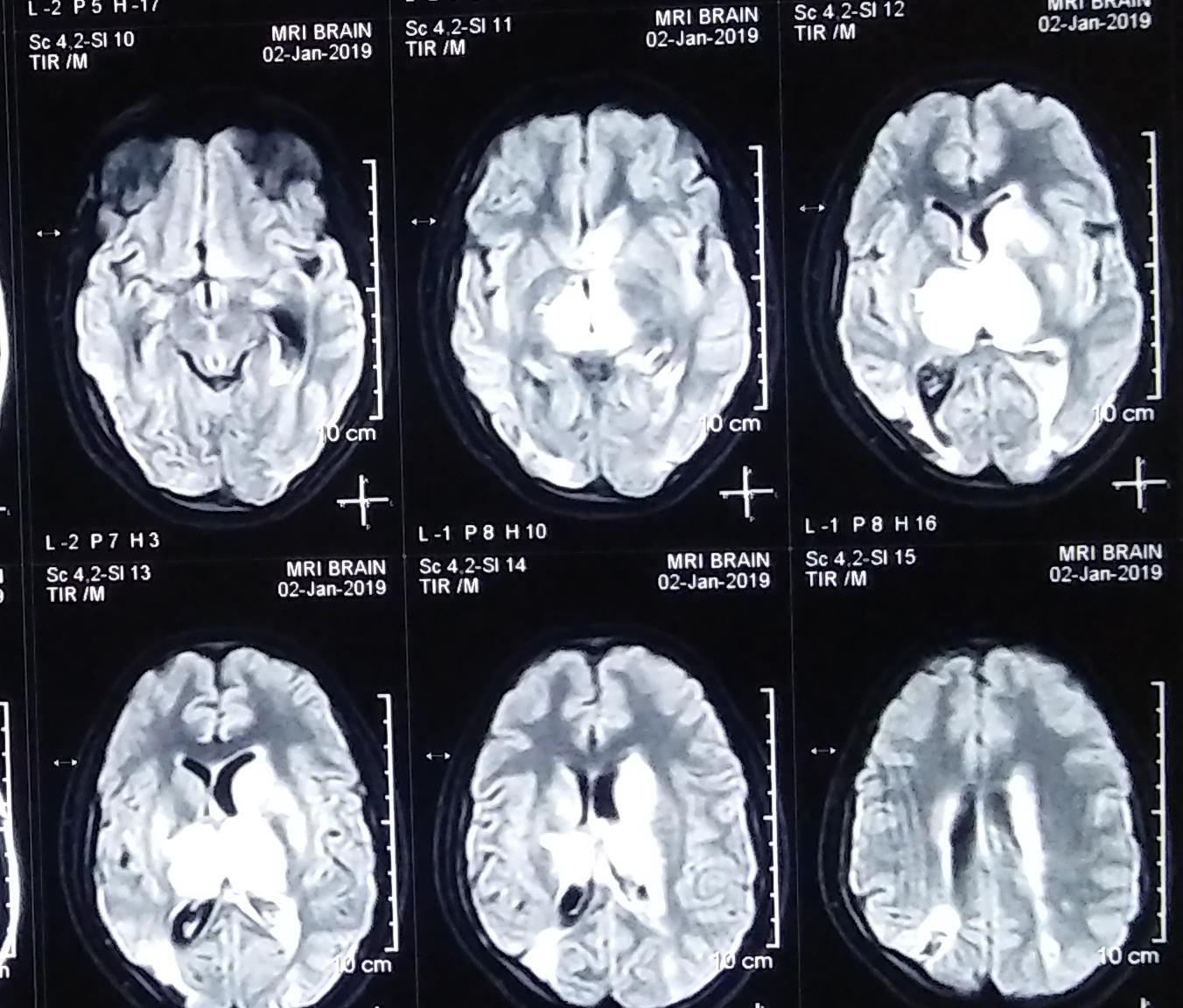
Figure 1: MRI brain showing multiple small acute infarctions in bilateral basal ganglia, and bilateral centrum semiovale along with vasogenic edema and swelling in bilateral thalami suggestive of secondary acute venous infarctions and edema.
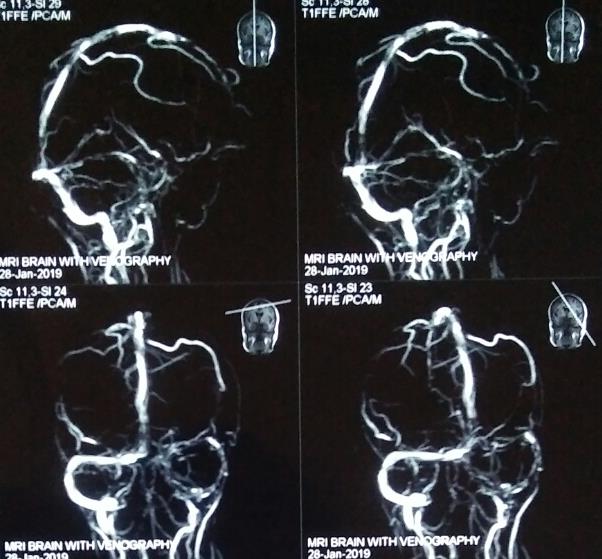
Figure 2: MR venography brain showing complete loss of flow related enhancement in the right transverse and sigmoid sinuses, internal cerebral veins, thalamostriate veins and veins of Rosenthal suggestive of thrombosis of sinuses and deep veins.
Presence of acute venous infarctions in brain parenchyma, thrombosis of venous sinuses and evidence of previous venous infarct along with a significant clinical history in a young female made high possibility of some hypercoagulable states like antiphospholipid antibody syndrome (APS). Hence, tests for lupus anticoagulant in the plasma, anti-cardiolipin antibody (aCL) and anti-beta 2 GP1 antibodies were obtained. Level of aCL and anti-beta 2 GP1 antibodies were present in high titer in the patient’s sera. However, test result for lupus anticoagulant (LA) was negative. Results of other tests were as follows: anti-nuclear antibody (ANA)- negative; anti-dsDNA- negative; serological tests for HIV, HBsAg and anti-HCV – negative; venereal disease research laboratory (VDRL) - negative; bleeding time (BT), clotting time (CT) and prothrombin time (PT)- within normal range; hemoglobin -13gm/dl; platelet counts- 1.9 lakhs. 2D-echocardiography revealed normal cardiac function with no thrombus in any chamber of the heart. Color Doppler for both carotids revealed normal intimal medial thickness. Color Doppler for both limbs revealed no evidence of deep and superficial vein thrombosis. Thus, the clinical findings and test results were more in favor of APS, so treatment was started accordingly. In addition to anti-epileptic therapy, anticoagulation therapy was started with injection enoxaparin, which was subsequently overlapped and switched over to warfarin, aiming to maintain international normalized ration (INR) between ranges of 2 to 3. Patient was also put on oral Aspirin 75mg per day. With this, the patient improved symptomatically and she was discharged on oral anticoagulation and antiepileptic therapy with further follow up in outpatient department. Her APS profile was repeated at 12 weeks following discharge and found positive for aCL and anti-beta 2 GP1 antibodies, which made our diagnosis, confirmed as primary APS. Hence, she was planned for lifelong anticoagulation. Patient and her attendants were explained about the disease, its progression, complications, outcome and need of life long treatment with importance of regular monitoring of INR.
Discussion
Antiphospholipid syndrome (APS), also known as Hughes syndrome an autoimmune clinical condition associated with the synthesis of autoantibodies against membrane phospholipids and phospholipid binding proteins (PLBP) [1]. Anti-phospholipid antibodies (aPL) cause activation of endothelial cells, oxidant mediated injury and modulation of natural anticoagulants, which lead to vasculopathy, and promotion of coagulation ultimately causing vascular thrombosis [2]. Thus, APS increases the risk of arterial thrombosis (myocardial infarction, stroke), venous thrombosis (commonly involve deep veins of legs, cerebral venous sinuses rarely), and obstetric failure due to involvement of placental vessels.
The Diagnosis of this clinical entity is made by revised Sapporo criteria (Table 1), which are based on clinical and laboratory parameters [1, 4, 7]. The major aPLs detected APS patients are anti-β2GP1, aCL antibody and lupus anticoagulant (LA). Detection of aPLs must be persistent (present for more than 12 weeks duration) because transient aPL detection may occur in some infections and medications. Approximately 20% of HCV positive patients and up to 50% patients infected with HIV have associated aPLs but no increased risk of thrombosis has been demonstrated in these infections [8-10]. Positivity for aPL occurs in many bacterial infections including leprosy, tuberculosis, syphilis and leptospirosis [8, 9]. It may be the first antibody to be appearing in SLE and even may predate the diagnosis of SLE by up to 7 years [8]. The presence of these antibodies, especially LA, is a predictor for thrombosis as up to 50% of patients with LA develop DVT [11]. However, our patient was negative for LA and she had not any history of DVT of lower limbs.
Table 1: Revised Sapporo diagnostic criteria for APS [1, 7].
|
Clinical criteria
|
Laboratory criteria
|
|
1. Vascular thrombosis: Venous or venous
2. Pregnancy comorbidity:
Any one of the followings-
a) One or more premature births of a morphologically normal fetus at or beyond the tenth week of gestation.
b) One or more premature births of a morphologically normal neonate before the 34th week of gestation because of eclampsia, severe preeclampsia or placental insufficiency.
c) Three or more unexplained consecutive spontaneous abortions before the 10th week of gestation.
|
Presence of intermediate or high titer of any one or more of the following antibodies:
1. Anti-cardiolipin IgM and IgG
2. Lupus anti-coagulant (LA)
3. Anti-beta 2 GP1 antibodies (anti-β2GP1)
|
|
Note: *Antibodies should be positive on two or more occasions, at least 12 weeks apart; **One clinical and one laboratory criteria should be met to make the diagnosis.
|
Central nervous system (CNS) is not spared from APS; even CNS involvement is one of the most prominent features of APS. CVT is the uncommon life threatening neurological manifestation of APS. Ferro JM et al found CVT in 5.9% patients of APS in their study [12]. Cervera et al, reported CVT only in 7 out of 1000 patients with APS [13]. Most patients having APS related CVT present with headache and focal neurological deficits [14]. Less common presentations are epileptic seizures, impaired sensorium, and cognitive dysfunction [5]. The aPL antibodies have been found to be associated with the epileptic seizures, especially in secondary APS [15]. Herranz et al found a statistically significant high prevalence of aPL in SLE patients with seizures compared with control SLE patients [16]. Liou et al found that epilepsy may be a primary neuropsychiatric event associated with high titers of aCL antibodies in SLE patients [17]. A recent study recruited 88 patients with primary APS and found nine (10.2 per cent) suffered from seizures [18]. Delgado MG et al, reported a case of 77-year-old female who presented with recurrent CNS manifestations for 3 years and her pro-coagulation profile test revealed LA, anti-beta2GP1 and aCL antibodies positivity and diagnosed as APS [19]. There are only few case reports where PAPS presented primarily with seizures without having pregnancy morbidities. Taipa & Santos reported a case of PAPS where encephalopathy, seizure and psychosis were the presenting manifestations [20]. Our case also had evidences of recurrent thrombosis in cerebral venous sinuses on brain imaging which makes our case more specific and uncommon.
There is no standard therapy available other than anticoagulation. Patients of APS-related thrombosis require life-long anticoagulation therapy preferably with warfarin aiming to achieve an international normalized ratio (INR) ranging from 2.5 to 3.5, alone or in combination with 75 mg of aspirin daily [1, 21, 22]. Pregnancy morbidity is prevented by a combination of heparin with aspirin 75 mg daily. Intravenous immunoglobulin (IVIg) 0.4g/ kg per day for 5 days may also prevent abortions, whereas glucocorticoids are ineffective [1].
Conclusion
Antiphospholipid syndrome is one of the important causes of young ischemic stroke and cerebral venous sinus thrombosis. Clinicians should always consider this clinical entity as a differential diagnosis especially in young female patients with or without history of pregnancy morbidities, who have history of recurrent seizures and have ischemic/ thrombotic lesions on brain imaging. Anticoagulation therapy should be started as soon as diagnosis is made as it may influence the course and outcome of the disease.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Moutsopoulos HM, Vlachoyiannopoulos PG. Antiphospholipid syndrome. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, editors. Harrison’s Principles Internal medicine 19thedi new york: Mcgraw hill, 2015; pp.2134–2136.
[2] Antiphospholipid Syndrome (Hughes syndrome). In: Paul BJ, editor. Essentials of clinical rheumatology. New delhi: Evangel Publishing, 2021; pp.120–125.
[3] Keeling D, Mackie I, Moore G, Greer IA, Greaves M, et al. Guidelines on the investigation and management of antiphospholipid syndrome. Br J Haematol. 2012; 157(1):47–58.
[4] Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). Thromb Haemost. 2006; 4(2):295–300.
[5] Cervera R, Piette JC, Font J, Khamastha MA. Euro-phospholipid project group. Antiphospholipid syndrome: clinical and immunologic manifestations and patterns of disease expression in a cohort of 1000 patients. Arthritis Rheum 2002; 46(4):1019–1027.
[6] Marwah S, Shailesh GH, Gupta S, Sharma M, Mittal P. Cerebral Venous Thrombosis in Pregnancy-A Poignant Allegory of an Unusual Case. J Clin Diagn Res. 2016; 10(12):QD08–QD09.
[7] Wilson WA, Gharavi AE, Koike T, Lockshin MD, Branch DW, et al. International consensus statement on preliminary classification criteria for definite antiphospholipid syndrome: report of an International Workshop. Arthritis Rheum. 1999; 42(7):1309–1311.
[8] Biggioggero M, Meroni PL. The geoepidemiology of the antiphospholipid antibody syndrome. Autoimmunity reviews. 2010; 9:A299–A304.
[9] Ramos-Casal M, Cervera R, Lagrutta M, Medina F, Garcia Carrasco M, et al. Clinical features related to antiphospholipid antibody syndrome in patients with chronic viral infections [hepatitis C virus/ HIV infection]: decription of 82 cases. Clin Infect Dis. 2004; 38(7):1009–1016.
[10] Sene D, Piette JC, Cacoub P. Antiphospholipid antibodies, antiphospholipid syndrome and infections. Autoimmunity reviews. 2008; 7(4):272–277.
[11] Petri M. update on antiphospholipid antibodies in SLE: the Hopkins lupus cohort. Lupus. 2010; 19(4):419–23.
[12] Ferro J.M. Prognosis of cerebral vein and dural sinus thrombosis: results of the international study on cerebral vein and dural sinus thrombosis (ISCVT). Stroke. 2004; 35(3):664–670.
[13] Cervera R, Piette JC, Font J, Khamashta MA, Shoenfeld Y, et al. Antiphospholipid syndrome: Clinical and immunologic manifestations and patterns of disease expression in a cohort of 1,000 patients. Arthritis Rheum. 2002; 46(4):1019–1027.
[14] Lienas AJ, Mathian A, Aboab J, Crassard I, Hie M, et al. Cerebral vein thrombosis in the antiphospholipid syndrome: analysis of a series of 27 patients and review of the literature. Brain Sci. 2021; 11(12):1641.
[15] Shoenfeld Y, Lev S, Blatt I, Blank M, Font J, et al. Features associated with epilepsy in the antiphospholipid syndrome. Journal of Rheumatology, 2004; 31(7):1344–1348.
[16] Herranz MT, Rivier G, Khamashta MA, Blaser KU, Hughes GRV. Association between antiphospholipid antibodies and epilepsy in patients with systemic lupus erythematosus. Arthritis Rheum. 1994; 37:568–571.
[17] Liou HH, Wang CR, Chen CJ, Chen RC, Chuang CY, et al. Elevated levels of anticardiolipin antibodies and epilepsy in lupus patients. Lupus. 1996; 5(4):307–312.
[18] de Carvalho JF, Pasoto SG, Appenzeller S. Seizures in primary antiphospholipid syndrome: the relevance of smoking to stroke. Clin Dev Immunol. 2012; 2012:1–7.
[19] Delgado MG, Rodríguez S, García R, Sánchez P, Sáiz A, et al. Antiphospholipid syndrome of late onset: a difficult diagnosis of a recurrent embolic stroke. Journal of Stroke and Cerebrovascular Diseases. 2015; 24(8):e209–e211.
[20] Taipa R, Santos E. Primary antiphospholipid antibody syndrome presenting with encephalopathy, psychosis and seizures. Lupus. 2011; 20(13):1433–1435.
[21] Khamashta MA, Cuadrado MJ, Mujic F, Taub NA, Hunt BJ, et al. The management of thrombosis in the antiphospholipid-antibody syndrome. N Engl J Med. 1995; 332(15):993–997.
[22] Derksen RH, de Groot PG, Kater L, Nieuwenhuis HK. Patients with antiphospholipid antibodies and venous thrombosis should receive long-term anticoagulant treatment. Ann Rheum Dis. 1993; 52(9):689–692.