Short Communications
2013
March
Volume : 1
Issue : 1
Breast cancer screening and impalpable breast cancers –Our experience
Jwala Srikala M
Pdf Page Numbers :- 40-44
Jwala Srikala M1,*
1Department of radiology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad - 500003, AP, India
*Corresponding author: Dr. M. Jwala Srikala, MD, MRD, DNB (Radiology), Consultant Radiologist, Krishna Institute of Medical Sciences, Minister Road, Secunderabad - 500003, AP, India, Tel.: +91 40 44885197; E-mail: srikalajwala@yahoo.com
Received 12 January 2012; Revised 13 February 2013; Accepted 20 February 2013
Citation: Jwala Srikala M. Breast cancer screening and impalpable breast cancers –Our experience. J Med Sci Res 2013; 1(1): 40-44. http://dx.doi.org/10.17727/JMSR.2013/1-009
Copyright: © 2013 Jwala Srikala M. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Abstract is not available for this article
Full Text
Why breast cancer screening?
Worldwide over one million women are diagnosed with breast cancer every year (10% of all new cancers). Regular mammographic screening has been proven to reduce mortality from the disease, and the reduction was 24% in eight randomizedcontrol trials (RCTs) in women over the age of 50 years invited for screening. Causes of breast cancer are not known so prevention is not an option currently.It is proven in that one in 8 women will be affected by breast cancer in their lifetime. Breast cancer rates tend to be highest in Western Europe and North America, where lifetime risk of the disease is slightly higher than 10%. In some Africancountries, the lifetime risk is only 1%. In East Asian countries, risk has been low in the past but is increasing now toward western rates. The other most important risk factor is age. The disease is almost unheard of in childhood and adolescence, and incidence gradually increases with age. Around the time of the menopause, there is a hiatus in the trend of increasing incidence, and in western populations incidence continues to increase thereafter at a slower rate. For some far eastern and other populations, incidence falls after the menopause. Early menarche, late menopause, late full term pregnancy, prolonged use of oral contraception, hormone replacement therapy are some of the known risk factors for development of breast cancer. Recently included risk factor is the BRCA positivity. BRCA 1 is localised on chromosome 17q21, BRCA 2 on 13q. If one is BRCA 1 positive there is a 50% to 73% chance of developing cancer by 50 years and 87% chance by 70 years. BRCA 2 positivity increases the risk by 45 % by age 70 years (breast cancinoma).
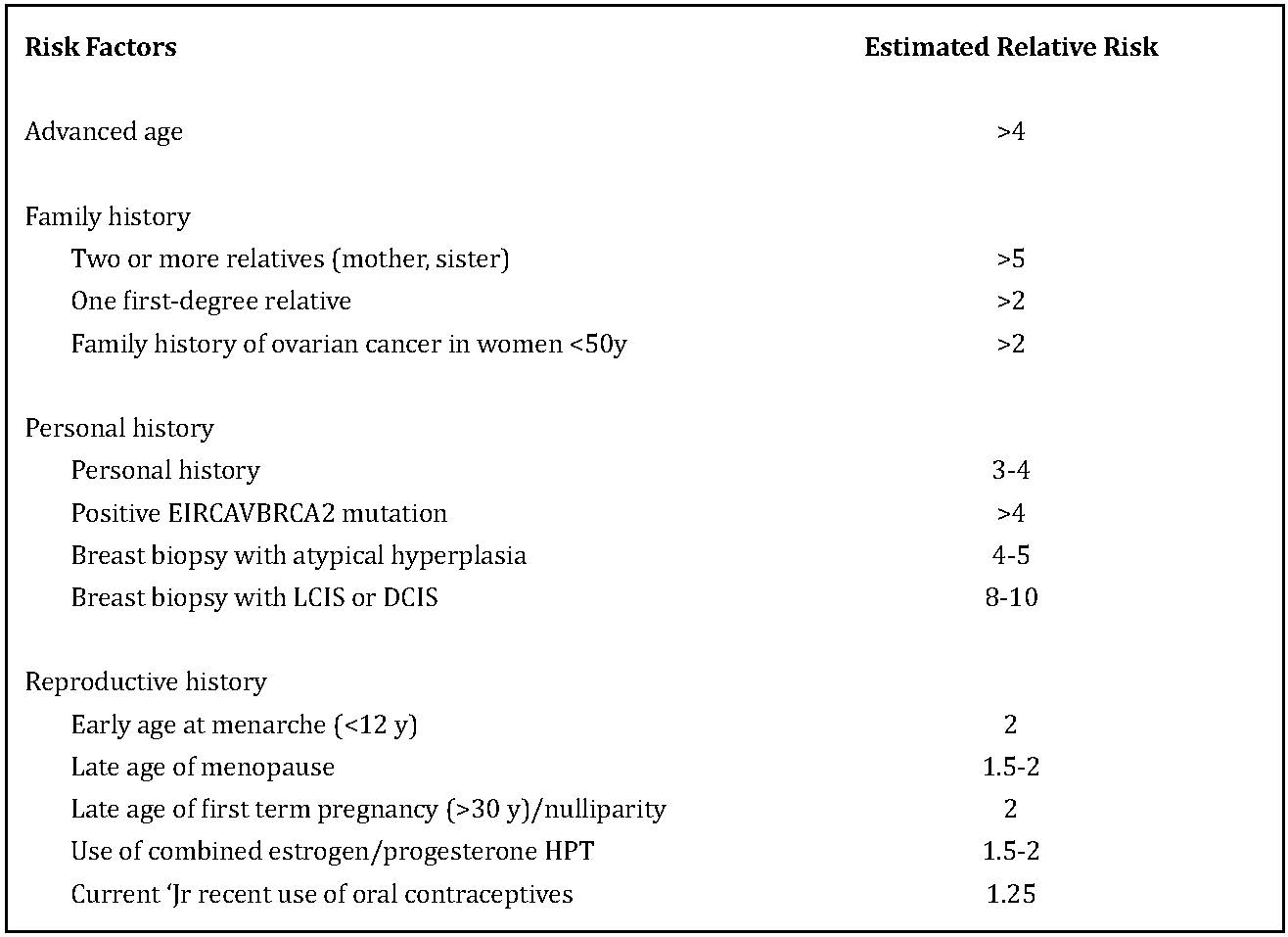
Table 1: Shows the estimated relative risk of breast cancer of some of the known risk factors.
Breast cancer screening Data from 2 county Swedish trial supports the contention that breast cancer is localised to the breast for a variable period of time before the development of systemic disease.
- Time to diagnosis is critical , earlier the better.
- Cancers less than 1 cm have a 12 yr survival rate of 95%
- Node negative breast cancers less than 1.5 cm have a 12yr survival rate of 94%.
- RCT starting at age 40 yrs have shown 20%-40% reduction in breast cancer mortality rates in screened groups compared to controls.
It is accepted that breast cancers grow more rapidly in pre-menopausal women so screening mammography every 2 yrs is recommended starting at age 40yrs. Accuracy of mammography is about 85% and is by far the best screening modality available.
Our experience
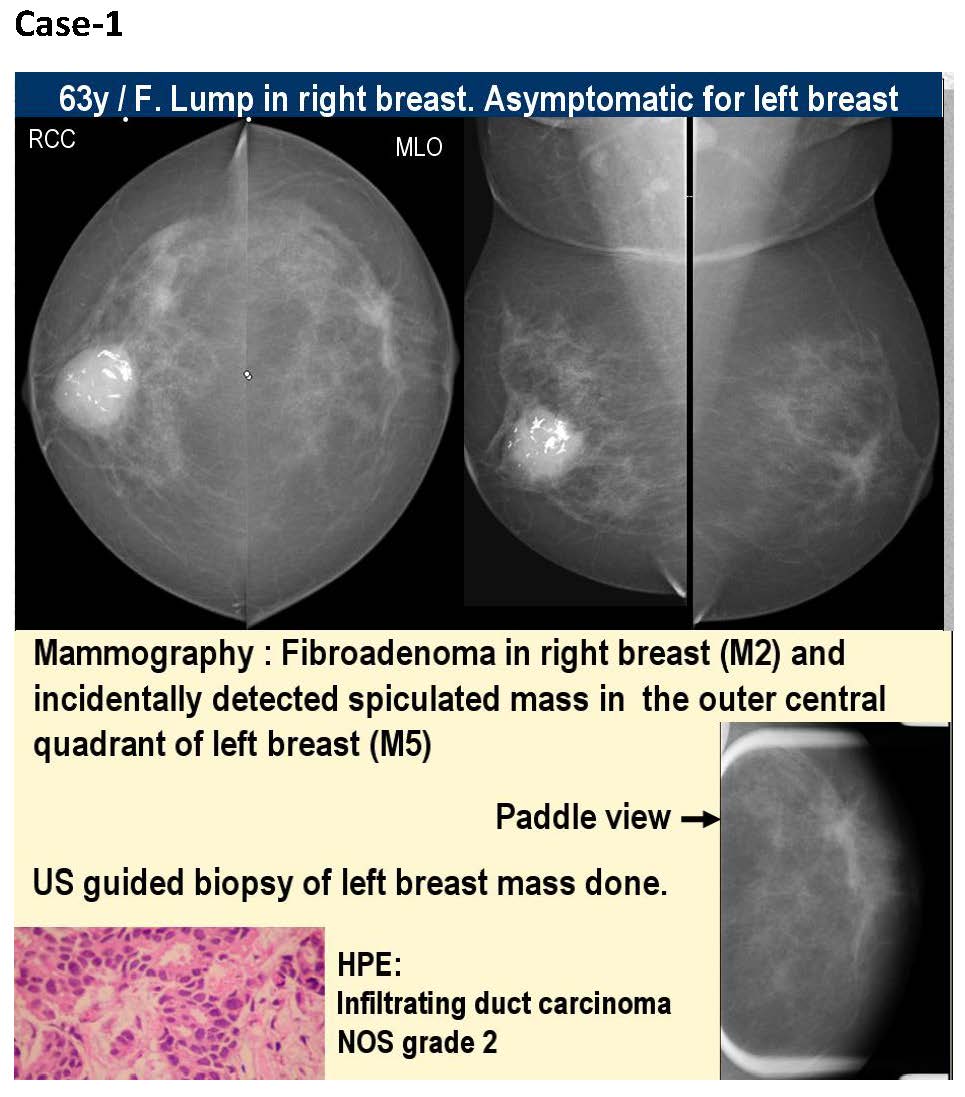
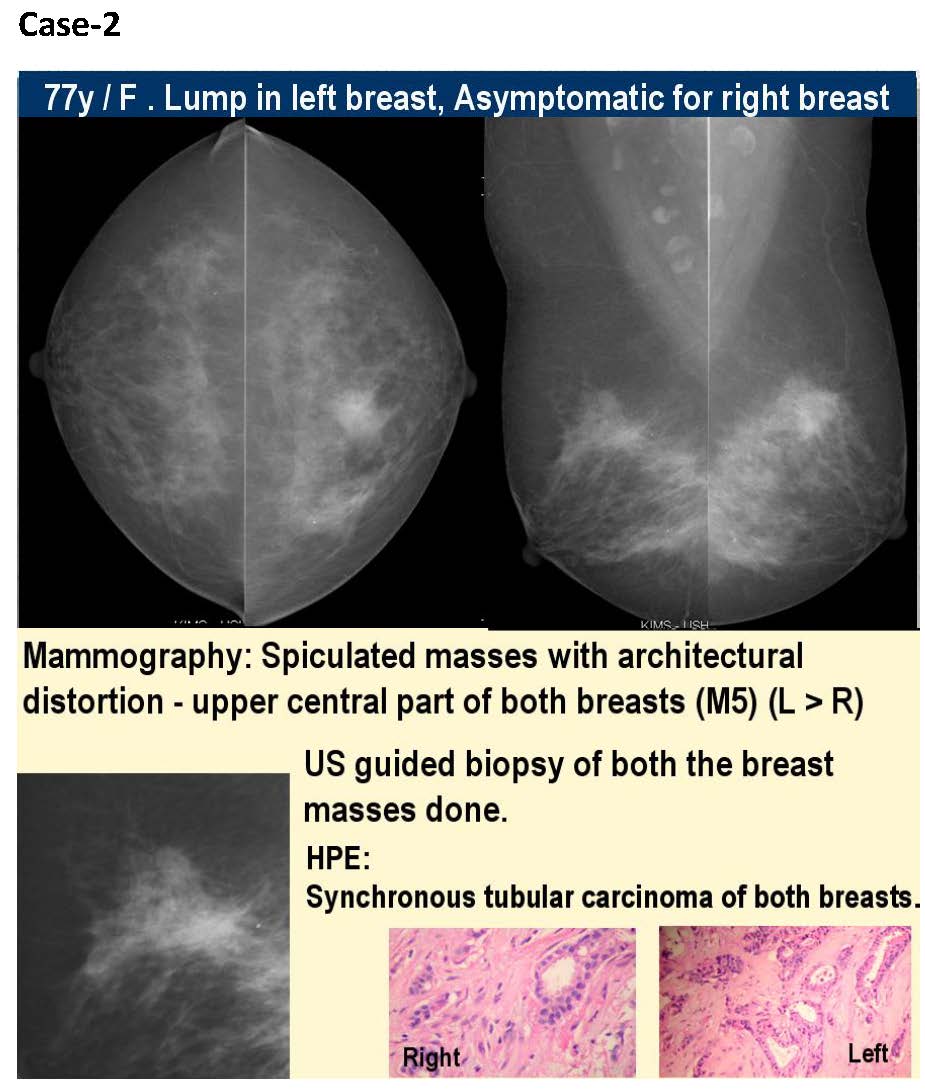
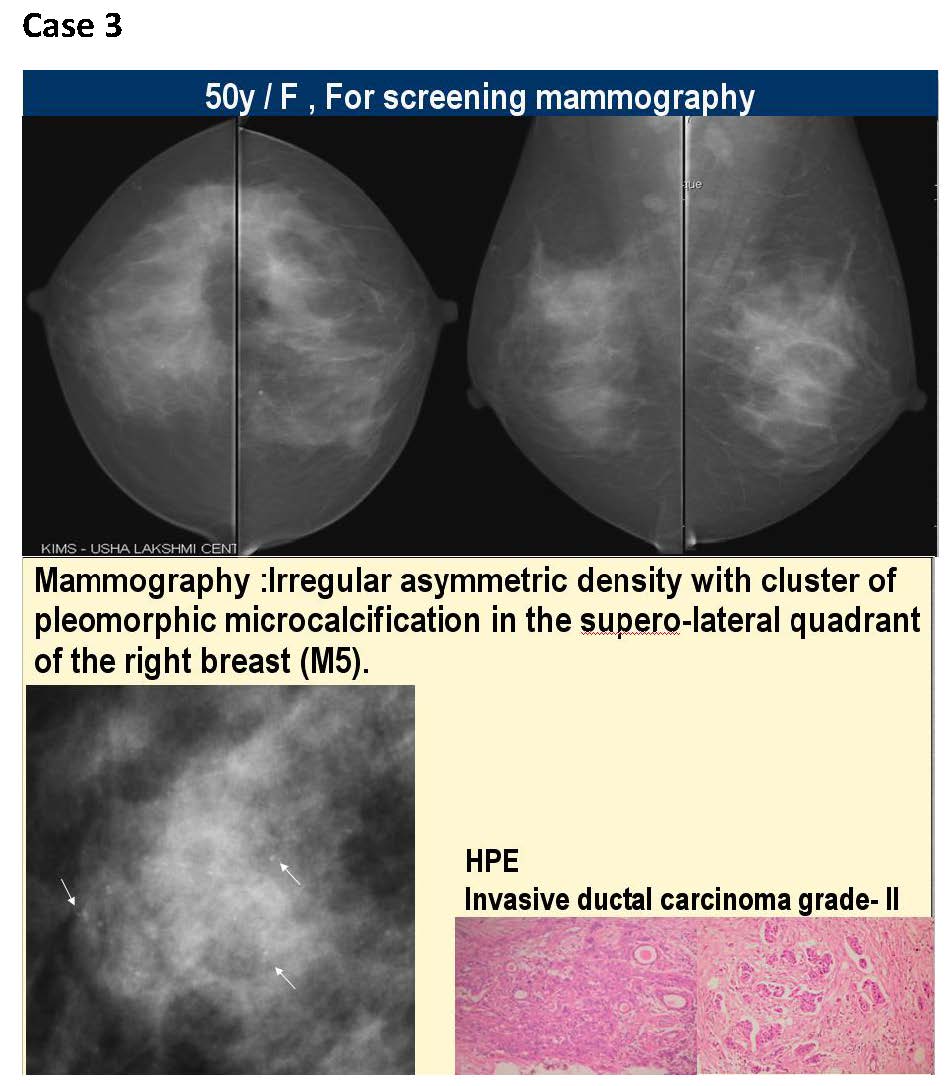
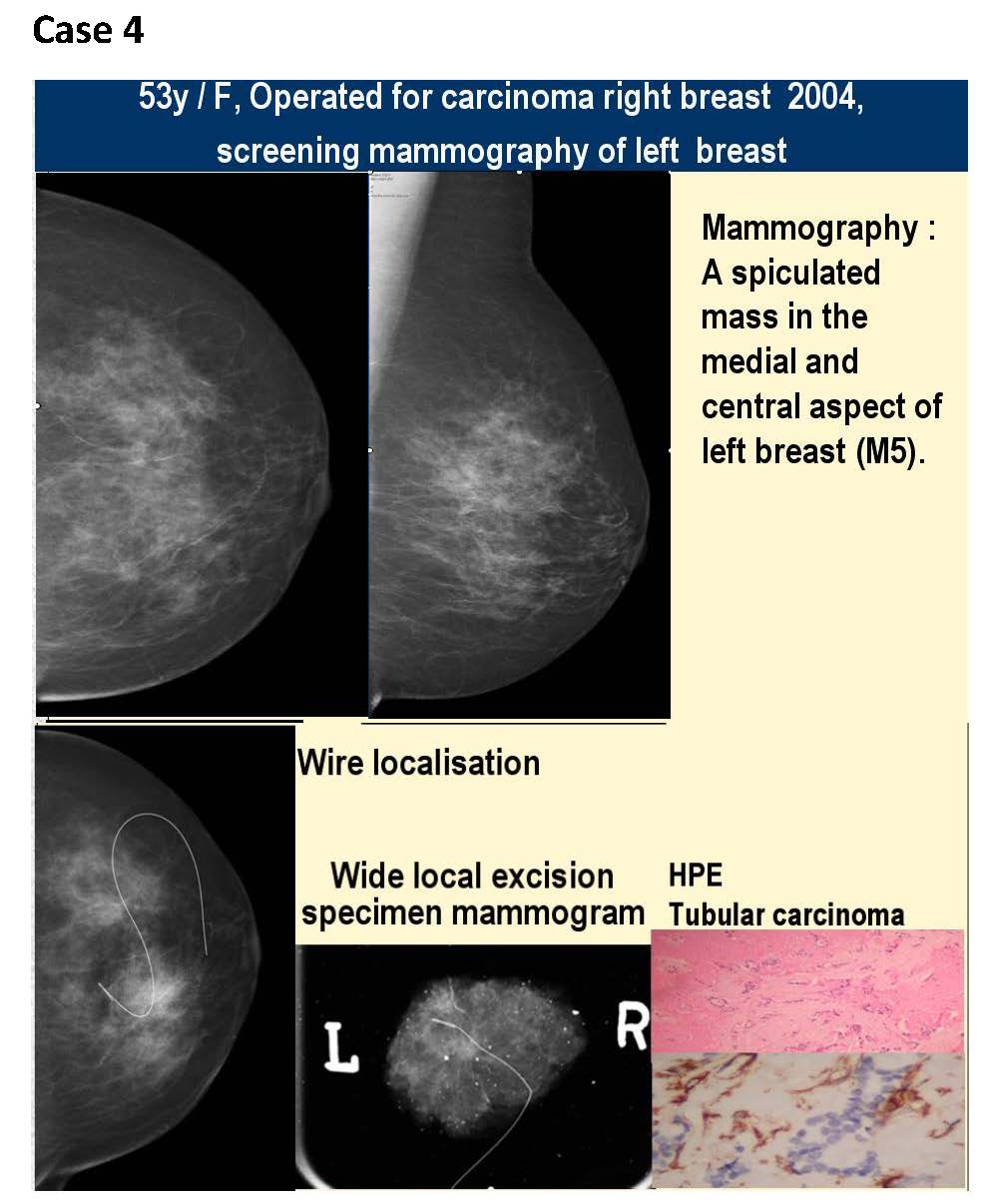
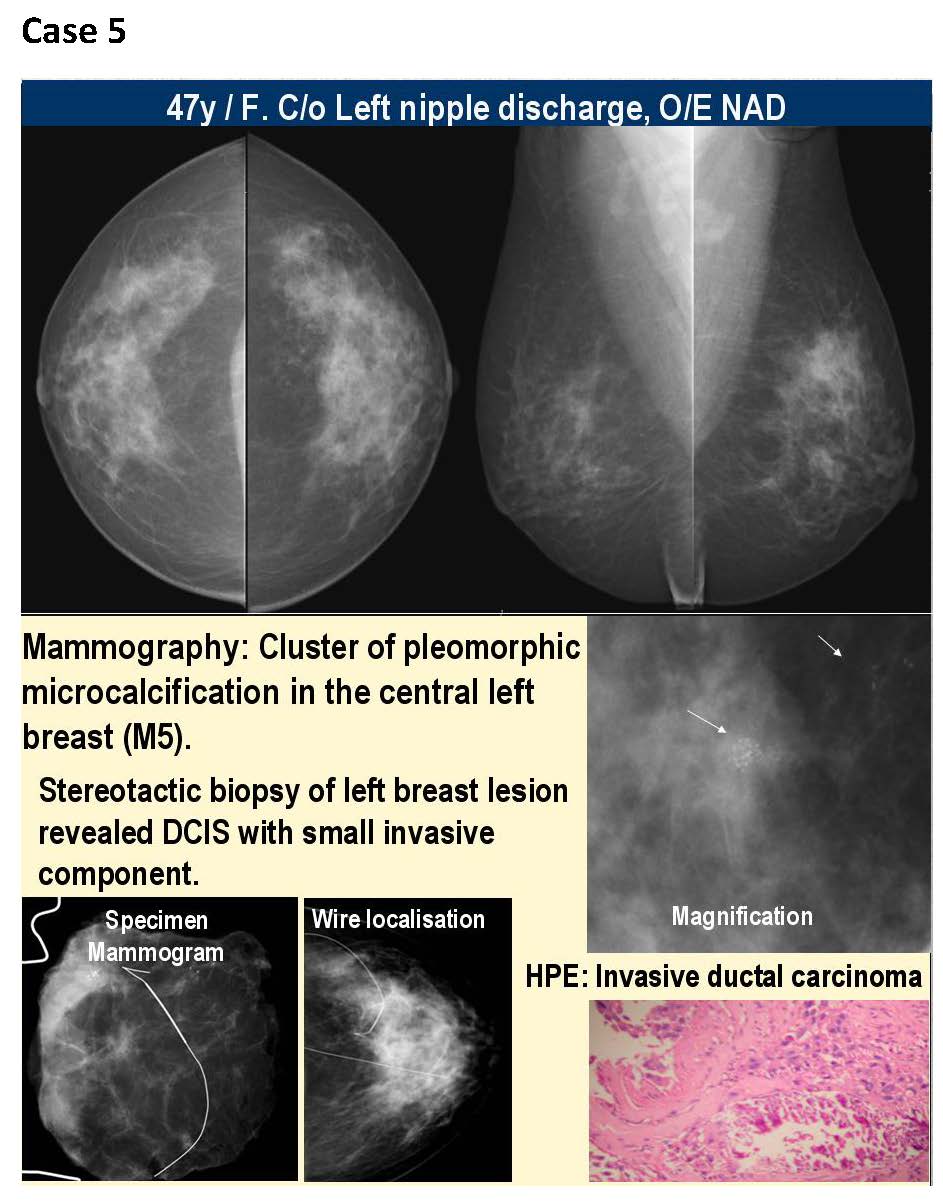
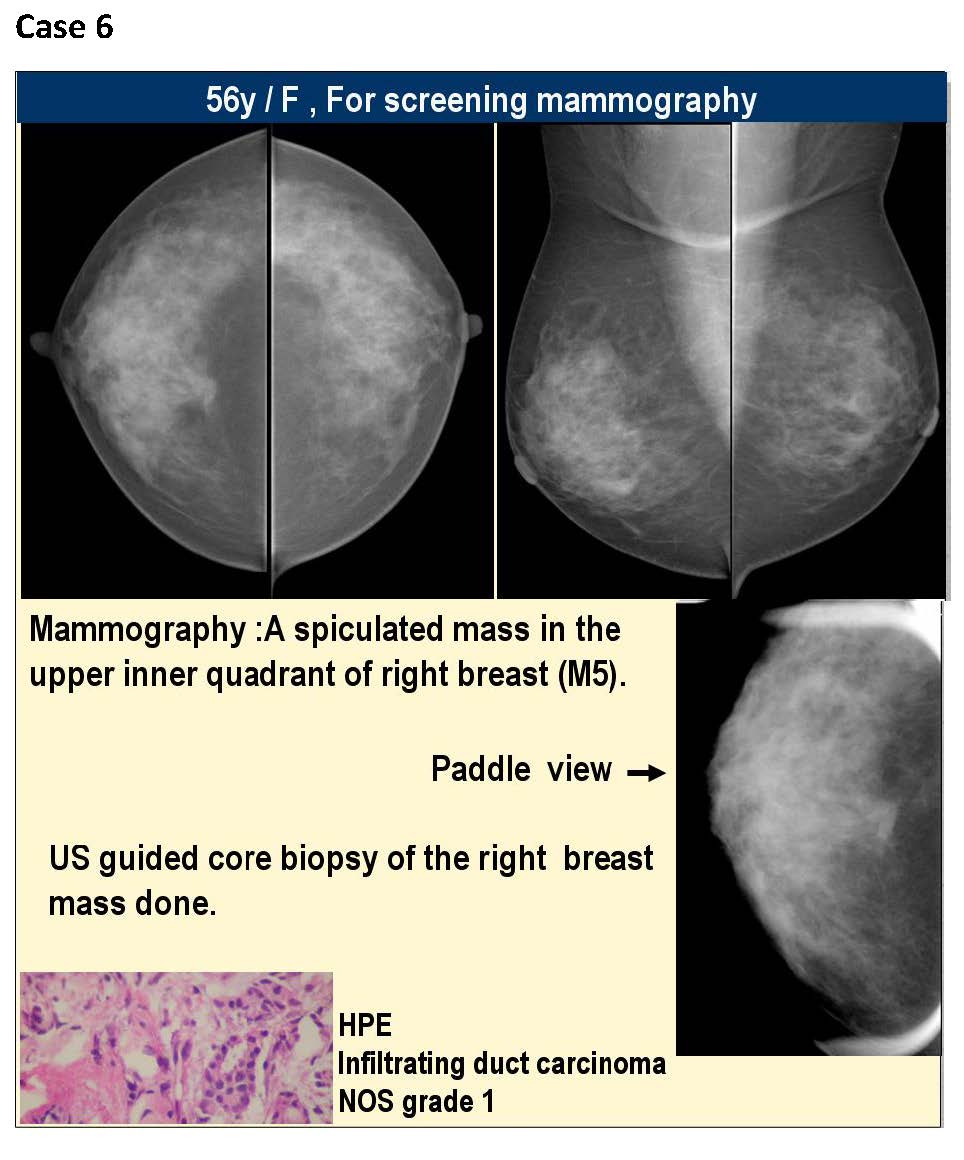
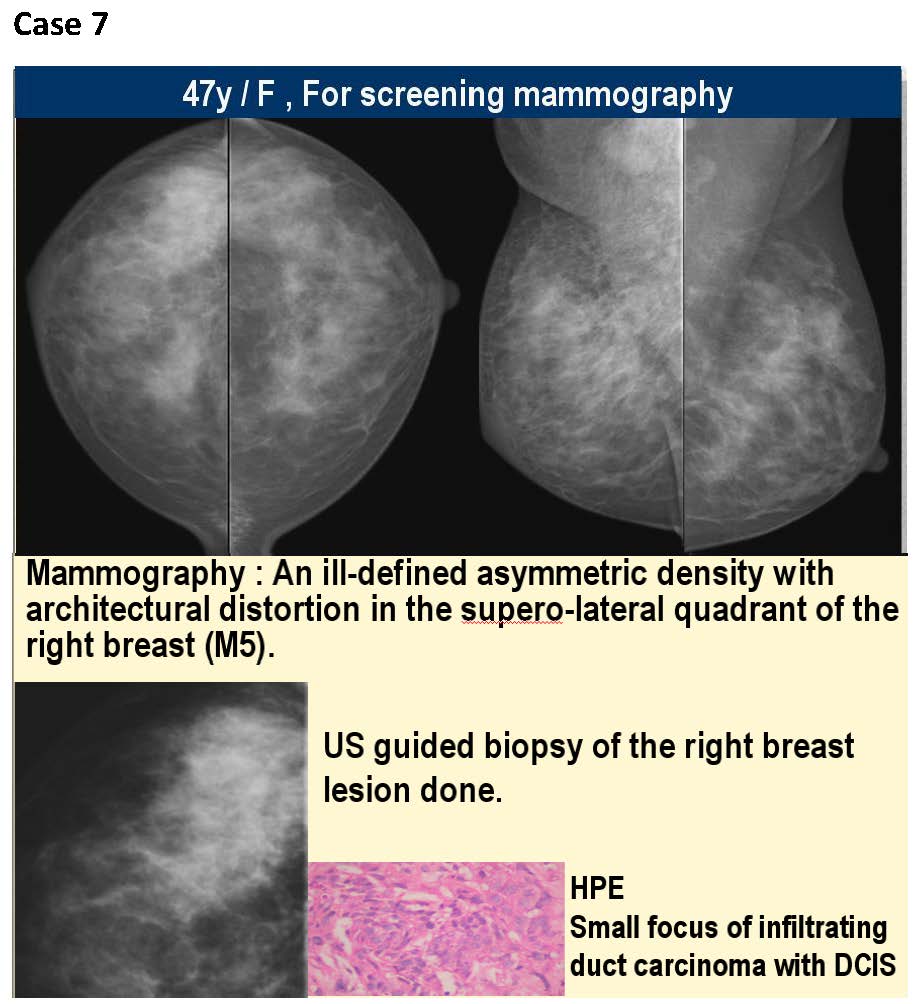
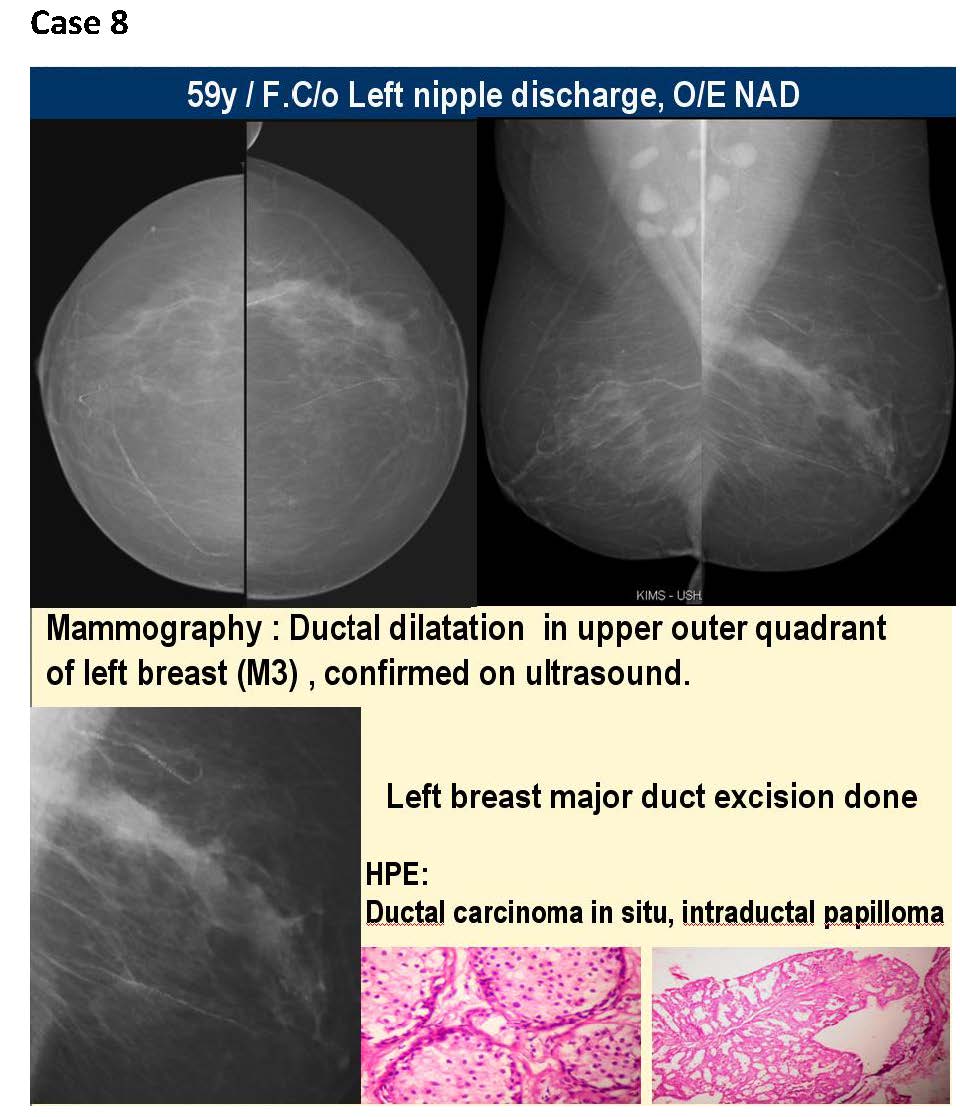
The KIMS-Ushalakshmi centre for breast disease was started in December 2007.The facility has a full-field digital mammography, the first of its kind in south India, a high end ultrasound and facility for counselling. We have performed about 11000 screening and symptomatic mammograms from December 2007 to December 2012, an average of about 2200 mammograms per year and about 42 impalpable breast cancers have been diagnosed. All these screening patients underwent digital mammography in both MLO and CC views, magnification views were taken as needed. Later they were referred for an ultrasound and depending on the findings ultrasound guided core biopsies were performed (Figure 1). Finally histopathological findings were considered as confirmatory. If the findings were of microcalcifications alone, stereotactic core biopsy was performed for confirmation of diagnosis. Further, after the diagnosis of a malignancy the patients underwent image guided wire localisation and wide local excision. The reporting system followed was as follows-
Reporting
1 Normal
2 Benign
3 Indeterminate,probably benign
4 Probably malignant
5 Malignant
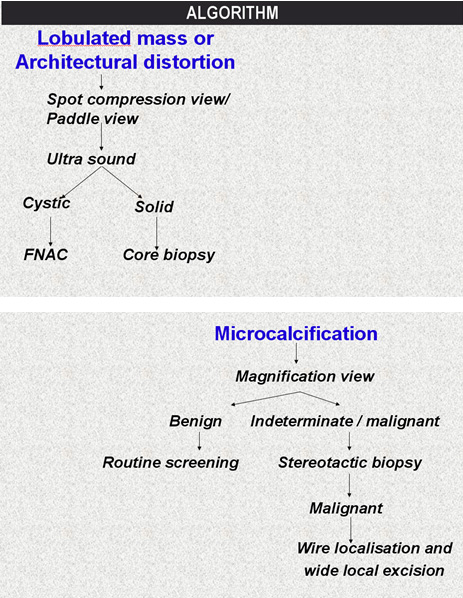
Figure 1: Algorithm for mammography detected abnormalities.
The sensitivity, specificity, and predictive values of mammography at our centre were as follows (Table 2), and have matched with several international studies.
Table 2: The sensitivity, specificity, and predictive values of mammography.
|
Sensitivity Digital mammography
|
90.4 %
|
|
|
Specificity Digital mammography
|
99 %
|
|
|
Predictive value of a positive test digital mammography
|
90.4 %
|
|
|
Predictive value of a Negative test digital mammography
|
99 %
|
|
|
Percentage of false positive digital mammography
|
09.5 %
|
|
|
Percentage of true negative digital mammography
|
0.09 %
|
|
Conclusions
Our understanding of the epidemiology of breast cancer together with our ability to influence the natural history of the disease both in individuals and in populations is almost unrecognisable compared with a few decades ago. Mammography is a highly sensitive and specific tool for detection of early breast cancer and remains the gold standard for breast cancer screening. The improvements in imaging such as the digital mammography and image guided biopsy techniques have revolutionised cancer detection and cancer care. Screening and early detection, together with improved therapy have resulted in a striking improvement in survival.
Conflicts of interest
Author declares no conflicts of interest.
References
1. Simgel K. Breast cancer death rates death rates decline for white women. I Natl Cancer Inst 1995, 87:173.
2. Peto R, Boreham J, Clarke M, et al. UK and USA breast cancer deaths down 25% in year 2000 at ages 20-69. Lancet 2000, 355: 1822.
3. Kopans DB. Beyond randomized controlled trials: organized mammographic screening substantially reduces breast cancer mortality. Cancer 2002, 94:580-581.
4. Tabar L, Vitak B, Tony HH, et al. Beyond randomized controlled trials: organized mammorgaphic screening substantially reduces breast carcinoma mortality. Cancer 2001, 91:1724-1731.
5. Tabar L, Duffy SW, Burhenne LW. New Swedish breast cancer detection results for women aged Cancer 1993, 40-49.