Full Text
Introduction
Chronic obstructive pulmonary disease (COPD) is a condition characterized by obstruction of airways that is not fully reversible [1].
COPD is a broader term which includes the following 3 conditions, (1) Emphysema – Pathologically defined by destruction and enlargement of the lung alveoli, (2) Chronic bronchitis- A clinically defined condition with chronic cough and phlegm and (3) Small airways disease- Condition in which small bronchioles are narrowed.
Chronic obstructive pulmonary disease (COPD) is the sixth leading cause of death hence measures to implement awareness among public might prove to reduce the burden. Estimations of Global initiative for chronic obstructive lung disease (GOLD) suggest that COPD will rise to the third most common cause of death world wide by 2020. Following an acute exacerbation of COPD, majority of the patients often have exacerbations which decreases the quality of life and reduce the working days as well. Moreover, more than half the patients discharged, often require re-admission in the subsequent six months. Thus, the economic and social burden created by acute execrations of COPD are extremely high [2]. Also, cardiovascular diseases are more common among COPD patients and also in patients with asthma COPD overlap syndrome [3, 4].
Smoking is the major risk factor for COPD and a number of other illness, often coexist in COPD patients [5]. Although we know that exacerbations are key events in chronic obstructive pulmonary disease (COPD), our understanding of their frequency, determinants, and effects is incomplete [6]. It has been shown that the best predictor of exacerbations was a previous history of exacerbations and the second predictor being a history of reflux or heartburn [7]. Though the COPD patients mostly present with the features of acute respiratory infections (productive cough, dyspnea etc.), there may be a number of metabolic derangements arising out of the disease process or as a consequence of the therapy instituted like hyponatremia, hypokalemia, elevated transaminases, elevated blood urea.
In chronic respiratory acidosis as commonly seen in COPD patients, compensation takes place by kidney by retaining more bicarbonate [8]. COPD patients are prone to develop hyponatremia due to pulmonary illness, heart or renal failure, diuretics use, SIADH, and also due to the use of bronchodilators or steroids [9]. Also it is found that elevated plasma arginine vasopressin (AVP) in COPD may cause hyponatremia [10]. Though most of these features are correctable, very often they are missed or confuse the diagnosis [11]. Hypokalemia in also seen COPD patients, reasons attributed are long standing steroid therapy, beta 2-adrenoceptor agonist usage [12, 13].
As there is paucity of studies on the electrolyte disturbances in COPD in the current literature, a clinical study of these electrolyte derangements in COPD can help us determine its significance in predicting the outcome.
Aims and objectives
To study the levels of hypoxemia and serum electrolytes like sodium and potassium in cases of acute exacerbation of COPD and to assess the significance of dyselectrolytemia, as a prognostic marker in these patients.
Materials and methods
The study was undertaken from November 2014 to October 2016 among the patients attending, Victoria hospital and Bowring and Lady Curzon hospital attached to Bangalore Medical College and Research Institute, Bangalore, Karnataka, India, with acute exacerbation of COPD diagnosed clinically and by the pulmonary function tests.
50 patients with acute exacerbation of COPD and 50 stable COPD patients without acute exacerbation (controls) were included in the study. After obtaining a written and informed consent, detailed history including chief complaints, past history, treatment history, personnel history including smoking history was taken, general physical examination and respiratory system examination was done and recorded in a proforma. Arterial blood gas analysis, levels of sodium, potassium and appropriate haematological investigations was done for each patient and control. Control group was selected based on past history and previously documented diagnosis of COPD but are stable on OPD follow up.
Descriptive and inferential analysis has been carried out in the present study. Results on continuous measurements given by mean ± SD and results on categorical measurements in percentage (n). Significance assessed at 5 % level of significance.
Chi-square/ Fisher exact test has been used to find the significance of study parameters.
Results
Mean age of the cases was 61.88±10.71 and controls was 60.10±10.77.98% (n=49) of patients among the cases were males and 90%(n=45) among controls were males. On evaluating the symptoms, mean cough duration was 8.60±6.74 years and mean duration of breathlessness was 3.38±2.33 years. 10% (n=05) patients had fever. Features of right heart failure was seen in 10% (n=5) of the cases.
Oral medicines in the form of steroids or bronchodialators was taken by 14% (n=07) of the cases and 20% (n=10) of the controls. Inhalational steroids or bronchodialators was used by 44% (n=22) cases and 36% (n=18)of controls. Only 8% (n=02) cases and 4% (n=02) controls were on home oxygen therapy (Figure 1).
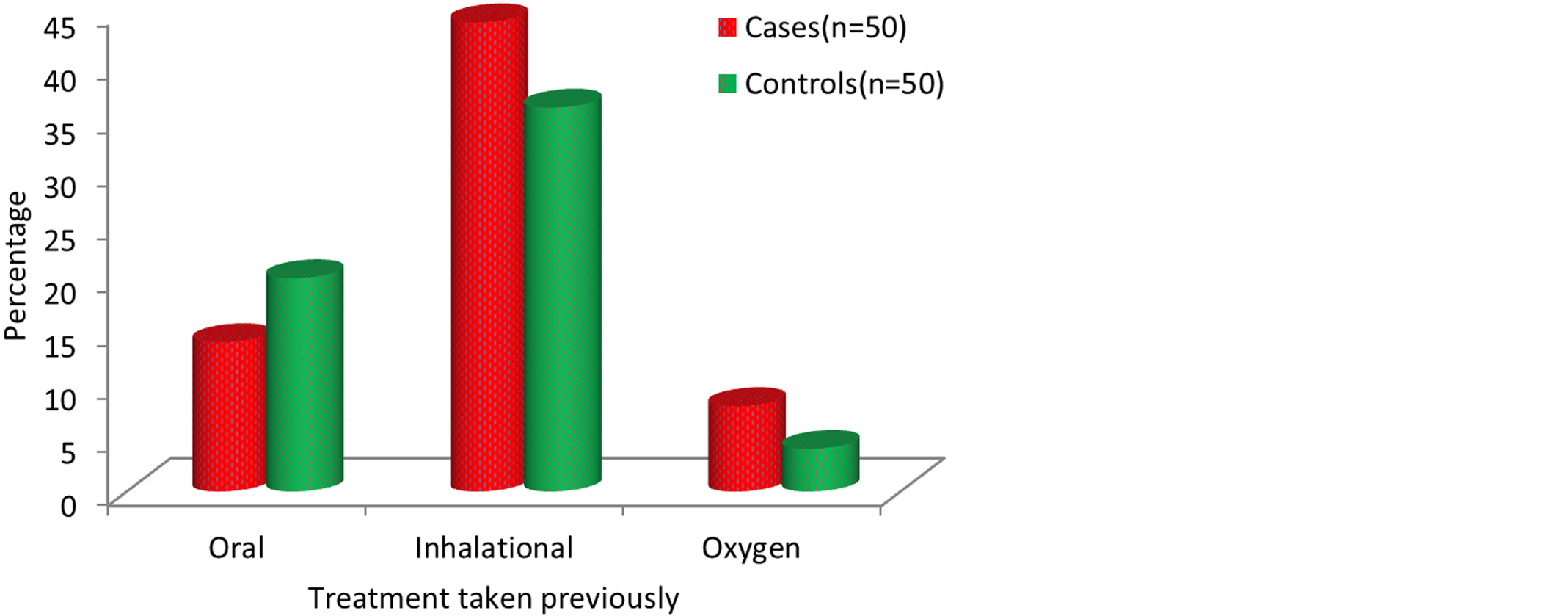
Figure 1: Type of treatment being taken.
Table 1: Comparison of clinical variables in two groups of patients studied.
|
Variables
|
Cases
|
Controls
|
P value
|
|
Hemoglobin (g/dl)
|
13.66±1.87
|
13.28±1.92
|
0.313
|
|
Total count
|
10314.80±2716.27
|
8238.40±2539.98
|
<0.001**
|
|
Platelet count
|
2.90±0.75
|
2.48±0.83
|
0.011*
|
|
Serum urea (mg/dl)
|
32.74±14.73
|
32.23±12.53
|
0.852
|
|
Serum creatinine (mg/dl)
|
0.89±0.29
|
0.80±0.26
|
0.135
|
|
RBS
|
109.78±21.09
|
117.80±27.51
|
0.105
|
|
Serum sodium (mEq/l)
|
132.70±5.37
|
136.18±4.00
|
<0.001**
|
|
Serum potassium (mEq/l)
|
3.54±0.64
|
3.86±0.59
|
0.010**
|
The mean values of various laboratory parameters among the cases and controls are shown in the table 1 with mean total leucocyte count and mean serum sodium and potassium levels being statistically significant between cases and controls with p<0.05.
Serum sodium levels were in normal range in 40% (n=20) of cases and 66% (n=33) of controls. Whereas serum sodium levels were below 135meq/L in 60% (n=30) of cases and 34% (n=17) of controls (Table 2).
Table 2: Serum sodium (mEq/l) distribution in two groups of patients studied.
|
Serum sodium (mEq/l)
|
Cases
|
Controls
|
|
No
|
%
|
No
|
%
|
|
<130
|
16
|
32.0
|
3
|
6.0
|
|
130-135
|
14
|
28.0
|
14
|
28.0
|
|
>135
|
20
|
40.0
|
33
|
66.0
|
|
Total
|
50
|
100.0
|
50
|
100.0
|
Similarly serum potassium levels were in the normal range in 44% (N=22) of the cases and 76% (n=38) of controls and serum potassium levels were below 3.5 meq/L in 56% (n=28) of cases and 24% (n=12) controls (Table 3).
Table 3: Serum potassium (mEq/l) distribution in two groups of patients studied.
|
Serum Potassium (mEq/l)
|
Cases
|
Controls
|
|
No
|
%
|
No
|
%
|
|
<3.5
|
28
|
56.0
|
12
|
24.0
|
|
>3.5
|
22
|
44.0
|
38
|
76.0
|
|
Total
|
50
|
100.0
|
50
|
100.0
|
Pulmonary function test was done in 76% (n=38) cases and 100% (n=50) controls and 54% (n=27) and 16% (n=08) among cases and controls respectively showed moderate obstruction and 22% (n=11) in each study group showed severe obstruction.
Arterial blood gas analysis showed respiratory acidosis in 54% (n=27) of the cases.40% (n=20) patients improved with ventilator support and 6% (n=30) showed improvement in symptoms without need of ventilator and two patients died during the course both of whom required ventilator support.
Table 4: Outcome in of patients.
|
Outcome
|
No. of patients
(n=50)
|
%
|
|
Improved with ventilatory support
|
20
|
40.0
|
|
Improved without ventilatory support
|
30
|
60.0
|
|
Death
|
2
|
4.0
|
Further on correlating their serum sodium levels, 8 patients (40%) among the cases having serum sodium levels below 135meq/L required ventilator support which was statistically significant with p<0.05. Similarly 17 patients (34%) among the cases having serum potassium levels below 3.5meq/L required ventilator support which was also statistically significant at p<0.05.
Discussion
In our study age distribution varied between 40 to 80 years with mean age group of 61.88 ±10.77among cases and 60.10±10.71 among controls. The mean age in a study done by Das et al. [2] was similar to our study 62.22±12.45 years.
Males constituted 98% (n=49) of the cases and 90% (n=45) of controls in our study. In study by Das et al. [2] male to female ratio was 2.6:1 among cases and 3:1 among controls. In our study the most common presentation in acute exacerbation was cough, fever and breathlessness.
The mean pack years among our study population was 20±10.5 pack years, similar to a study by Mohan et al. [14] where the mean pack years was 22.3±11.2 pack years.
Majority of our patients i.e. 44% (n=22) of cases and 36% (n=18) of controls were on inhalational steroids and bronchodialators and 4 patients among cases and 2 patients among controls were on home based oxygen therapy.
Mean serum sodium was 127±5 meq/L among cases and 133±6 meq/L among controls, with 28% (n=14) cases and 6% (n=03) controls having hyponatremia with serum sodium levels below 135meq/L. In a study by Das et al. [2] mean serum sodium was 133±6meq/L among cases and 142±2.28 meq/L among controls.
In our study mean serum potassium levels were 2.8±1.2meq/L among cases and 3.5±2.2 meq/L among controls. And 56% of cases had serum potassium below 3.5meq/L. In a study by Mohan et al. [14], hypokalemia with serum potassium levels below 3.5meq/L was seen in 16.4% of their study group. In another study by Das et al. [2] serum potassium levels were 3.39± 0.96 meq/L almond patients with acute exacerbation of COPD.
In this study pulmonary function test showed 54% of cases (n=27) and 62% (n=31) controls showed moderate obstruction and 22% (n=11) in each group had severe obstruction.
In our study 54% (n=27) patients had respiratory acidosis on ABG analysis, similar to a study done by Vijay et al. [15], where 33% (n=20) patients had respiratory acidosis.
On studying outcomes, 40% (n=20) of our cases needed ventilator support (invasive and non-invasive support) and 60% (n=30) of the cases showed improvement in their symptoms without ventilator support and two patients among those who were on ventilator support died during the course.
Further on correlating their serum sodium levels, 8 patients (40%) among the cases having serum sodium levels below 130meq/L required ventilator support which was statistically significant with p<0.05. Similarly 17 patients (34%) among the cases having serum potassium levels below 3 meq/L required ventilator support which was also statistically significant at p<0.05.This was similar to a study done by Rabinovitz et al. [16] where hyponatremia was significantly associated with increased rate of mortality with hazard ratio of 1.82. In another study by Celli et al. [17], concluded that water retention and hyponatremia was associated with final stages of COPD and that onset of hyponatremia was a poor prognostic factor.
Conclusion
Electrolyte abnormalities are most commonly seen in patients with chronic obstructive pulmonary disease (COPD) with acute exacerbation and carry very poor prognosis in this group of patients. Thus, overlooking of coexistent metabolic abnormalities may contribute to a great deal of mortality and morbidity in COPD patients during their acute exacerbation episodes.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] John JR, EdwinKS, COPD, Harrison’s principles of internal medicine, 18th edition. New York: McGraw- Hill; 2012; pp.2151–2160.
[2] Das P, Bandyopadhyay M, Baral K, Paul R, Banerjee AK. Dyselectrolytemia in chronic obstructive pulmonary diseases with acute exacerbations. Nig J Physiol Sci. 2010; 25(1):25–27.
[3] Dransfield MT, Kunisaki KM, Strand M, Anzueto A, Bhatt SP, et al. acute exacerbations and lung function loss in smokers with and without chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017; 195(3):324–330.
[4] Wedzicha JA, Banerji D, Chapman KR, Vestbo J, Roche N, et al. Indacaterol-glycopyrronium versus salmeterol-fluticasone for COPD. N Engl J Med. 2016; 374(23):2222–2234.
[5] Tsiligianni IG, Kosmas E, Van der Molen T, Tzanakis N. Managing comorbidity in COPD: a difficult task. Curr Drug Targets. 2013; 14(2):158–176.
[6] Rashid MDH. Electrolyte disturbances in acute exacerbation of COPD. J Enam Med Col. 2019; 9(1):25–29.
[7] Hurst JR, Vestbo J, Anzueto A, Locantore N, Müllerova H, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010; 363(12):1128–1138.
[8] Acharya CP, Paudel K. Serum electrolyte in acute exacerbation of chronic obstructive pulmonary disease. JGMC Nepal. 2020; 13(1):9–13.
[9] McKeever TM, Hearson G, Housley G, Reynolds C, Kinnear W, et al. Using venous blood gas analysis in the assessment of COPD exacerbations: a prospective cohort study. Thorax. 2016; 71:210–215.
[10] Suri P, Habeeb K, Alai MS, Rather HA, Jalal S. Hyponatremia presenting as cardiac conduction defect. J K Science.2009; 11(2):85–86.
[11] Vijayan VK. Chronic obstructive pulmonary diseases. Indian J Med Res. 2013; 137:251–269.
[12] Bollmeier SG, Hartmann AP. Management of chronic obstructive pulmonary disease: A review focusing on exacerbations. Amer J Heal-Syst Pharm. 2020; 77(4):259–268.
[13] Yang CT, Lin HC, Lin MC, Wang CH, Lee CH, et al. Effect of beta 2-adrenoceptor agonists on plasma potassium and cardiopulmonary responses on exercise in patients with chronic obstructive pulmonary disease. Eur J ClinPharmacol. 1996; 49(5):341–346.
[14] Mohan A, Premanand R, Reddy LN, Rao MH, Sharma SK, et al. Clinical presentation and predictors of outcome in patients with severe acute exacerbation of chronic obstructive pulmonary disease requiring admission to intensive care unit. BMC Pulm Med. 2006; 6:27–30.
[15] Vijay S, Bhargava AK, Sharma M, Gupta D. Arterial blood gas analysis in chronic obstructive pulmonary disease. Ind J Appl Res. 2015; 5(12).
[16] Rabinovitz A, Raiszadeh F, Zolty R. Association of hyponatremia and outcomes in pulmonary hypertension. J Card Fail. 2013; 19(8):550–556.
[17] Celli BR, Wedzicha JA. Update on clinical aspects of chronic obstructive pulmonary disease. N Engl J Med. 2019; 381:1257–1266.