Full Text
Introduction
Gallbladder (GB) cancer is one of the most common bilary tract malignancies in India. According to Globocan 2020, number of new cases of gallbladder cancer in India is 19570, among all ages and sexes. It is also sixteenth common cause of death from cancer in India. According to, Globocon 2020, 5 years prevalence of gallbladder cancer patients in both the sexes is 1.82 per 100,000 populations per year, in India [1] (Table 1).
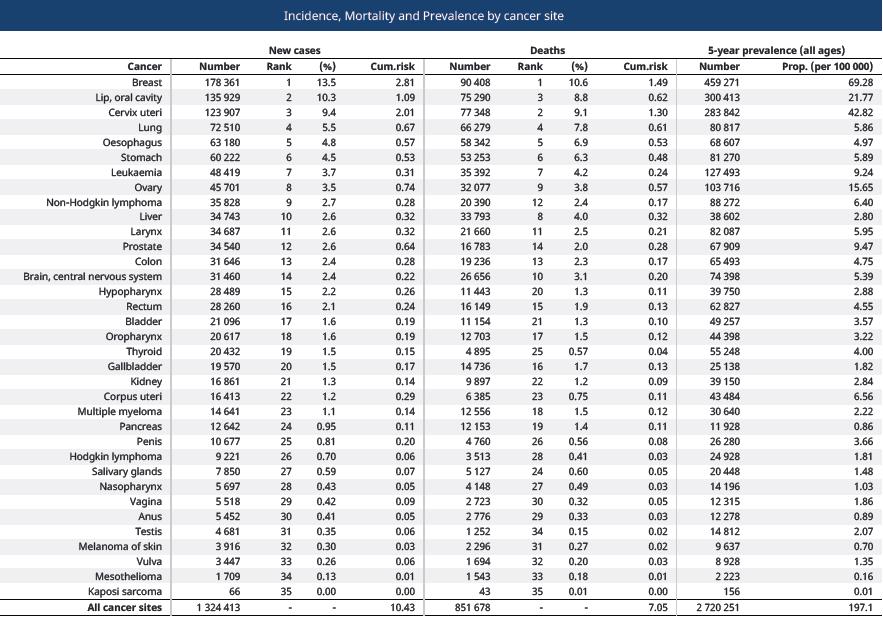
Table 1: Incidence, mortality and prevalence of gallbladder carcinoma in India, according to Globocan 2020.
Gallbladder cancer (GBC) arising from the fundus, neck or body of the GB and also manifests as diffuse thickening of the GB wall. Within India, the incidence is high in North, North-East, Central and Eastern India, and less common in South and West India [2].
The presentation is often with advanced disease and carries dismal prognosis. GBC in India usually affects younger patients in the 5th and 6th decade in contrast to the west. Gallstones are present in 80% of the Indian patients causes mucosal injury, leading to GBC. The incidence of GBC is out of proportion to the prevalence of gallstones in the country.
Additional co-factors such as old age, lower socio-economic status, chronic Salmonella typhi (S. typhi) infection, Helicobacter pylori (H. pylori) infection, exposure to pollutants, heavy metals, chemicals, and adulterated mustard oil causes gallbladder cancer. Smoking in patients with gallstones have been identified, which promotes carcinogenesis. Environmental risk factors such as soil and water contamination by industrial wastes, agricultural effluents and human sewage have been identified as risk factors [3]. GBC can be classified, on the basis of tumour site, as distal, peripheral and intra hepatic. Its clinical presentation is often non-specific resulting in significant delay in diagnosis. It is either detected incidentally at the time of cholecystectomy or when it presents with complications due to local spread of the malignancy in the form of jaundice, hepatomegaly, ascites or duodenal obstruction [4].
Rapid spread of the tumour due to its aggressive biological nature and adjoining vital structures. In India maximum number of patient diagnosed late and often unresectable at presentation, resulting in an overall dismal prognosis. Moreover, chemotherapy, radiotherapy and immunotherapy are not particularly curative. The 5-year survival rate is often <5% in most centres [5]. Also, there are no screening programs in place because it is difficult to detect early tumour since the gallbladder mucosa is not amenable to direct endoscopic inspection, in contrast to other luminal organs.
GB wall thickening of radiological features are non-specific and may consequences as chronic cholecystitis [6]. For future challenge, large multicentric comprehensive studies are required in India to identify the attributable risk of each of the identified risk factors at early stage.
Material and methods
Before initiation of the study a formal approval letter from institutional ethics committee was obtained. As this was a single institutional retrospective study, the data was collected from the institutional cancer registry from June 2019 to December 2020. Mainly diagnosis was done by ultrasonography followed by MRCP and histopathology. Sample size was 108 patients. The study was approved by the IEC.
Method of data collection
Pre-treatment data were collected in case-record form with history, physical examination, detailed clinical examination and radiological assessment and laboratory investigations.
Definition of population
Patients suffering from histologically proved carcinoma, attending the outpatient department, Department of Radiotherapy, Government Medical College and Hospital, West Bengal, India. Different demographic parameters like age, sex, religion, food habits were tabulated in the excel sheet. Besides that risk factors (gall stone disease, alcohol, smoking history), infection history (HBV, HCV, typhoid fever), clinical history, type of presentation were also noted. Detail treatment history and the outcome within this time period were also considered. The stage of the cancer defined in our study as metastatic and non-metastatic.
Laboratory investigations, parameters and procedures: Complete blood count, blood sugar (F) and (pp), kidney function test-urea, creatinine, liver function test- bilirubin, SGOT, SGPT, Serological marker like CA19-9, X-ray chest PA View, CT and MRI/ MRCP whole abdomen.
Histopathological examination: i. Fine needle aspiration cytology, ii. Core biopsy.
Statistical analysis
Statistical analysis was done by MS excel version. As this a single intuitional study, we purposefully did not showed the statistical significance with p-value.
Results
This was a retrospective, descriptive, tertiary cancer care institute based study. The results were as follows: Total 108 patients were enlisted in our study. The distribution of disease was highlighted in the table. Mean age of diagnosis was 53.4 ± 10.6. Range from <30 years to >60 years (Figure 1 and 2).
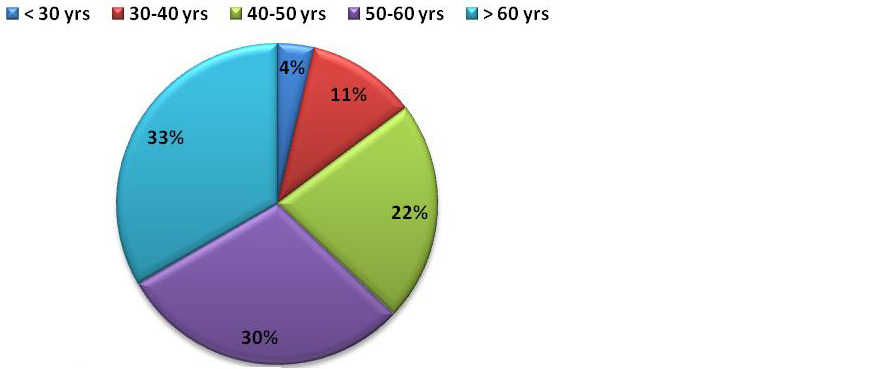
Figure 1: Age wise number of patients (N=108).
Male: female ratio was 1:1.8. The disease was found more common in female (64%) (Figure 2).

Figure 2: Patients segregation - sex wise (N=108).
89.81 % tumours are adeno-carcinoma and rest are squamous cell carcinoma (Table 2)
Table 2: Histology.
|
Histological pattern
|
No. of patients
|
|
Adenocarcinoma
|
97
|
|
Squamous cell carcinoam
|
11
|
Patienst were usually presented with pain in right upper quadrent (62.04%), dyspepsia. Nausea & vomiting, weight loss (Figure 3).
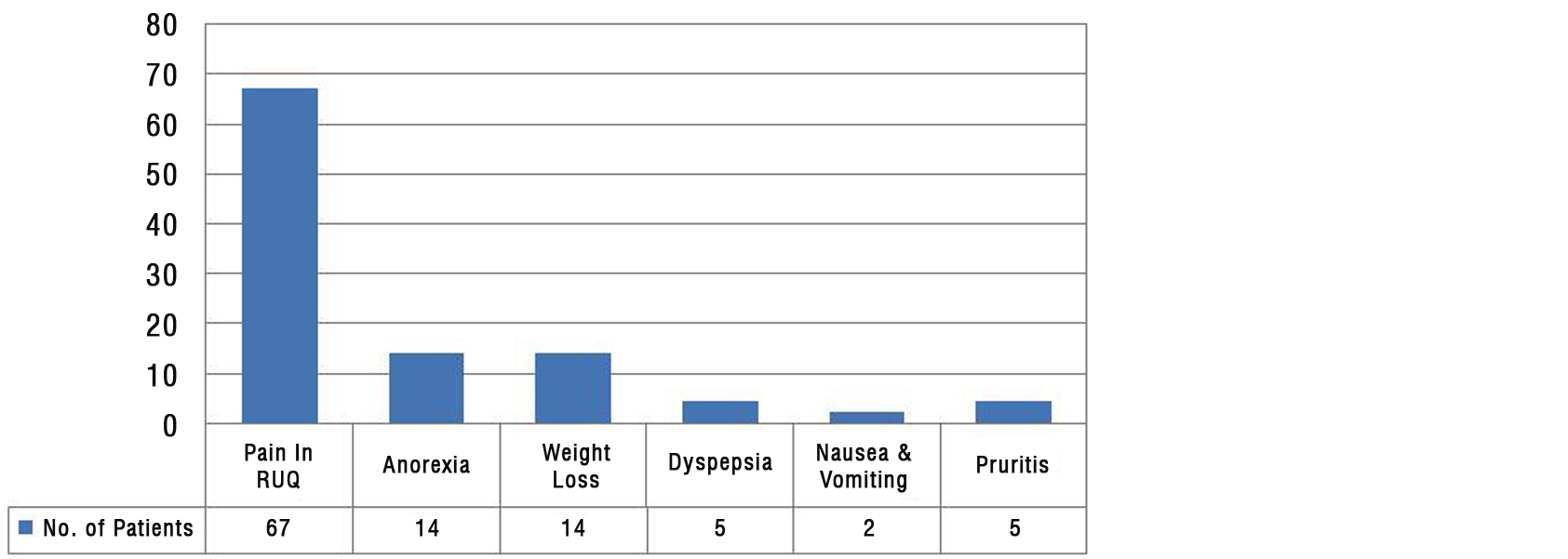
Figure 3: Clinical presentation (N=108).
Patients were usually presented with Jaundice (64.82%). and palpable lump (12.97%) (Figure 4).
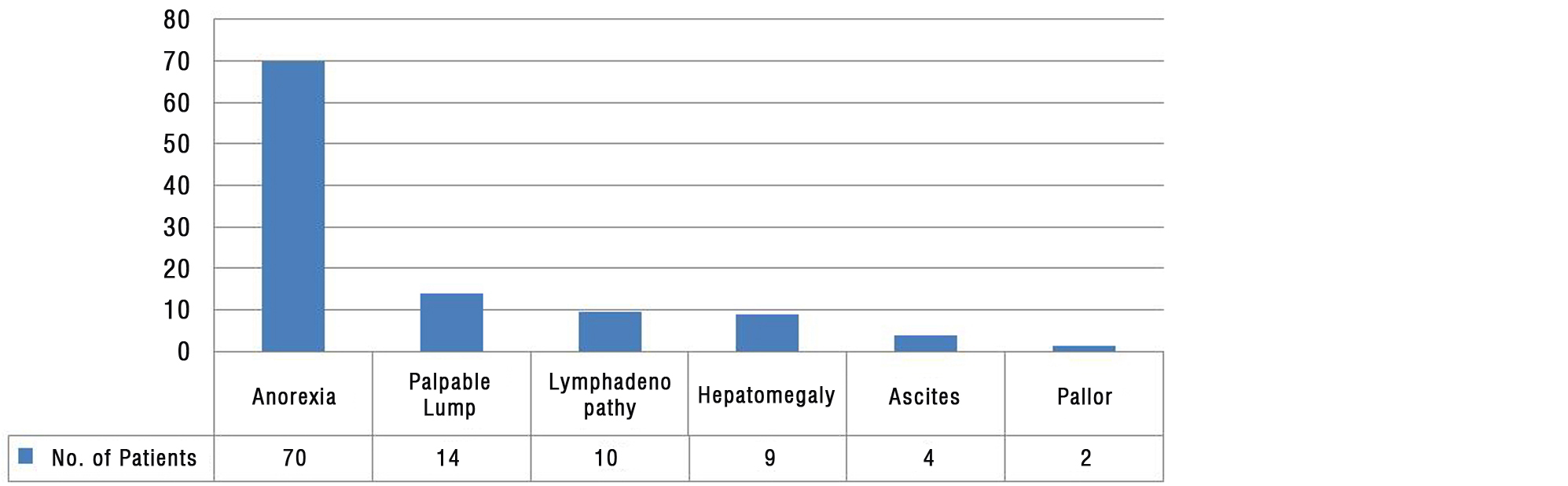
Figure 4: Clinical findings (N=108).
Maximum number of patients (86%) were diagnosed at metastatic stage (Figure 5).
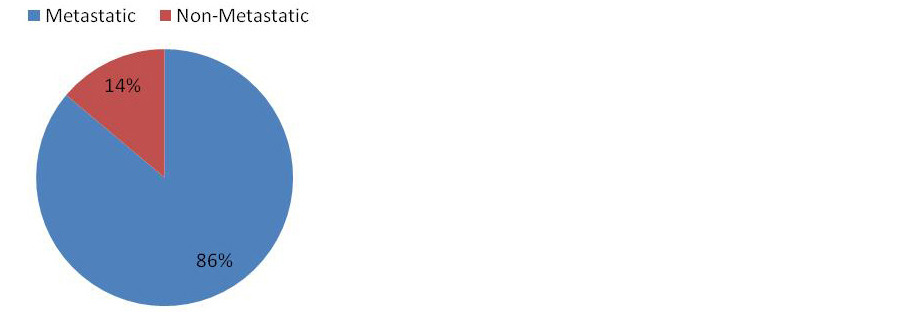
Figure 5: Stages presentation (N=108).
59.26% patients develoved gallbladder cancer by gall stone. Other risk factors include porcelain gallbladder, gallbladder polyp of > 10mm diameter and anamolis pancreatico biliary duct junction (APBDI), Heptitis B virus and hepatitis C virus (Figure 6).
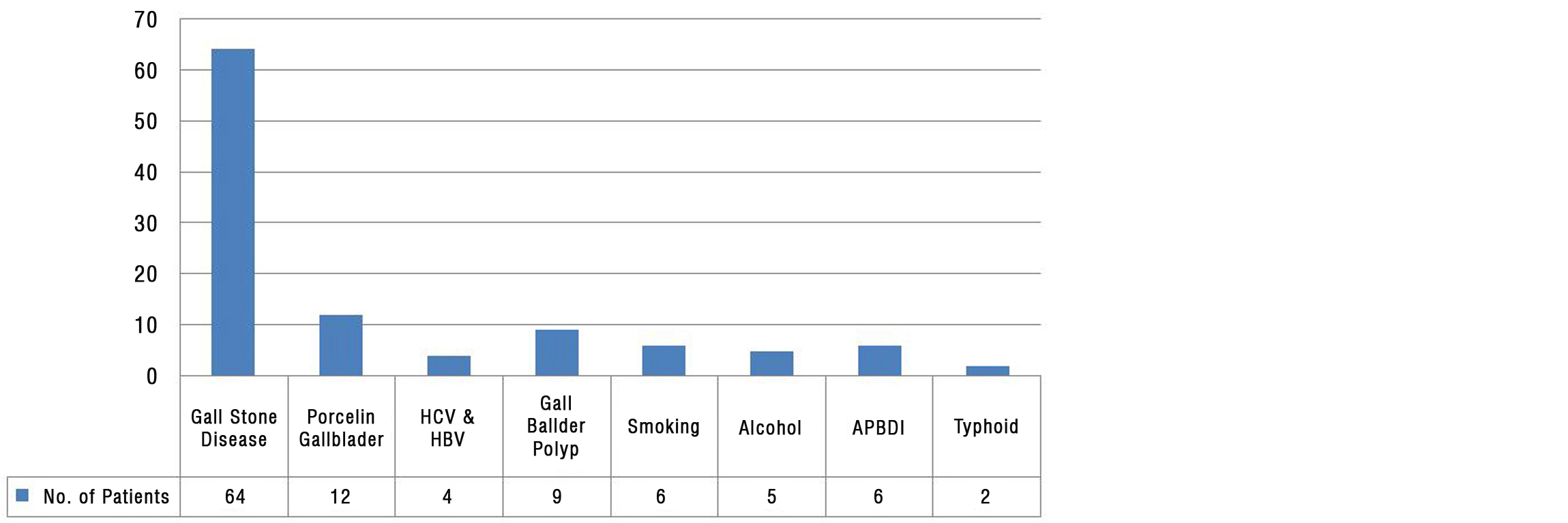
Figure 6: Risk factors (N=108).
Maximum spread of tumor by local invasion (including liver segment IV & V) through lymphatic and venous blood to liver (73.15 %).
Management of patients of gallbladder carcinoma
Patients, who were potentially curable, were sent to surgery department for radical surgery. After surgery, patients histopathological report were examined and then they were planned for adjuvant chemotherapy (Figure 7). Most histological pattern is Adenocarcinoma. Common chemotherapy regimens were gemcitabine + cisplatin (N=49), gemcitabine + oxaliplatin (N=31) and cisplatin + 5-Fu (5-fluorouracil, N=28). Combination of gemcitabine + cisplatin gives a higher response of 61%, in our study. Metastatic patients were planned for palliative therapy according to their compliance i.e., whose performance status was in between ECOG 1 and ECOG 2, they were planned for intravenous (IV) chemotherapy. Who were not fit for IV chemotherapy they were either given oral chemotherapy (tab capecitabine) or offered best supportive care. All patients received symptomatic management. Patients with high bilirubin were referred to competent department for percutaneous trans biliary drainage (PTBD) stenting.
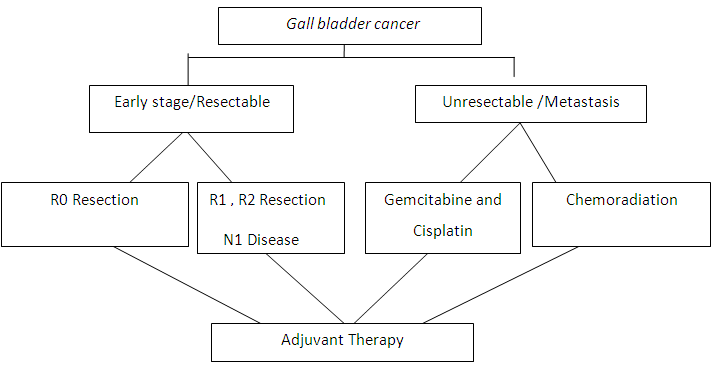
Figure 7: Management of patients of gallbladder carcinoma.
In case of locally advanced disease adjuvant therapy with EBRT (median dose of 45 Gy. in 25 fractions for 5 weeks) and chemoradiotherapy (5-Fu) generally given after surgery. During that after 1-year of study period, 34 patients died due to the disease process.
Discussion
A good number of gallbladder cancer patients visited to my radiotherapy outpatients department (OPD) regularly. The incidence of the disease in female was 1.8 times more than males. Women with gall stones are at 2.4 times higher risk than males for gallbladder carcinoma [7].
In various Indian series the female: male ratio varies from 3:1 [8]. Our study shows that female: male ratio 1.8:1. A study from South India, which is a low incidence area, contradicts the above with male: female ratio of 1.6:1 [9].
Pain in right upper quadrant is most common clinical features, followed by loss of appetite, which was also evident in our study. In our study most common clinical findings were Jaundice (64.82%) and palpable lump (12.97%), which is described in our textbook literature [10].
In our study we found that 59.26% of affected population had gall stone disease and other risk factor included porcelain gallbladder, gallbladder polyp and APBDI. Pathogens such as H. pylori and S. typhi are known for their potential to initiate carcinogenesis [11-14]. Cholecystectomy is done in patients who have S. typhi carrier state and Gall stone [11]. All patients were given chemoradiotherapy (25 Gy. in 25 fractions, 5 days/week) with 5-Fu.
In our study four patients suffering from gallbladder stone, underwent cholecystectomy, but unfortunately detected gallbladder carcinoma.
Although there is high incidence of GBC in our country, incidental GBC is fairly underreported due to no active screening program. They can be dealt with great deal of suspicion. Routine annual screening of the gallbladder by ultrasound can be helpful in these patients [15, 16]. If patients are suspected with high risk gallbladder cancer, they can be early detected and radical cholecystectomy to be done properly during surgery [17]. Another study in Delhi shows that 59% of patients are from rural area versus 41% patients from urban area with gallstones [18]. Our study also shows that maximum patients are from rural area. Dubey et al. shows that 75% of patients with GBC belong to lower-middle or lower-socio-economic class [19]. Our study corroborate with this finding.
In a study from Tertiary Care Hospital of North India, of 3,827 endoscopic retrograde cholangio-pancreatography (ERCP), only 2.6% had pancreaticobiliary junction anomaly [APBDI] [20]. Corroborating these findings, in our study there are six patient of APBDI causing GBC. Studies from Japan have suggested that a fair number of patients with GBC have APBDI [21].
Gallbladder polyps are present in around 5% of adult patients. Most of them (95%) are non-neoplastic in nature. Benign adenomas associated with gallstones, older age and rapidly increasing size of polyp suggests neoplastic nature of the polyp [22]. Differentiation of benign versus malignant polyp is done by endoscopic ultrasound. Increased risk for neoplasia is identified by presence of hypoechoic, heterogenous lesion with height/width ratio (0.8) and increased vascularity [23].
Close follow-up for 3–6 months is required to detect increase in polyp size. Cholecystectomy is done to patients associated with gallbladder wall thickness or family history of malignancy [22, 23].
Porcelain gallbladder is fragile, and it leads to dystrophic calcification. It imparts a bluish tinge to the gallbladder. The calcification may be focal or diffuse. It is prevalent in 0.1–0.2% of patients with GB disease. 25% of older patients with porcelain gallbladder have prevalence of GBC. However, a recent systematic review of 111 studies suggest that rate of GBC is only 6%. Gallbladders with focal, stippled or multiple punctuate calcification, those associating with thickening of gallbladder wall and symptomatic porcelain gallbladder are more likely to harbour malignancy. These patients may benefit from prophylactic cholecystectomy [24, 25].
Patients with chronic biliary inflammation promote carcinogenesis. So they need annual surveillance for GBC and are likely to benefit with prophylactic cholecystectomy. In a study from Lucknow, 87% of the GBC cases were from oral contraceptive users [26]. Other drugs causing gallbladder carcinoma are methydopa and isoniazid [27, 28]. Post-menopausal women undergoing oral hormone replacement therapy leads to gallbladder carcinoma. Transdermal patches of HRT are better than oral estrogen. The GB mucosa has been found to have estrogen and progesterone receptors which may promote GB stasis and stone formation. This in turn increases exposure time of the GB mucosa to bacterial and chemical toxins [29].
Czito et al. [30] shows that a retrospective analysis done on 22 patients with primary and non-metastatic gallbladder cancer and those who were treated with surgical resection followed by concurrent chemoradiotherapy (median dose 45 Gy) and 5 FU chemotherapy. Our study corroborate with the above process. Czito et al. [30] also shows that five-year LRC, DFS and OS were 59%, 33%, and 37% respectively and median survival was 1.9 year. Socio-demographic and clinical characteristics of the patients with gallbladder is being evaluated by this study to meet future challenges of gallbladder cancer. This data may be an indicative for further studies and public health policies in these states regardless of etiology. As it is performed in specialized institutions, this result shows that this unfavourable scenario can be changed by monitoring at-risk patients. To prevent late stage gallbladder cancer diagnosis, it is necessary to have a standardization of the screening and monitoring of gallbladder disease.
Determination of staging of gallbladder was done based on clinical protocols, post operative histopathology report and metastatic work-up. While databases provide patient death information, there might be under reporting. Under reporting of patients is due to death of patients outside the hospital and whose records are not closed in the system. Study results should be interpreted carefully for the above reasons. When it comes to public policies with the generation of relevant evidence of a larger number of patients, it helps in broader analysis and decision making.
Limitations
The OPD attendance was hindered by COVID-19 pandemic and related complete lockdown during this period. Lack of dedicated surgical oncology unit unwillingly obscured patient’s outcome. Being a single institutional study, results derived cannot be extrapolated in the entire study. Detailed subgroup analysis was required for identifying risk factors in individual cancers.
Conclusions
In our study, devastating outcome was noted to most of the patients due to late presentation. GBC affects patients at a younger age than their western counterparts in developed nations. Selected patients with gallbladder stone, polyp and cyst, in these regions are easily identifiable targets via imaging techniques, which may be offered prophylactic cholecystectomy to prevent GBC. In the current scenario and the challenges for the future, large multicentric comprehensive studies are required in India. This will help in formulating cost effective national strategies in preventing GBC related mortality in the country.
Acknowledgement
Authors were eternally grateful to Prof. Dr. Partha Pratim Mukhopadhyay for guiding in ethical issues and logistic support.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] GLOBOCAN: 2020, International Agency For Research on Cancer ,WHO. India.
[2] Rai A, Mohapatra SC, Shukla HS. A review of association of dietary factors in gallbladder cancer. Indian J Cancer. 2004; 41(4):147–151.
[3] Dutta U, Bush N, Kalsi D, Popli P, Kapoor VK. Epidemiology of gallbladder cancer in India. Chin Clin Oncol. 2019; 8(4):33.
[4] Acharya SK. Epidemiology of hepatocellular carcinoma in India. J Clin Exp Hepatol. 2014; 4(Suppl 3):S27–S33.
[5] Feng J, Polychronidis G, Heger U, Frongia G, Mehrabi A, et al. Incidence trends and survival prediction of hepatoblastoma in children: a population-based study. Cancer Commun (Lond). 2019; 39(1):62.
[6] Levy AD, Murakata LA, Rohrmann CA. Gallbladder carcinoma: Radiologic-pathologic correlation. RadioGraphics. 2001; 21(2):295–314.
[7] Jain K, Sreenivas V, Velpandian T, Kapil U, Garg PK. Risk factors for gallbladder cancer: A case-control study. Int J Cancer. 2013; 132(7):1660–1666.
[8] Bhagabaty S, Sharma J, Krishnatreya M, Nandy P, Kataki AC. Profiles of gallbladder cancer reported in the hospital cancer registry of a Regional Cancer Center in the North-East India. Int J Res Med Sci. 2014; 2(4):1683.
[9] Sachidananda S, Krishnan A, Janani K, Alexander PC, Velayutham V, et al. Characteristics of Gallbladder Cancer in South India. Indian J Surg Oncol. 2012; 3(3):228–230.
[10] Abou-Alfa GK, Jarnagin W, Lowery M, D’Angelica M, Brown K, et al. Liver and bile duct cancer. In: Neiderhuber JE, Armitage JO, Doroshow JH, Kastan MB, Tepper JE, eds. Abeloff’s Clinical Oncology. 5th ed. Philadelphia, PA. Elsevier; 2014; pp.1373–1395.
[11] Patel T, Borad MJ. Carcinoma of the biliary tree. In: DeVita VT, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenberg’s Cancer: Principles and Practice of Oncology. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015; pp.715–735.
[12] Nagaraja V, Eslick GD. Systematic review with meta-analysis: the relationship between chronic Salmonella typhi carrier status and gall-bladder cancer. Aliment Pharmacol Ther 2014; 39(8):745–750.
[13] Bansal VK, Misra MC, Chaubal G, Gupta SD, Das B, et al. Helicobacter pylori in gallbladder mucosa in patients with gallbladder disease. Indian J Gastroenterol. 2012; 31(2):57–60.
[14] Matsukura N, Yokomuro S, Yamada S, Tajiri T, Sundo T, et al. Association between Helicobacter bilis in bile and biliary tract malignancies: H. bilis in bile from Japanese and Thai patients with benign and malignant diseases in the biliary tract. Jpn J Cancer Res. 2002; 93(7):842–847.
[15] Said K, Glaumann H, Bergquist A. Gallbladder disease in patients with primary sclerosing cholangitis. J Hepatol. 2008; 48(4):598–605.
[16] Chapman R, Fevery J, Kalloo A, Boberg KM, Shneider B, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010; 51(2):660–678.
[17] Mishra RR, Tewari M, Shukla HS. Helicobacter pylori and pathogenesis of gallbladder cancer. J Gastroenterol Hepatol. 2011; 26(2):260–266.
[18] Lafaro KJ, Demirjian AN, Pawlik TM. Epidemiology of hepatocellular carcinoma. Surg Oncol Clin N Am. 2015; 24(1):1–17.
[19] Dutta U, Garg PK, Kumar R, Tandon RK. Typhoid carriers among patients with gallstones are at increased risk for carcinoma of the gallbladder. Am J Gastroenterol. 2000; 95(3):784–787.
[20] Kochhar R, Singhal M, Nagi B, Lal A, Dutta U, et al. Prevalence of type iii anomalous pancreaticobiliary junction in a tertiary care hospital of North India. JOP 2009; 10(4):383–386.
[21] Mori K, Nagakawa T, Ohta T, Nakano T, Kayahara M, et al. Association between gallbladder cancer and anomalous union of the pancreaticobiliary ductal system. Hepatogastroenterology. 1993; 40(1):56–60.
[22] Dutta U, Poornachandra KS. Gallbladder polyps: how to pick up the sinister ones. J Gastroenterol Hepatol. 2009; 24(2):175–178.
[23] Hickman L, Contreras C. Gallbladder Cancer. Surg Clin North Am. 2019; 99(2):337–355.
[24] DesJardins H, Duy L, Scheirey C, Schnelldorfer T. Porcelain Gallbladder: Is Observation a Safe Option in Select Populations? J Am Coll Surg. 2018; 226(6):1064–1069.
[25] Schnelldorfer T. Porcelain Gallbladder: A benign process or concern for malignancy? J Gastrointest Surg. 2013; 17(6):1161–1168.
[26] Dwivedi S, Madeshiya A, Singh D, Singh S, Krishna A. Gallbladder Cancer and some epidemiological factors: A cross sectional study. Biomed Res. 2013; 24(1):5.
[27] Lowenfels AB, Norman J. Isoniazid and bile duct cancer. JAMA. 1978; 240(5):434–435.
[28] Dixit R, Shukla VK. In: Perspectives in Cancer Prevention-Translational Cancer Research - Why Is Gallbladder Cancer Common in the Gangetic Belt? Sudhakaran P, editor. New Delhi: Springer; 2014. pp.145–151.
[29] Baskaran V, Vij U, Sahni P, et al. Do the progesterone receptors have a role to play in gallbladder cancer? Int J Gastrointest Cancer. 2005; 35(1):61–68.
[30] Czito BG, Hurwitz HI, Clough RW, Tyler DS, Morse MA, et al. adjuvant external-beam radiotherapy with concurrent chemotherapy after resection of primary gallbladder carcinoma: A 23-year experience. Int J Radiat Oncol Biol Phys. 2005; 62(4):1030–1034.