Case Report
2016
March
Volume : 4
Issue : 1
Blount’s disease: A case report
Krishnaiah K, Sameer Rathore, Vasil Quadri
Pdf Page Numbers :- 15-17
Krishnaiah K1,2,*, Sameer Rathore1 and Vasil Quadri1
1Department of Orthopaedics, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India
2KIMS Foundation and Research Centre, Minister Road, Secunderabad - 500003, Telangana, India
*Corresponding author: Dr. K. Krishnaiah, M.S., M.C.h (Ortho), FRCS, Department of Orthopaedics, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India. Email: krishnaiah_k@hotmail.com
Received 20 October 2015; Revised 8 December 2015; Accepted 22 December 2015; Published 29 December 2015
Citation: Krishnaiah K, Rathore S, Quadri V. Blount’s disease: A case report. J Med Sci Res. 2016; 4(1):15-17. DOI: http://dx.doi.org/10.17727/JMSR.2016/4-005
Copyright: © 2016 Krishnaiah K, et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Blount’s disease is defined as a growth disorder of medial aspect of proximal tibia physis with abrupt medial angulation of proximal tibia distal to epiphysis, leading to varus angulation of proximal tibia and medial rotation of tibia. Epidemiology is not well established and very rarely cases have been reported from Indian subcontinent.
Presentation of case: A 3-years-old female child presented with deformity in both the legs and altered walking pattern for the past one year. On examination there was 15 degrees of varus deformity in both the knees. There was 25 degrees of internal tibial torsion bilaterally. The child was managed by surgical intervention. Oblique proximal tibial osteotomy was done. Fixation was done with a single cancellous screw on both sides and immobilisation was done in above knee plaster cast. Child recovered well with correction of deformity and could walk with normal gait pattern.
Discussion: The cause of Blount’s disease is still not well established. Treatment depends upon age at presentation, severity of varus deformity as determined by Langenskiold staging, and progression of the disease. Early intervention is required to avoid progression of the disease and permanent deformity.
Conclusion: Blount’s disease is a very rarely encountered condition in Indian subcontinent but has a characteristic presentation. It should be included in differential diagnosis in cases presenting with pathological bowing of legs. Radiological findings and normal blood biochemistry can guide us towards the diagnosis of Blount’s disease.
Keywords: Blount’s disease; Indian subcontinent; bilateral Blount’s disease, infantile Blount’s disease
Full Text
Blount’s disease is defined as a growth disorder of medial aspect of proximal tibial physis with abrupt medial angulation of proximal tibia distal to epiphysis, leading to varus angulation of proximal tibia and medial rotation of tibia [1, 2]. There are three types of Blount’s disease: (a) Infantile- Early onset below 4 years of age; (b) Juvenile- Late onset after 4 years of age (4 years-10 years); (c) Adolescent- Late onset after 10 years of age [3]. Pathology lies in the disordered endochondral ossification of medial part of proximal tibial physis. It is bilateral in 60% of cases [4]. Clinically the child presents with bowing and limb length discrepancy of lower limbs, non-tender bony protuberance on the medial aspect of proximal tibia and sometimes pain. Epidemiology of Blount’s disease is not well documented. Predisposition to Blount’s disease has been attributed to race, genetics, age at walking and obesity. Blount’s disease has increased prevalence in Afro-American and Scandinavian paediatric populations. Incidence in Indian subcontinent is not well documented. In this case report we wish to report a case of infantile bilateral Blount’s disease in a 3-year-old Indian girl.
Presentation of case
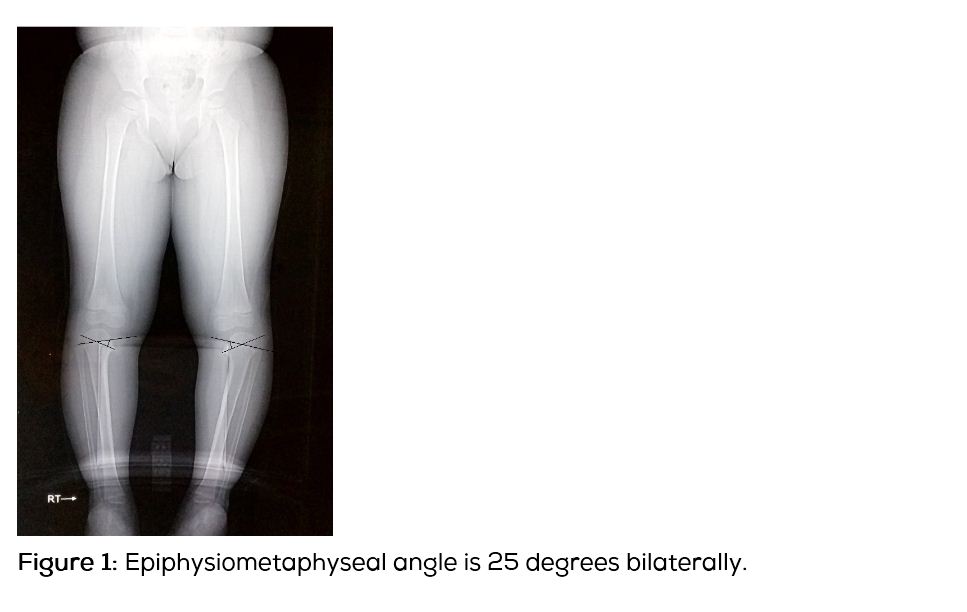
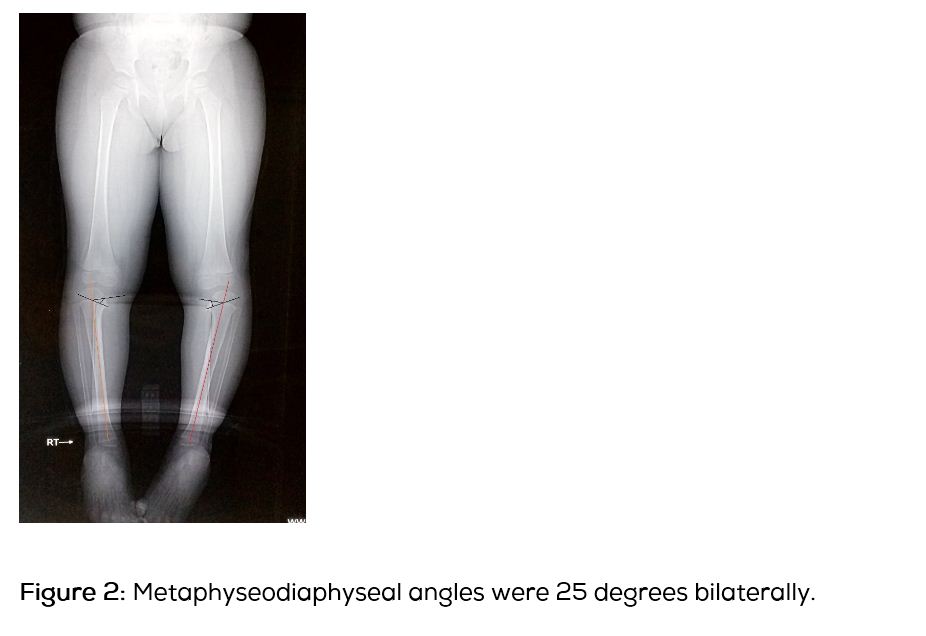
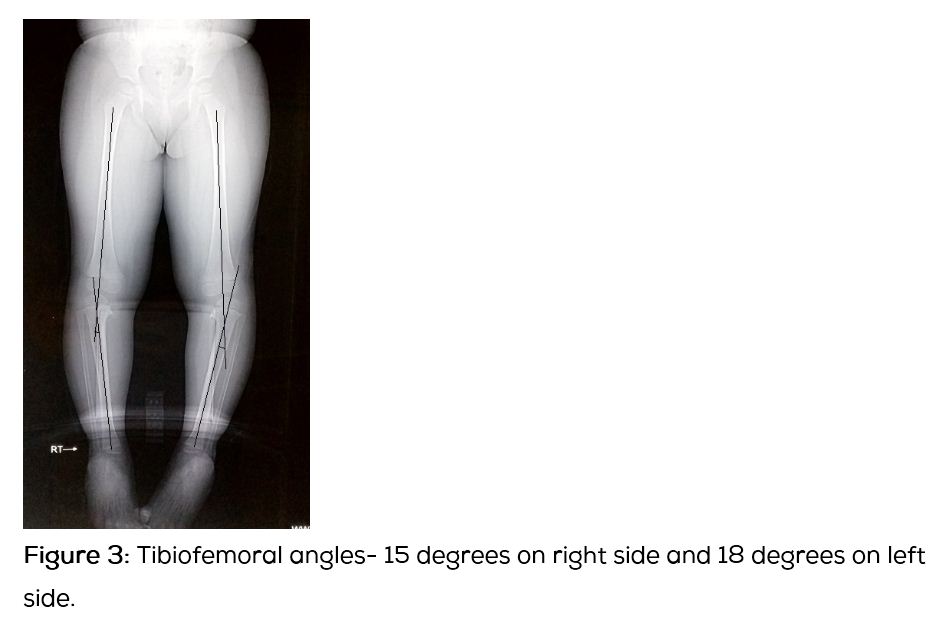
A 3-years-old female child presented with deformity in both the legs and altered walking pattern for the past one year. The child had started to walk since 1 year of age. There was no history suggestive of trauma or osteomyelitis. There was no relevant family history. On examination there was 15 degrees of varus deformity in both the knees. There was 25 degrees of internal tibial torsion bilaterally. Knee range of motion was from 10 degree of hyperextension to 140 degrees of full flexion. There was no tenderness around the knee and no ligamentous laxity. Knee joints were in contact with each other in standing position. On a scanogram, the epiphysiometaphyseal angle was 25 degrees (Figure 1), metaphyseodiaphyseal 15 degrees (Figure 2), tibiofemoral angle being angle was 15 degrees on the right side and 8 degrees on the left (Figure 3). Haematological investigations (Serum calcium, Vitamin D, Alkaline phosphatase, ESR) were within normal limits.
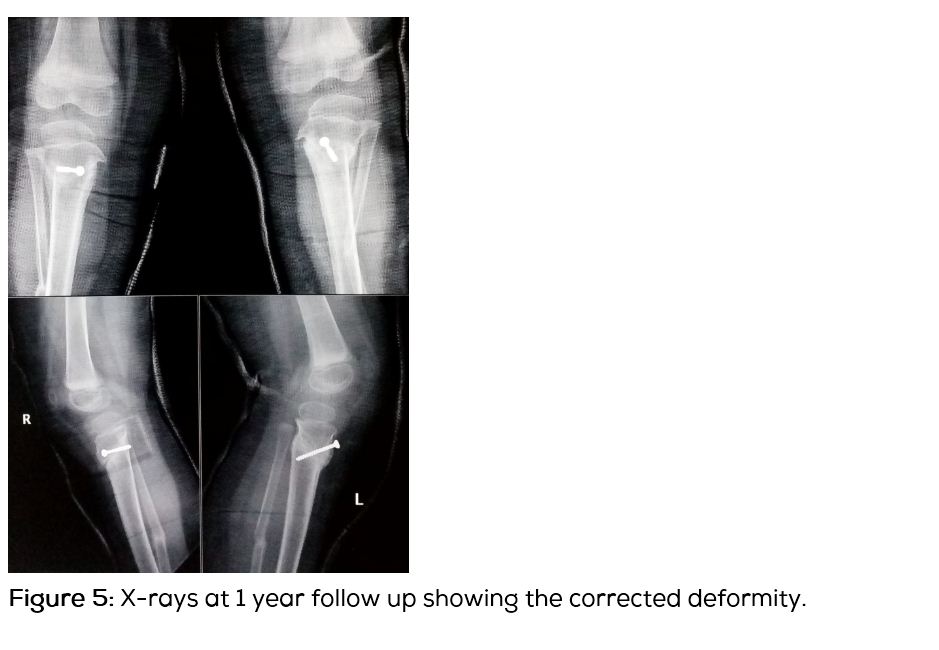
Diagnosis of Blount’s disease was made on the basis of the clinical and radiological findings. Radiologically the disease fits in Langenskiold stage 3. The patient’s age being 3 years at the time of presentation, appropriate treatment would be proximal tibial osteotomy [5]. Patient was operated for bilateral proximal tibia oblique osteotomy (Figure 4). Osteotomy was stabilised with a cancellous screw and above knee plaster cast was applied for 6 weeks. Osteotomy showed good union by the end of 2 months. Clinically the deformities were corrected (Figure 5) and child started walking with normal gait pattern.

Discussion
Bowing of leg is a common problem in a child. It may be physiological or pathological. Physiologic bowing will improve without treatment as the child grows, while pathologic bowing will tend to worsen over time without treatment. So it is very important for the clinician to identify whether the bowing is physiological or pathological. A common diagnosis in such cases is rickets. In cases with normal serum biochemistry and indicative radiological findings, diagnosis of Blount’s disease should also be kept in mind. Early diagnosis and treatment of Blount’s disease is vital to avoid progressive worsening. In infantile Blount disease, radiograph of lower limb demonstrates bowing and abrupt medial angulation, “beaking” of the medial cortical wall of the proximal tibial metaphysis. Lateral knee radiographs show posteriorly directed projection at the proximal tibial metaphyseal level [6, 7]. Epiphyseometaphyseal angle more than 20 degrees with metaphyseodiaphyseal angle more than 11 degrees in a child with genu varum should raise the suspicion of Blount’s disease [5].
The differential diagnosis of Blount disease includes [8, 9]:
1. Physiologic bowing - It is usually a self-limited condition, recognized by smoothly curved bowing of the femur and tibia and usually resolves by 18-24 months of age.
2. Congenital bowing - Angulation may occur in the middle portion of the tibia with a normally appearing distal femur and proximal tibia.
3. Rickets - Typical radiological features like fraying, splaying and cupping at the metaphyseal end with biochemical abnormalities (which were normal in our case).
4. Osteomyelitis - Growth plate disturbance occurs secondary to infection.
5. Metaphyseal chondrodysplasia - Metaphyseal deformities are seen with rickets occurrence radiological changes without serum biochemical abnormalities.
6. Ollier’s disease - It is differentiated easily from Blount’s disease on radiographs by the presence of multiple enchondromas.
Treatment depends upon age at presentation, severity of varus deformity as determined by Langenskiold staging, and progression of the disease. Problems to be managed are deformity – varus, procurvatum and internal torsion, joint depression, physeal bar, limb length discrepancy and chances of recurrence. The options for treatment are careful observation and follow up, orthotic treatment and surgical correction.
Conclusion
Blount’s disease is commonly seen in African-American lineage and rarely, cases are reported from other parts of world. The usual diagnosis in such cases is rickets but Blount’s disease should also be kept in mind during the evaluation of the patients with similar clinical presentation and normal blood investigations.
Acknowledgements
Acknowledgements are due to the Departments of Radiology & Imageology, Krishna Institute of Medical Sciences (KIMS), Secunderabad.
Conflicts of interest
Authors declare no conflict of interest.
References
1. Blount WP. Tibia vara: osteochondrosis deformans tibiae. J Bone Joint Surg. 1937; 19(1):1–29.
2. Greene WB. Infantile tibia vara. J Bone Joint Surg Am. 1993; 75(1):130–143.
3. Langenskiold A. Tibia vara. A critical review. Clin Orthop Relat Res. 1989; 246:195-207.
4. Hoffman A. Blount’s disease after skeletal maturity. J Bone Joint Surg Am. 1982; 64(7):1004–1009.
5. Joseph B, Nayagam S, Loder RT, Torode I. Paediatric orthopaedics: A system of decision making. Hodder Arnold. 2009.
6. Loder RT, Johnston CE 2nd. Infantile tibia vara. J Ped Orthop. 1987; 7(6):639–646.
7. Greene WB. Infantile tibia vara. J Bone Joint Surg Am. 1993; 75(1):130–143.
8. Silve C, Jüppner H. Ollier disease. Orphanet J Rare Dis. 2006; 1:37.
9. Jain N, Narain S, Gupta AK, Nag HL, Kabra SK. Blount’s disease: A lesser known cause of Bowlegs mandating early differentiation from physiological bowing. Indian J Pediatr. 2002; 69(2):189–191.