Full Text
Introduction
Ischemia of bone includes medullary infarction, cortical ischemia and osteonecrosis of the articular margins. Bone infarction is a term used to refer to bone marrow necrosis within the metaphysis or diaphysis of a long bone. Necrosis is a type of cell death due to irreversible cell injury. Bone ischemia also includes cortical bone sclerosis and avascular necrosis by the way of collapse of articular ends of bones, small bones of hands and feet and ossification centres [1]. The causes of these are many and are listed in Table 1.
Table 1: Associated lesions and causes of Ischemia of bone:
|
• Idiopathic
• Trauma
• Hemoglobinopathies, e.g. sickle cell disease
• Gaucher disease
• Collagen vascular disorders including Lupus
• Behçet's disease
• Corticosteroid excess (both endogenous and exogenous)
• Alcohol
• Radiotherapy
• Chemotherapy for lymphoma
• Pancreatitis
• Gout
• Infection
• Renal transplant
• Diabetes
• Caisson disease
• Fibrous dysplasia
|
Of these, the common entities include steroids and other non-steroidal pain killing drugs, alcoholism, trauma and systemic disorders including hemoglobinopathies, Gaucher disease, Gout, collagen vascular disorders, etc. [2].
Bone infarction involves the bone marrow of long bones.
Bone ischemia that occurs in systemic disorders such as hemoglobinopathies is shown as sclerosis of the cortical bone on conventional films with infarcts. Ischemia of the physeal region results in shortening of the bone such as seen in trauma, sickle cell anemia, radiation therapy, etc.
Osteonecrosis involves the epiphysis, small bones of the hands and feet, articular margins of long bones in adults and ossification centres in children. Radiographically there are several stages in bone marrow infarction and avascular necrosis. Plain films may be normal initially but MRI demonstrates classical findings in the bone marrow and in osteonecrosis.
Pathologically, the blood supply to a section of bone is interrupted and an infarct forms. The infarct includes a central necrotic core which is surrounded by a hyperemic ischemic zone. With time collagen granulation tissue becomes layered around the necrotic core. Demarcation between the normal surrounding marrow, the ischemic zone, and the necrotic core accounts for many of the radiographic appearances of bone infarcts. Calcification occurs eventually due to saponification of fat in necrotic areas. Investigations mainly include conventional radiology and MRI. An interesting observation is the presence of gas in post traumatic osteonecrosis of the vertebral body and it goes by the name of Kummell disease. Similarly gas emboli producing osteonecrosis in bones is noted in Caisson disease. Other methods of imaging are included in Table 2.
Table 2: Imaging methods.
|
• Conventional radiographs
• CT
• MRI
• Nuclear bone scanning
• PET CT
|
Imaging features and discussion
Conventional radiology is the initial investigation and the infarct can be missed in early stages, where CT and MRI will help. Radionuclide scanning is non-specific but identifies the location of the lesion. In acute ischemia, radionuclide scan is cold and as reparative changes take place, it becomes hot. PET scan shows the different changes better (Figure 1).
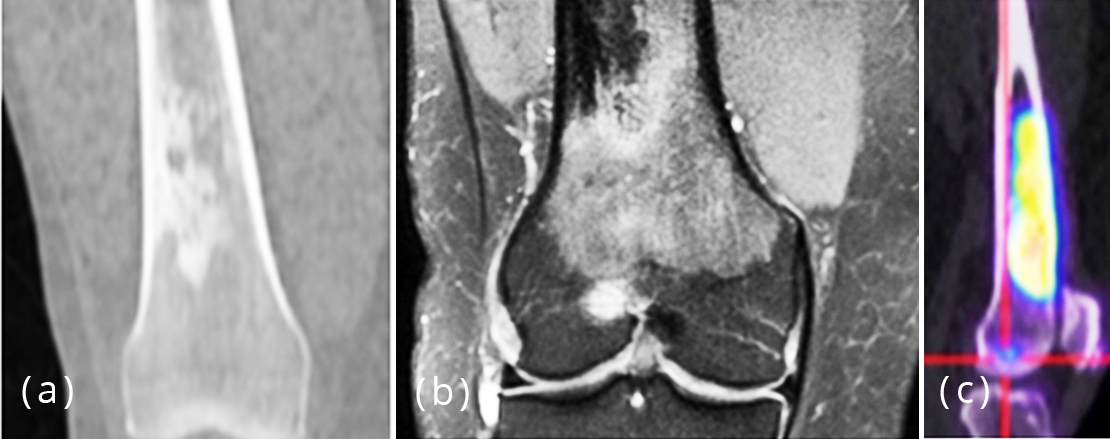
Figure 1a-c: Bone infarcts, (a) conventional, (b) MRI, (c) PET scan.
Imaging features of bone infarction
On conventional radiography, a significant delay occurs between the onset of infarct and development of radiographic signs. In acute infarct, the findings may simulate acute osteomyelitis such as seen in children with osteolysis and periosteal reaction. It is better noted in Sickle Cell Dactylitis (Figure 2a,b). In the spine, cup-like deformities are noted with a “step off” density in the middle-third of the depressed articular plate (Figure 2c). This is called Raynold’s Phenomenon representing the site of infarction of bone. MRI at this time identifies the lesion. Early in the course of disease a bone infarct may develop as an area of rarefaction and, later, may have a mixed, osteolytic and sclerotic pattern. With healing, the lesion becomes well demarcated, with a serpiginous or linear zone of calcification and ossification. The calcified peripheral zone is called fibroosseous membrane and this is specific for bone infarct.
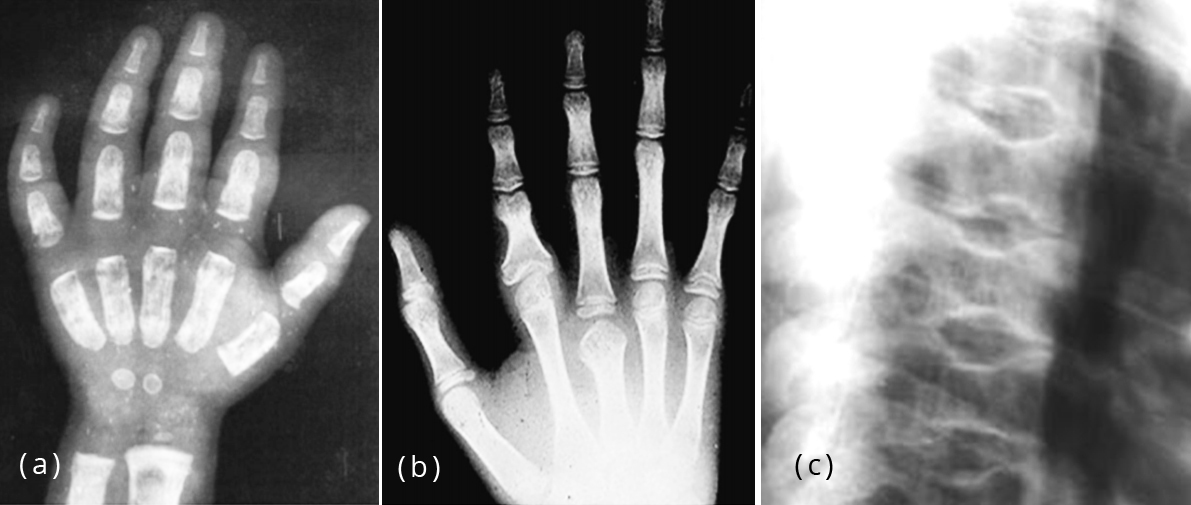
Figure 2: (a) Sickle cell dactylitis - with infarctions, (b) Sickle cell dactylitis -shortening of bones in sickle cell anemia, (c) Sickle cell disease, step-off defect.
The serpiginous calcifications when seen end-on simulate enchondroma. However, the calcifications in enchondroma are nodular, arc-like, and circular. Radiographic findings depend upon the stage of the disease. Periostitis is rare in chronic infarcts. The lesion may be limited to diaphysis, metaphysis or may extend from metaphysis to articular margin. They are often bilateral and multiple, and whatever the etiology, the imaging findings are similar. However, the morphological characteristics of infarcts are different in each case.
CT: CT would outline the mineralized portion of the infarct (Figure 3).

Figure 3: CT – Infarct of the humerus extending to the head.
MRI features are as follows
An important feature in differentiating bone infarct from other medullary lesions is that the central signal usually remains that of normal marrow. The marrow is not replaced.
T1 shows serpiginous peripheral low signal due to granulation tissue and to lesser extent sclerosis, peripheral rim may enhance post gadolinium and central signal usually that of marrow (Figure 4).
T2 shows double-line sign: hyperintense inner ring of granulation tissue and a hypointense outer ring of sclerosis, absence of double-line sign does not exclude bone infarct and central signal usually that of marrow.
Radionuclide bone scan shows no uptake (cold spot) in the early stage where blood supply is absent, and shows mildly increased uptake at periphery during acute phase.
Differential diagnosis: (1) Enchondroma: chondroid matrix, central marrow signal is absent, (2) Healing non-ossifying fibroma: usually cortically oriented and is not medullary, (3) Lipoma: well circumscribed fatty lesion with varying degrees of calcification, (4) Brodie’s Abscess: Penumbra effect of the border.
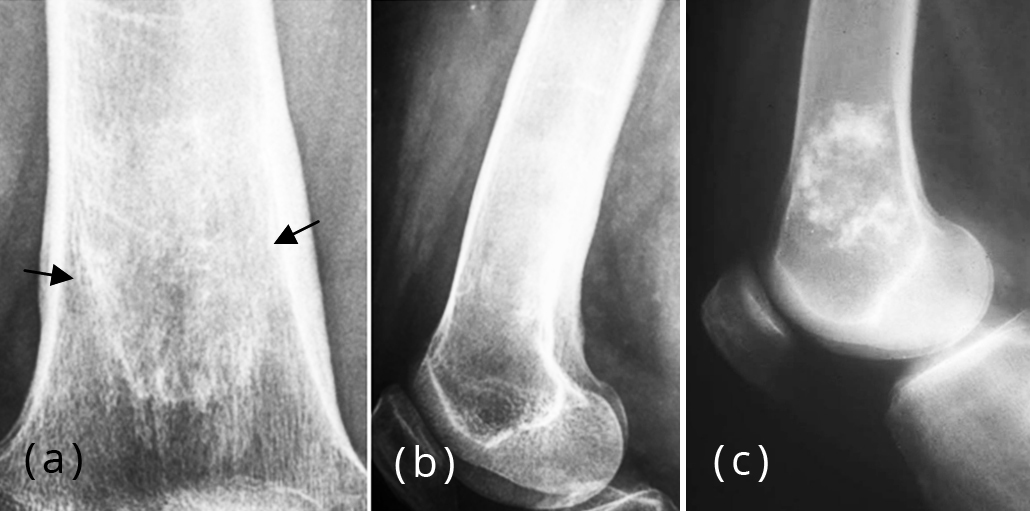
Figure 4: (a, b) Infarct, well demarcated peripheral rim, (c) Enchondroma, note the arc-like and circular calcifications.
Idiopathic
Osteonecrosis of femoral head or otherwise called avascular necrosis (AVN) is defined as bone death of the adult femoral head owing to ischemia. Majority of the times, the etiology may not be established. The plain radiographic features follow a sequence with the Crescent sign (Figure 5a) to start with, followed by osteoporosis, osteosclerosis, cystic changes, collapse of femoral head and secondary osteoarthritic changes (Figure 5b-e). It may be bilateral (Figure 5f). Another sign which is characteristic of avascular necrosis of the head of the femur is Snowcap sign which is on the top of the necrotic area (Figure 5c) [3]. There is classification of the stages of osteonecrosis of the femoral head, the details of which are not included in this article.
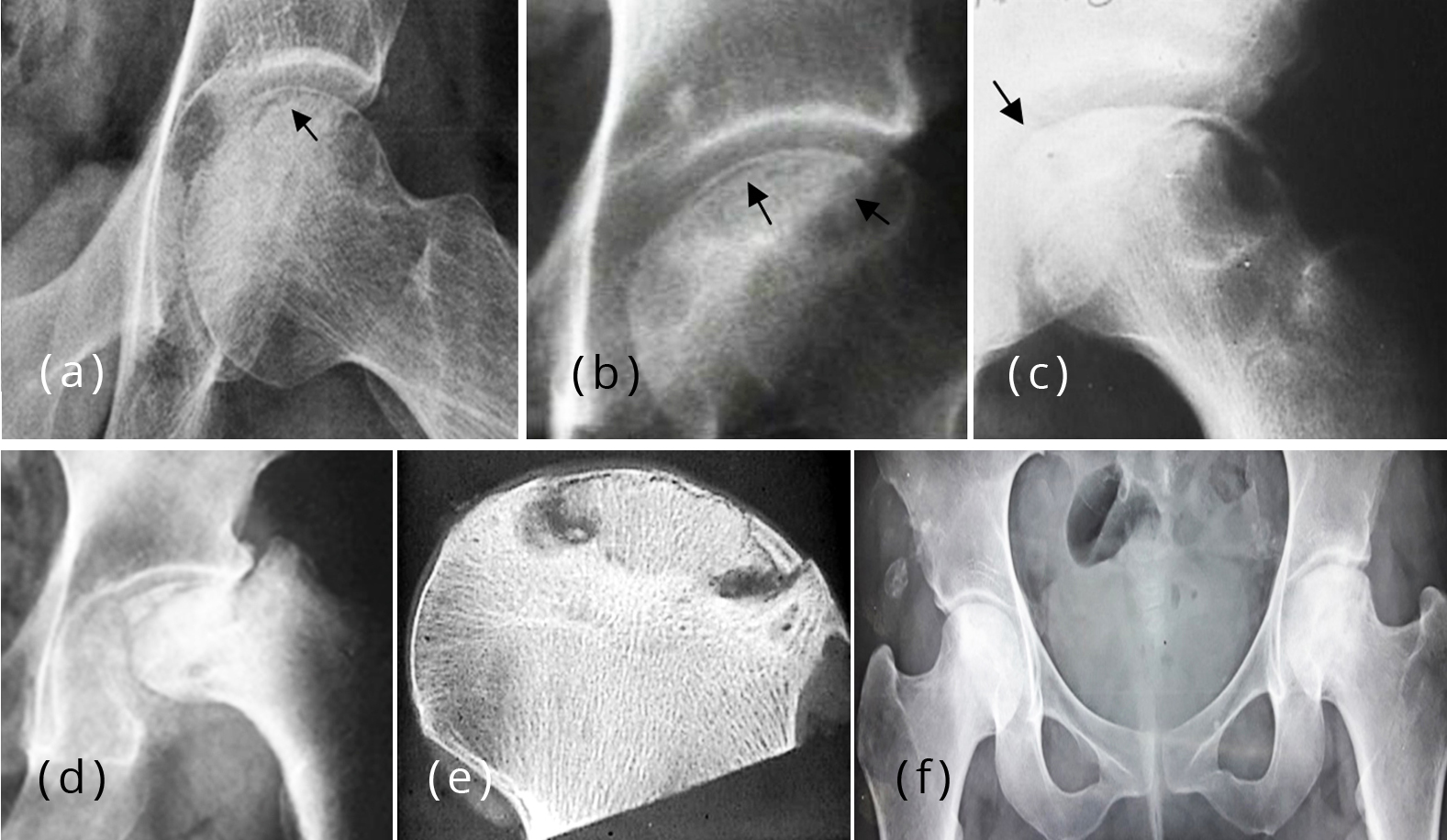
Figure 5: (a) Avascular necrosis head of femur – Crescent sign. (b-d) Crescent sign in osteonecrosis with collapse of fragment, (c) Snowcap sign, (e) Specimen AVN femoral head, (f) Bilateral avascular necrosis both femoral heads, 24 F.
Osteonecrosis (ischemic necrosis) of the proximal epiphysis of the femur is called Perthe’s disease and is common in boys aged between 4-8 years. Bilateral involvement is not uncommon (Figure 6). There is classification regarding the stages of Perthe’s disease, the details of which are not included in this article.
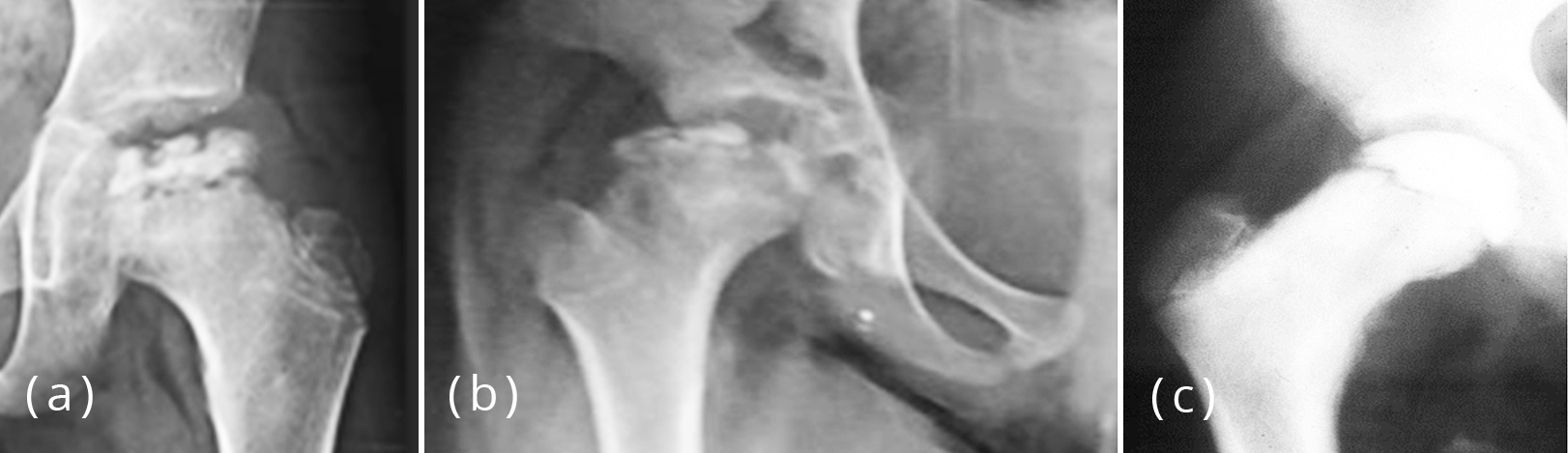
Figure 6a-c: Legg calve Perthe’s hips, (c) ivory type of epiphysis.
Trauma
Osteonecrosis of the knee is necrosis of unknown origin affecting predominantly the medial condyle of the distal femur in adults. On occasion the lateral condyle is also involved. It may be associated with trauma or any other cause such as SLE (Figure 7) [4].
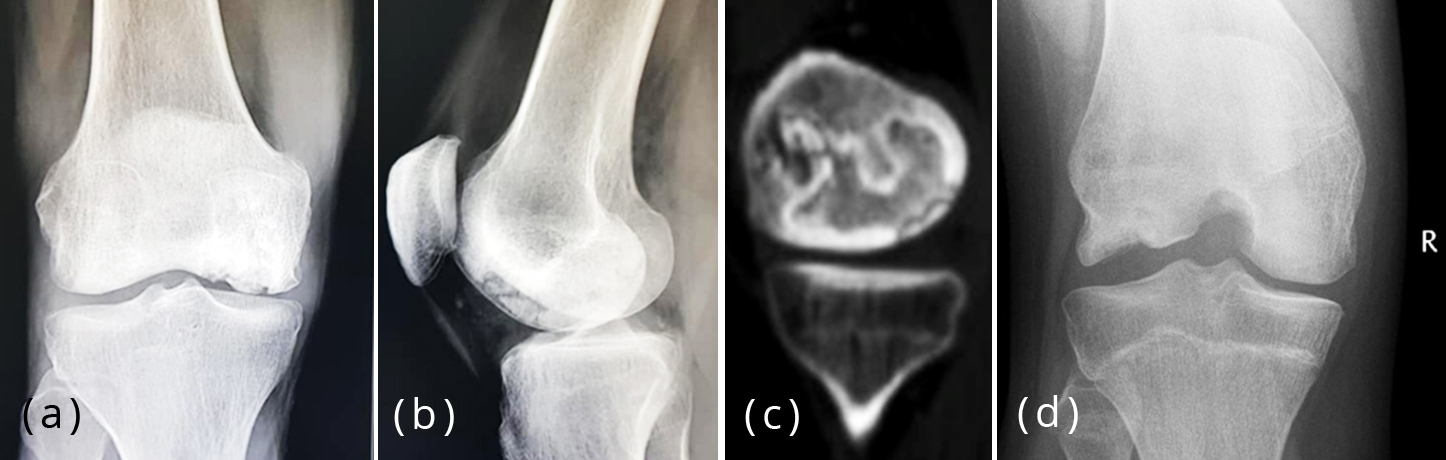
Figure 7a-d: Osteonecrosis of medial condyle, systemic lupus erythematosis, (d) advanced stage.
The exact mechanism of osteonecrosis depends primarily on the predisposing cause. In trauma, interruption of arterial supply to bone (e.g., scaphoid fracture, fracture neck of femur) is noted (Figure 8a-d).

Figure 8a-c: Post traumatic osteonecrosis of talus (T), (b, c) Osteonecrosis of the talus, Diaz’s disease, (b) and (c) stages of necrosis.
Keinbock’s disease is osteonecrosis of the lunate bone either due to trauma or some other reason. Very often the exact cause could not be established. There are five stages in the radiological spectrum, the details of which are not included here. The ultimate result is dense collapsed lunate bone (Figure 8e,f) [5].

Figure 8d-f: (d) Post-traumatic avascular necrosis of scaphoid (Preiser disease), (e, f) Keinbock’s disease.
Kümmell disease or vertebral osteonecrosis is generally noted in cases of osteoporosis, whatever the cause maybe. Gas bubbles are demonstrated in plain films as well as in CT or MRI (Figure 8g,h) [6].

Figure 8g,h: Kummell disease, post traumatic osteonecrosis with gas production.
Spontaneous multifactorial adult onset osteonecrosis of the tarsal navicular occurs in adults between 40 and 60 years of age. Plain radiographic features can include comma-shaped deformity due to collapse of the lateral part of the bone and medial or dorsal protrusion of a portion of the bone or the entire navicular bone. The disease may be bilateral or asymmetric and associated with pathologic fractures (Figure 9) [7].

Figure 9a,b: Mueller-Weiss disease, avascular necrosis of navicular.
Hemoglobinopathies
Hemoglobin SC (HbSC) disease, although a sickle cell disease subtype, with similarities to the classic condition, should ideally be considered as a distinct pathological entity (Figure 10) [8].
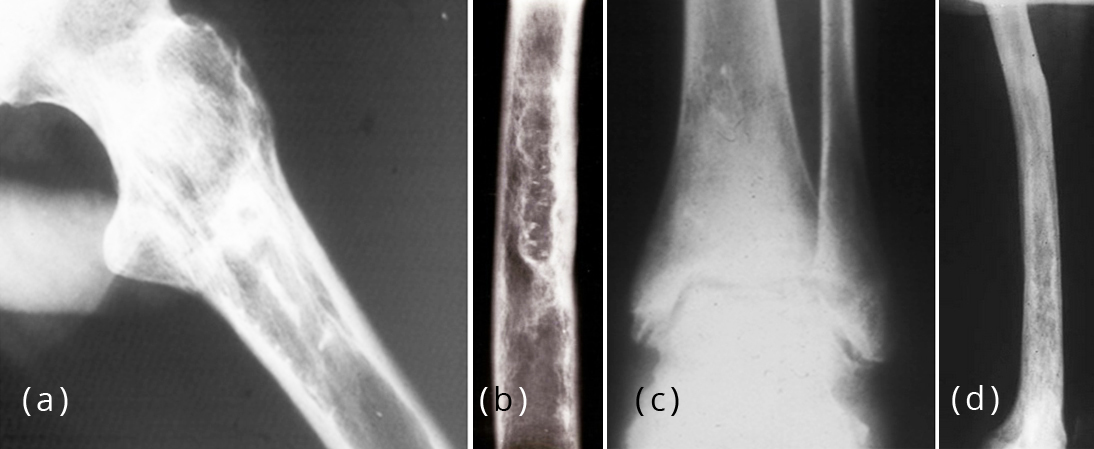
Figure 10: Bone infarcts in Sickle Cell Disease, (a) Fibroosseous membrane, (b) cortical thickening, (c) Osteosclerosis and osteonecrosis, (d) extensive bone infarct.
Gaucher's disease
Gaucher's disease is a rare familial disturbance of the cellular metabolism in the reticulo-endothelial cells and histiocytes, characterized by an accumulation and retention of the cerebroside kerasin. Marrow packing by Gaucher cells causing medullary hypertension and intraosseous venous occlusion is noted [9]. Proliferation of endosteal bone is another finding. Compromised blood supply will result in bone infarction at both subarticular and diaphyseal sites (Figure 11).

Figure 11: Infarcts in Gaucher’s disease.
Collagen vascular diseases including lupus
The body's immune system attacks its own tissues such as seen in Lupus. In many of the collagen vascular disorders, vasculitis with arterial occlusion is noted (Figure 12) [10].
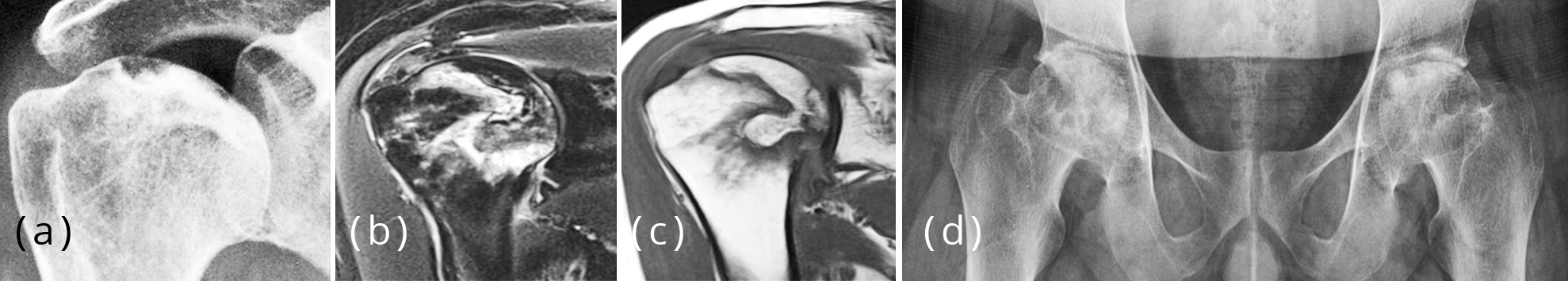
Figure 12a-d: (a-c) Osteonecrosis humeral head in lupus (HASS disease), (d) Lupus AVN both femoral heads.
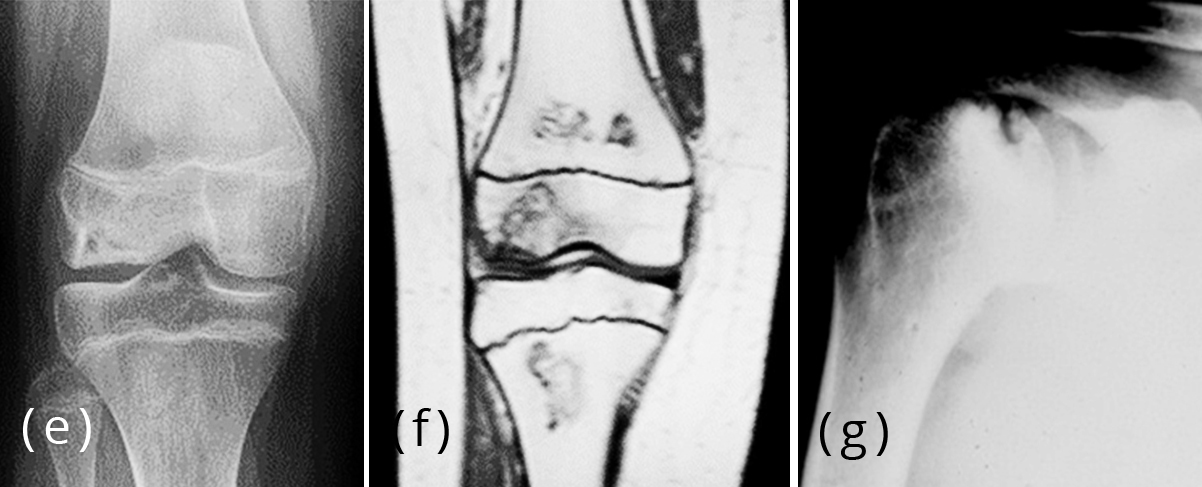
Figure 12e-g: (e, f) Bone infarcts and osteonecrosis of lateral femoral condyle in lupus, (g) Osteonecrosis humeral head in lupus.
Behcet’s disease
Behcet's disease is a multisystem disease characterized by recurrent oral and genital ulcers, relapsing uveitis, mucocutaneous, articular, gastrointestinal, neurologic, and vascular manifestations. Rheumatologic manifestations may also occur in Behcet's disease, and arthritis and arthralgia are the most common musculoskeletal findings followed by enthesopathy, avascular necrosis, myalgia, and myositis [11]. Although the main pathology of Behcet's disease has been known to be the underlying vasculitis, the etiology and exact pathogenesis of the disease are still unclear. Vasculitis causing arterial occlusion is noted.
Corticosteroid excess (both endogenous and exogenous)
Endogenous steroids are involved in a large number of physiologic processes, including modulating immune function, behavior, cardiovascular function, growth, metabolism, and inflammatory responses. In regional anesthesia and pain medicine, exogenous glucocorticosteroids (GCS) are some of the most common pharmacologic agents in clinical use. These potent intermediate to long-acting GCS are now used to promote predominantly anti-inflammatory effects on target tissues [12]. Fat cell enlargement causing medullary hypertension and intraosseous venous occlusion is noted (Figure 13).
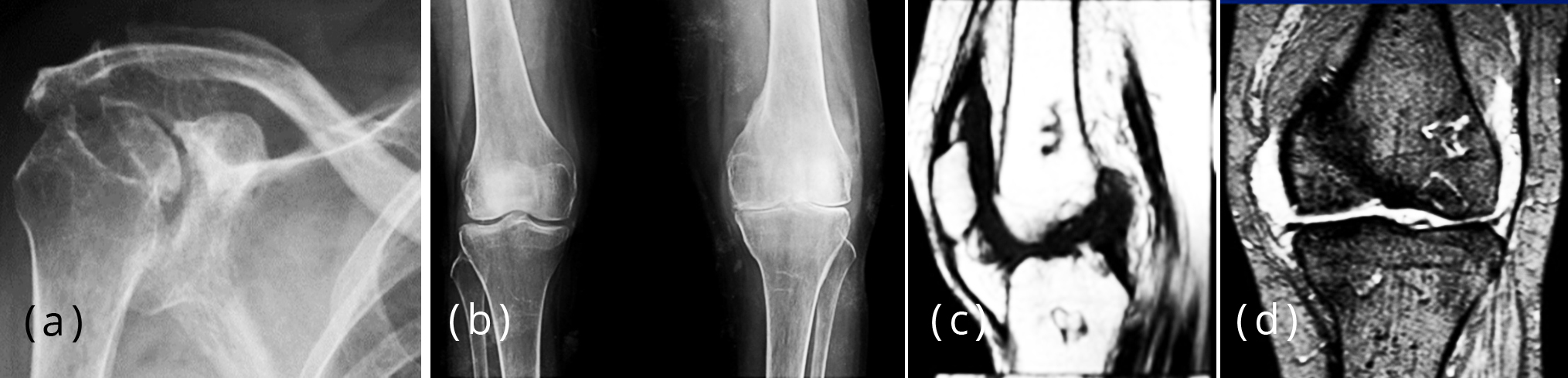
Figure 13a-d: (a) Steroid arthropathy, note the changes in the head of humerus and glenoid, (b-d) MRI - Bone infarct, steroid therapy. Plain films do no show infarcts. MRI reveals infarcts.

Figure 13e-g: (e) Bilateral bone infarcts, note the serpiginous outer margin, steroid,(f, g) 46 F, Steroid induced bone infarct extending to the articular margin.
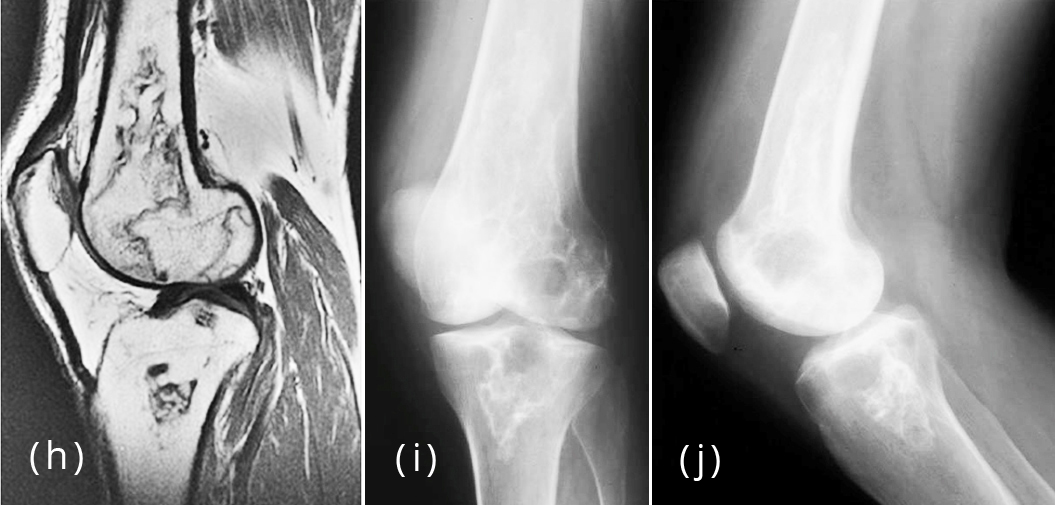
Figure 13h-j: Corticosteroid therapy producing Infarcts extending to the subarticular area.
Alcohol
Alcohol induced osteonecrosis is part of the differential diagnosis in patients with history of alcohol abuse and diffuse bone pain. Usually patients have a longer than 10 year history of alcohol abuse prior to the development of osteonecrosis. The femoral head is the commonest site involved; however, involvement of the long bones is also seen [13]. Fat embolism secondary to coexisting hyperlipidemia has been postulated as a possible cause of osteonecrosis in alcoholics. Fatty emboli causing arterial occlusion is also noted (Figure 14).
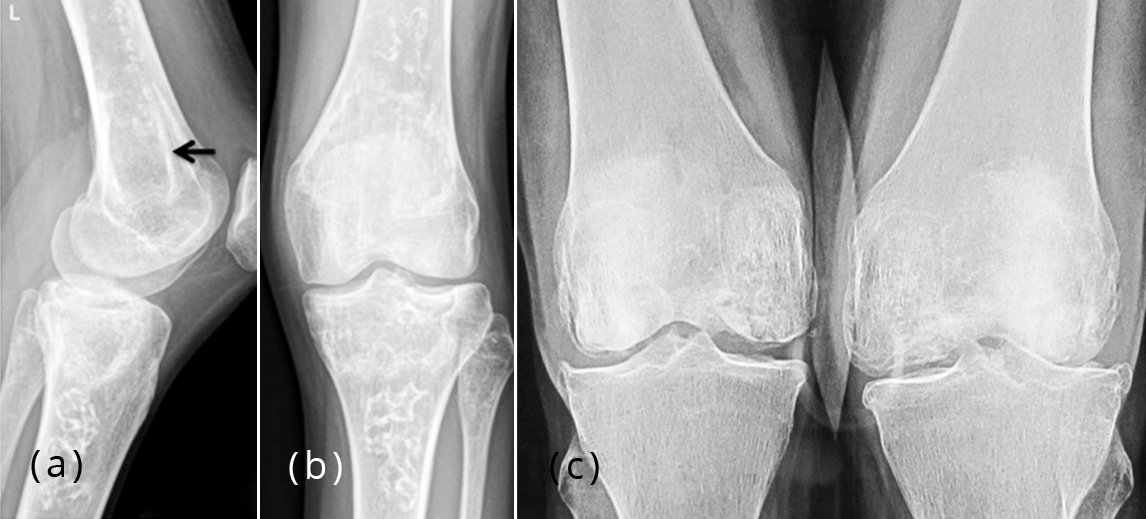
Figure 14: (a, b) Multiple bone infarcts in a chronic alcoholic, (c) Osteonecrosis femoral condyles in alcoholic.
Radiotherapy
Osteoradionecrosis (ORN) refers to a severe delayed radiation-induced injury and is characterized by bone tissue necrosis and failure in healing [14]. There is some overlap with the term Radiation osteitis. Direct injury to vascular supply leading to occlusion is noted (Figure 15a,b).
Chemotherapy Single or multiple infarcts are not uncommon in therapy of lymphomas and other myeloproliferative disorders (Figure 15c,d) [15].
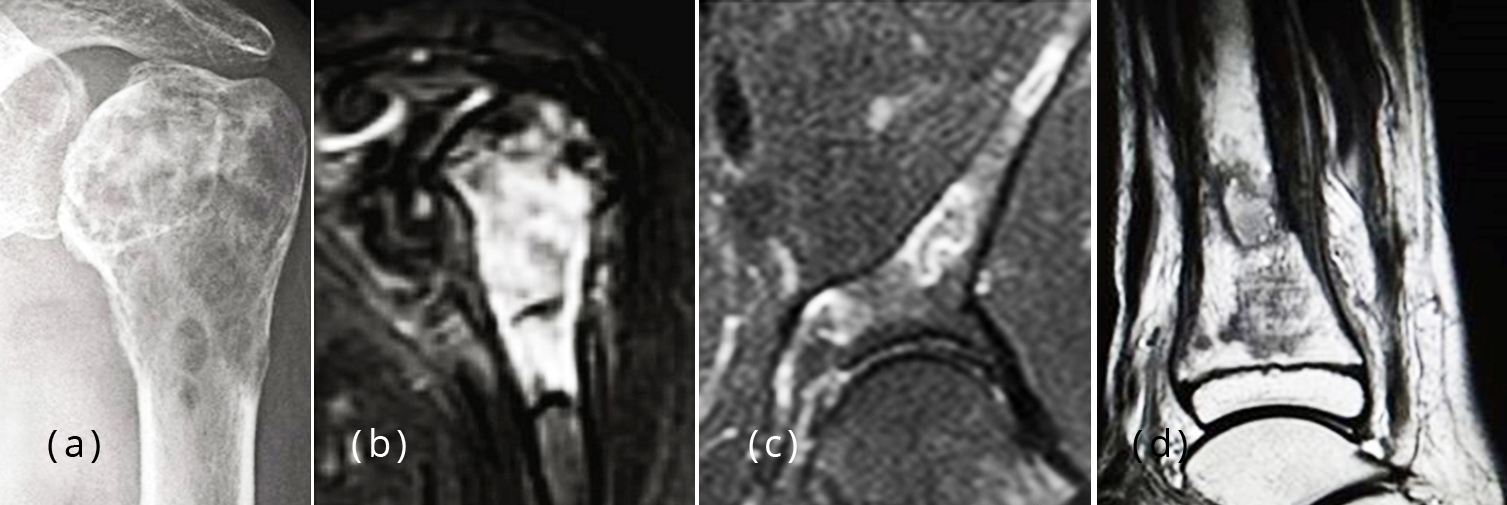
Figure 15: (a, b) Necrosis of femoral head after radiotherapy for carcinoma of the breast, (c) Multiple Infarcts iliac bone after chemotherapy for lymphoma. (d) Lymphoma chemotherapy, lower end of tibia in a child.
Pancreatitis
Sporadic cases of intramedullary fat necrosis associated with bone destruction have been reported in conjunction with acute and subacute pancreatitis, traumatic pancreatitis, and pancreatic carcinoma [16].
Gout
The radiographic manifestations of bone ischemia and the possible mechanism of infarction in gout are monosodium crystal deposits in small vessels [17].
Infection
In chronic osteomyelitis, sequestrum is a common observation which is a dead bone and an example of ischemic bone (Figure 16) [18]. The increased bone density in the sequestrum is partly due to ischemia and mostly due to collapsed trabeculae.

Figure 16: Chronic osteomyelitis with sequestrum.
Renal transplant
It is not uncommon to observe bone necrosis in patients who had organ transplant therapy particularly renal transplant. Besides the classical findings of osteonecrosis, infarcts also may be seen (Figure 17) [19]. Some of the necrotic cases are attributed to steroid and other immunotherapy.
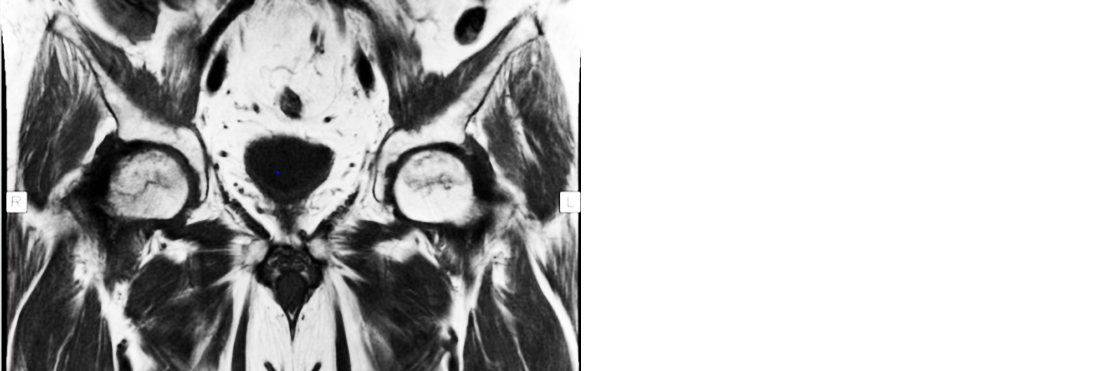
Figure 17: Renal transplant, bilateral osteonecrosis femoral heads MRI.
Diabetes
In chronic diabetes, bone infarcts are noted either due to arteriosclerosis/ microvascular disease or sub-clinical trauma [20]. The imaging characteristics are the same as in other entities (Figure 18).

Figure 18a,b: Bone infarct, diabetic 79 Y/O, note the fibroosseous membrane with sclerotic peripheral rim.
Caisson disease
The etiopathology of Caisson disease: accumulation of nitrogen gas in blood vessels. These act as emboli and produce bone ischemia, infarction and osteonecrosis. This phenomenon is noted in deep sea drivers who are removed too rapidly from a high pressure environment, less frequently from low pressure environments such as in high altitude flying. The entire syndrome has been called Decompression sickness (Figure 19) [21].

Figure 19: Caisson disease, bone infarction and osteonecrosis.
Fibrous dysplasia
Fibrous dysplasia associated with avascular head of the femur is extremely rare. But it has been reported in adults, but its association with Perthe’s is being described for the first time (Figure 20).

Figure 20: Fibrous dysplasia associated with Perthe’s disease of femoral head.
Conclusion
Bone ischemia and its imaging forms an interesting part of radiology where the ischemia manifests in increased density of bone in traumatic and infective diseases, collapse in different stages in osteonecrosis, and bone infarcts in long tubular bones. The identification by imaging methods is important. Each one of the above entities gives a different spectrum. There are numerous causes of ischemia but few imaging methods which include conventional, MRI and nuclide scan. The article is profusely illustrated with classical examples.
Acknowledgements
NIMS, KIMS and KREST, Hyderabad, India.
Conflicts of interest
Author declares no conflicts of interest.
References
[1] Olvi LG, Santini-Araujo E. Bone Infarct. In: Santini-Araujo E., Kalil R., Bertoni F., Park YK. (eds) Tumors and Tumor-Like Lesions of Bone. Springer, London, 2015. https://doi.org/10.1007/978-1-4471-6578-1_65
[2] Weerakkody Y, Dixon A. Bone infarction. Accessed from: https://radiopaedia.org/articles/bone-infarction-1
[3] Hacking C, Goel A. Snowcap Sign (Avascular Necrosis). – Accessed from: https://radiopaedia.org/articles/snowcap-sign-avascular-necrosis
[4] Osteonecrosis. Accessed from: https://rad.washington.edu/about-us/academic-sections/musculoskeletal-radiology/teaching-materials/online-musculoskeletal-radiology-book/osteonecrosis/
[5] Arnaiz J, Piedra T, Cerezal L, Ward J, Thompson A, et al. Imaging of Kienböck disease. AJR Am J Roentgenol. 2014; 203(1):131-139.
[6] Abdrabou A. Kummell Disease. Accessed from: https://radiopaedia.org/cases/kummell-disease-5
[7] Parvizi J. Avascular Necrosis. Accessed from: https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/avascular-necrosis
[8] Weerakkody Y, Stanislavsky A. Sickle Cell Disease. Accessed from: https://radiopaedia.org/articles/sickle-cell-disease
[9] James Reed J, Sosman MC. Gaucher’s Disease. Radiology. Accessed from: https://pubs.rsna.org/doi/10.1148/38.5.579
[10] Caramaschi P, Biasi D, Forno ID, Adami S. Osteonecrosis in systemic lupus erythematosus: an early, frequent, and not always symptomatic complication. Autoimmune Dis. 2012; 2012:725249.
[11] Bicer A. Musculoskeletal Findings in Behcet's Disease. Patholog Res Int. 2012; 2012:653806.
[12] Huntoon MA. Complications Associated with chronic steroid use. Accessed from: https://www.sciencedirect.com/science/article/pii/B9781416023920500364
[13] Wadhwa SS, Mansberg R. Multiple spontaneous bone infarcts secondary to alcohol abuse. Accessed from: https://inis.iaea.org/search/search.aspx?orig_q=RN:31037839
[14] Bell DJ, Weerakkody Y. Osteoradionecrosis. Accessed from: https://radiopaedia.org/articles/osteoradionecrosis
[15] Torrisi JM, Schwartz LH, Gollub MJ, Ginsberg MS, Bosl GJ, et al. CT findings of chemotherapy-induced toxicity: what radiologists need to know about the clinical and radiologic manifestations of chemotherapy toxicity. Radiology. 2011; 258(1):41-56.
[16] Gerle RD, Walker LA, Achord JL, Weens SH. Osseous changes in chronic pancreatitis. Radiology. Accessed from: https://pubs.rsna.org/doi/pdf/10.1148/85.2.330
[17] Schabel SI, Korn JH, Rittenberg GM. Bone infarction in gout. Skeletal Radiol. 1978; 3:42–47.
[18] Bone Infarction. Accessed from: https://radiologykey.com/bone-infarction
[19] Lopez-Ben R, Mikuls TR, Moore DS, Julian BA, Bernreuter WK, et al. Incidence of hip osteonecrosis among renal transplantation recipients: a prospective study. Clin Radiol. 2004; 59(5):431-438.
[20] Baker JC, Demertzis JL, Rhodes NG, Wessell DE, Rubin DA. Diabetic Musculoskeletal Complications and Their Imaging Mimics. RadioGraphics. Accessed from: https://pubs.rsna.org/doi/full/10.1148/rg.327125054
[21] Osteochondritis, Caisson disease, Caffey’s disease. Accessed from: https://pt.slideshare.net/airwave12/osteochondritis-dessicans-caisson-disease-caffeys-disease