Full Text
Introduction
A cyst is defined as a fluid containing sac, lined by epithelium and surrounded by connective tissue. It may have a capsule and may also have semisolid contents. The dental parts of mandible and maxilla are generally dealt by department of dental sciences. However, the bony part is also most important and should be studied imageologically, since some of the lesions of the jaws are not related to teeth only [1-5]. Radiological differentiation of these lesions is important in order to manage these. In practice, mandibular lesions are more common than maxillary. Radiologically, the term ‘cystic’ should not be confined only to completely lytic or lucent lesions. Solid radio lucent lesions may also appear imageologically lytic/lucent and are called cystic.
These cystic lesions may be classified in the following manner (Table 1). The more common cystic lesions of the mandible include periapical (radicular) and follicular (dentigerous) cysts [6-8]. Next in common include odontogenic keratocyst (OKC), Stafne (static bony cavity) cyst [9] and solitary bone cysts which include post traumatic cysts, simple or hemorrahagic. The rare cyst like or pseudo cystic lesions include ameloblastoma, fibrous dysplasia, ossifying fibroma, brown tumor etc [10, 11] (Table 2). Classification of the cysts of the jaw as defined by WHO in 1992 (Table 1).
Table 1: True cystic lesions (Modified list of WHO).
- Radicular cyst (Periapical cyst)
- Odontogenic Keratocyst
- Dentigerous (follicular) cyst
- Residual cyst
- Odontogenic cyst
- Incisive Canal Cyst
- Solitary bone cyst
- Aneurysmal bone cyst
- Stafne cyst
- Medullary pseudo cyst
|
In the differential diagnosis, the following cyst like lesions should be considered (Table 2).
Table 2: Cyst like lesions.
- Ameloblastoma
- Fibrous dysplasia
- Ossifying fibroma
- Giant cell tumor
- Giant cell reparative granuloma
- Brown tumor
- Hemangioma
- Peri apical abscess
- Traumatic bone cyst
- Langerhans histocytosis
|
Imaging methods
- Conventional radiology
- Intraoral and occlusive
- Orthopantomogram (OPG)
- Conventional CT
- Cone beam CT (CBCT)
- Magnetic resonance imaging (rarely used)
Imaging characteristics
Radicular cyst (Periapical cyst)
This is the most common cyst and is seen with relationship to the apex of the tooth. Radiologically, a poorly defined para-apical area of lucency is noted. Its sclerotic margin is continuous with lamina dura of the periphery of the cyst. The size of the cyst varies between 0.5 to 1.5cms in diameter (Figure 1 a,b). They may be multiple.

Figure 1: Orthopantomogram, radicular cyst, (a) Solitary, (b) Multiple.
Odontogenic keratocyst
This is a keratonised cyst and generally follows cystic degeneration of the enamel organ prior to the formation of tooth. Hence, it replaces the tooth. It is most commonly located in the body and ramus of the mandible and when multiple may also occur in the anterior mandible or anywhere in the maxilla.
Imaging features
Imaging wise, thinning of the cortex surrounding the lucency is noted commonly located in the posterior part of the mandible (Figure 2 a,b). These may be multiple which are generally associated with ‘Gorlin–Goltz syndrome’ consisting of multiple nevoid – basal cell carcinoma and keratocysts (Figure 2c).
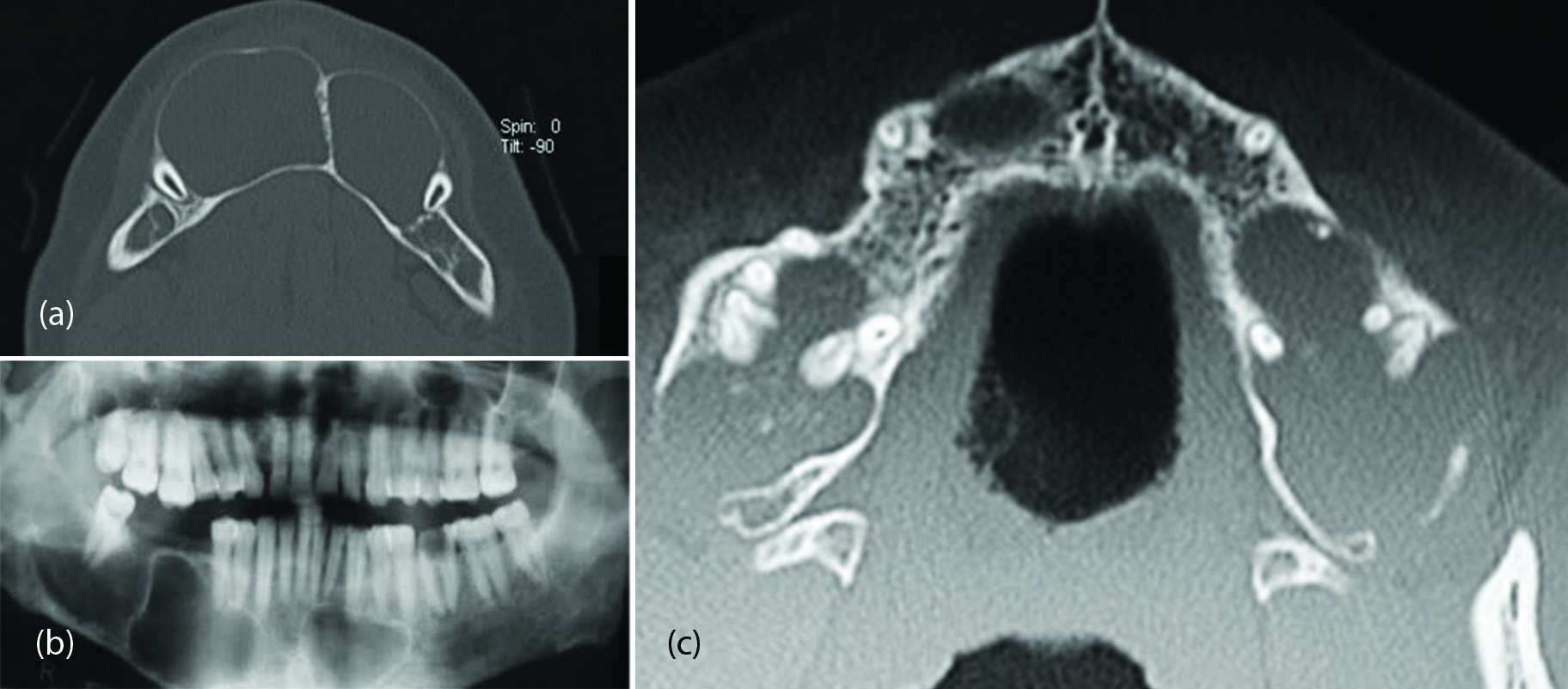
Figure 2: (a) Odontogenic keratocysts in the mandible, (b) CT, (c) Multiple keratocysts in maxilla in a patient with Gorlin–Goltz syndrome.
Dentigerous cyst or follicular cyst is a slow growing, benign and non-inflammatory odontogenic cyst, thought to be of developmental origin. It is associated with the crown of an unerupted (or partially erupted) tooth. The cyst cavity is lined by epithelial cells derived from the reduced enamel epithelium of the tooth forming organ. It is the 2nd most common odontogenic cyst after radicular cyst. Dentigerous cysts are the most common developmental cysts of the jaw, frequently associated with impacted third molar tooth. Bilateral dentigerous cysts are rare and occur typically in association with a developmental syndrome. It is encountered more in males than in females and is most common in an unerupted mandibular 3rd molar. It may also involve maxillary canine, mandibular premolar, maxillary 3rd molar and supernumerary teeth.
Imaging features
It is usually unilocular and well-defined lucent lesion with sclerotic margins. It is associated with crown of unerupted or impacted tooth. Larger cysts cause cortical expansion leading to facial asymmetry, tooth displacement and root resorption (Figure 3a-d). Persistence of bony trabeculae is seen in larger cysts giving multiloculated appearance.

Figure 3: Dentigerous cyst CT, (a, b) Mandibular, (c, d) Maxillary.
Odontogenic myxoma
It is a rare mandibular tumor, which is benign but locally aggressive. It rarely appears in bones other than the jaws. It is considered to be derived from the mesenchymal portion of the tooth germ. Radilogically, a multiloculated cystic lesion displacing the teeth (Figure 4). The diagnosis is made only by histological features.
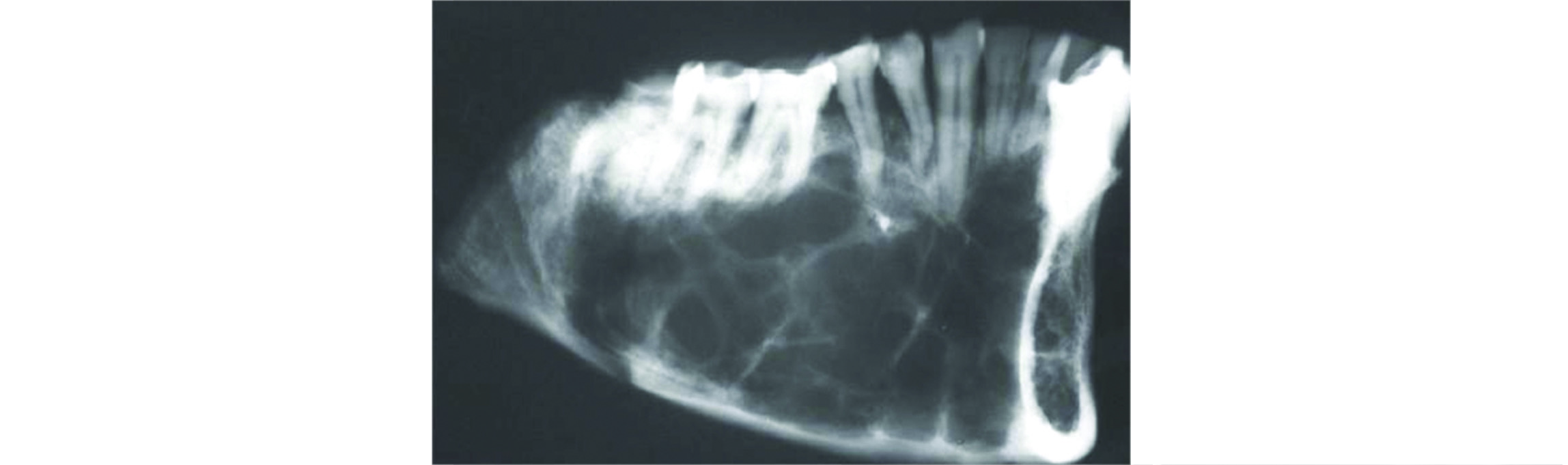
Figure 4: Odontogenic myxoma.
Residual cyst occurs due to incomplete surgical removal of a radicular or other inflammatory cyst. The histological and clinical features of the residual cyst are very similar to that of the radicular cyst except for the site of the extracted teeth. The radiographic feature is a well-defined unilocular radiolucent structure of varying size at the edentulous area of a previous extracted tooth site (Figure5).
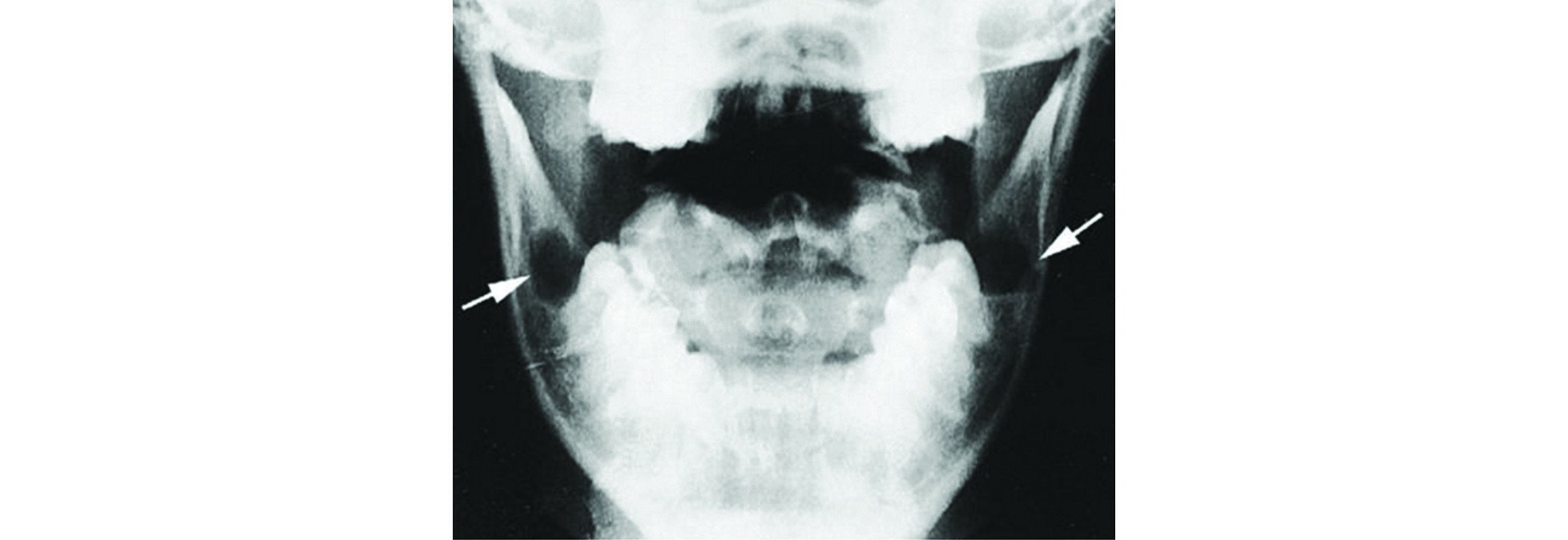
Figure 5: Residual cysts – Post tooth extraction.
Odontogenic cyst
This is also called lateral periodontal cyst (Botryoid cyst). The origin of this cyst is believed to be related to proliferation of rests of dental lamina. Radiologically, this lucent cystic lesion is placed in between two teeth (Figure 6).
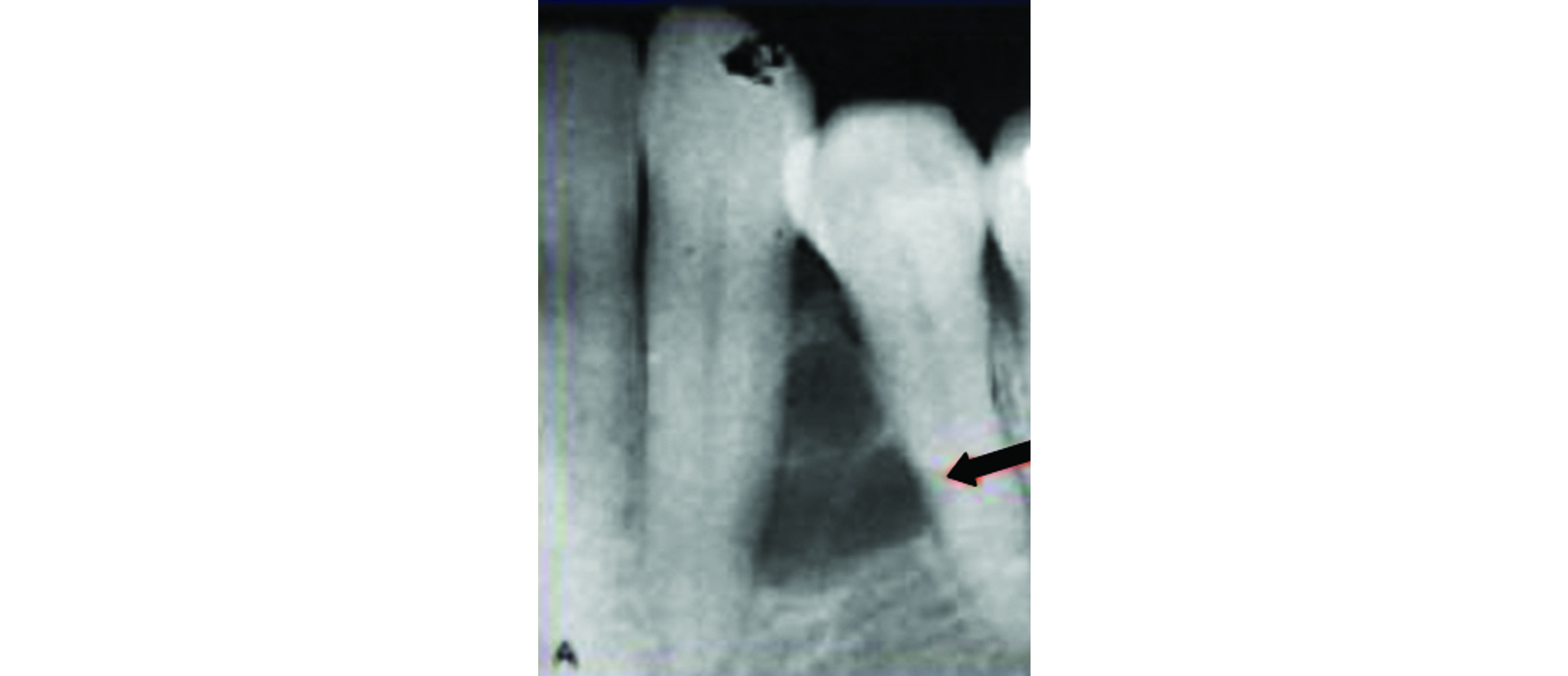
Figure 6: Odontogenic cyst.
Incisive canal cyst
It is also called median anterior maxillary cyst or nasopalatine duct cyst. It is located near the incisive canal, arising from proliferation of epithelial remnants of the asopalatine duct and is the most common maxillary developmental cyst. Radiologically, the size varies from few millimetres to 1centimetre. It is lucent and doesn’t contain any calcific material (Figure 7). It may be round or oval in shape.
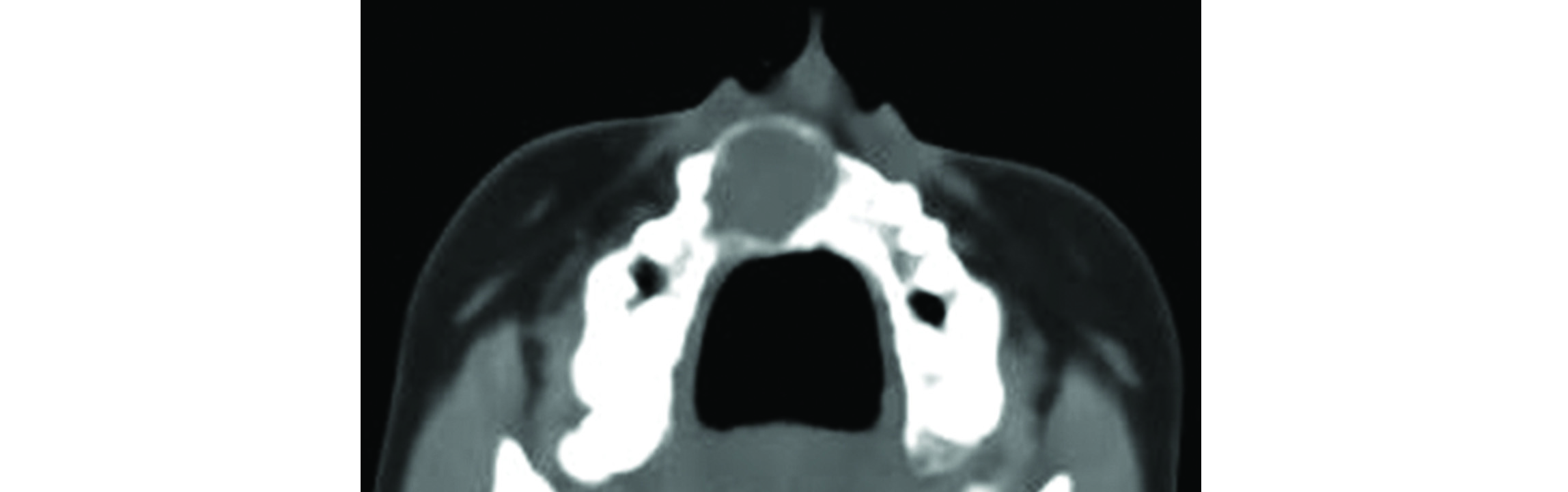
Figure 7: Incisive canal cyst.
Ameloblastoma
Ameloblastoma is the most frequent odontogenic neoplasm. It occurs most often in the mandible, particularly posteriorly. The common type of ameloblastoma is the conventional or solid-multicystic type. The most common pattern is follicular. The classical imaging appearance is a multilocualted (80%), expansile "soap-bubble" lesion with well demarcated borders and without matrix calcification (Figure 8a-d). Occasionally erosion of the adjacent tooth roots can be seen which is highly specific. When larger, it may also erode through cortex and extend into adjacent soft tissues. Although histologically four types have been described, it is difficult to differentiate them imageologically.
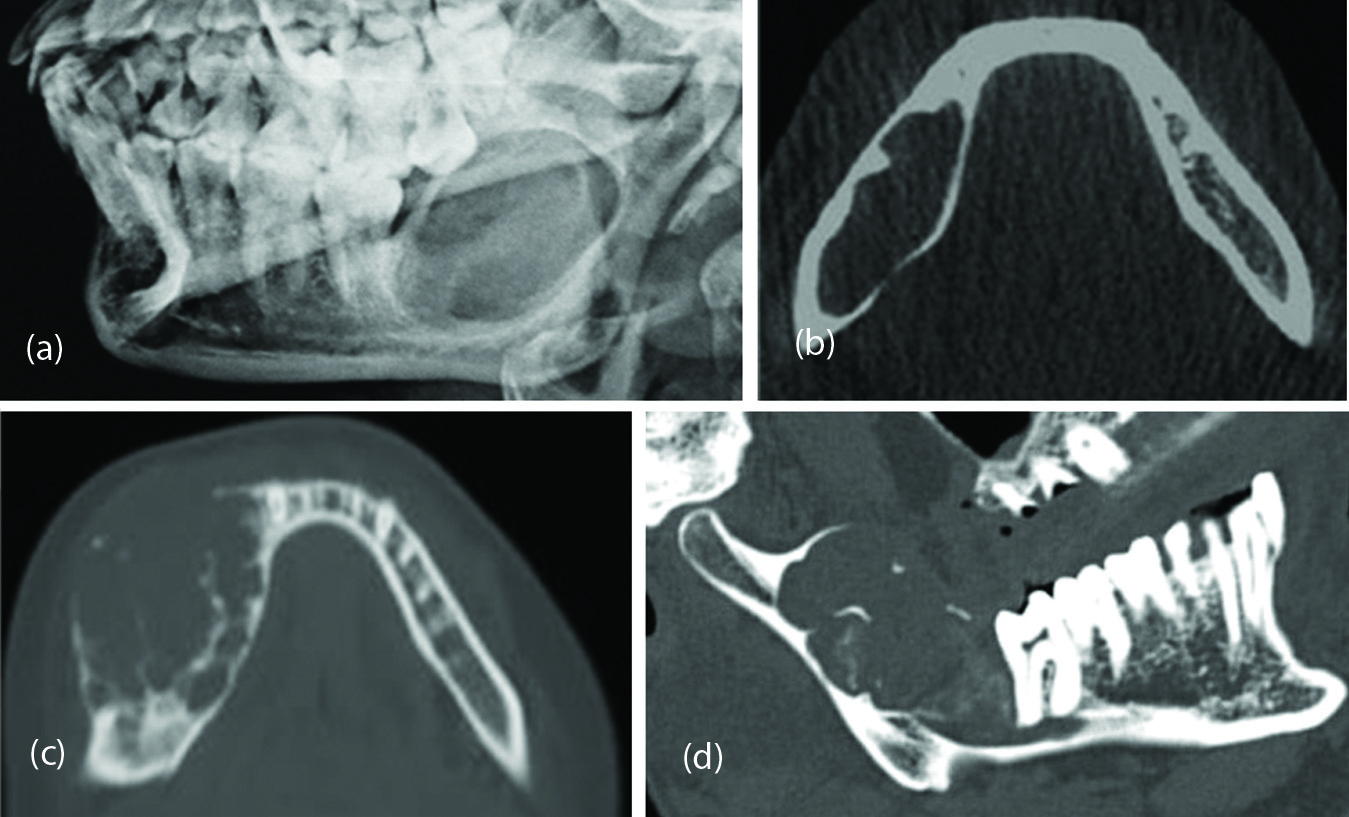
Figure 8: Ameloblastoma, (a) plain radiograph, (b, c, d) tomographs.
Fibrous dysplasia of the jaws
It is most common skeletal dysplasia and can be monostotic, polyostotic and may be associated with other syndromes. Cherubism is considered to be a variant of fibrous dysplasia, but it is a distinct entity. Clinically, it presents as a symmetrical bilateral jaw swelling with angelic facies. Radiologically, the features include lucent expanded regions within the maxilla and mandible, with soap-bubble appearance (Figure 9 a,b). As age advances, it may become sclerotic and may reduce in size. Fibrous dysplasia of the maxilla and mandible may be part of generalized skeletal fibrous dysplasia. Isolated cases of fibrous dysplasia of jaws are rare. The radiological appearances vary. However, the classical appearance is a cystic lesion with well defined sclerotic rind, with a groundglass matrix of variable densities (Figure 9c).

Figure 9: Cherubism, (a) maxilla, (b) mandible showing expanding bubbly lesions, (c) Fibrous dysplasia of the mandible.
Ossifying fibroma
Ossifying fibroma is also known as cementifying fibroma. It consists of fibrous tissue with variable amounts of bony trabeculae. Two clinicopathological variants are known, a conventional slow growing ossifying fibroma which are encountered in 3rd and 4th decades of life and an aggressive juvenile ossifying fibroma in early years. Most of these lesions are located in the posterior part of the mandible. Radiologically, a well encapsulated circumscribed lesion with variable radio density is present. It may be completely radiolucent or completely sclerotic or with mixed densities (Figure 10).

Figure 10: Ossifying fibroma of the mandible.
Giant cell tumor and giant cell reparative granuloma
Giant cell tumor is common in long bones and is a benign neoplastic process. Occurrence in the jaws is very rare. However, giant cell reparative granuloma is a little more common than giant cell tumors of the jaws. It is an aggressive proliferative intraosseous lesion consisting of fibrous tissue, hemorrhage and giant cells and is more common in young girls. This is often found in the anterior part of mandible and is central. Radiologically, early lesion appears as a small well defined radiolucent lesion simulating odontogenic cyst. Later it appears as a multilocular lucent lesion with tiny bony trabeculae traversing the lesion (Figure 11). It is difficult to differentiate it from giant cell tumor and odontogenic tumors.
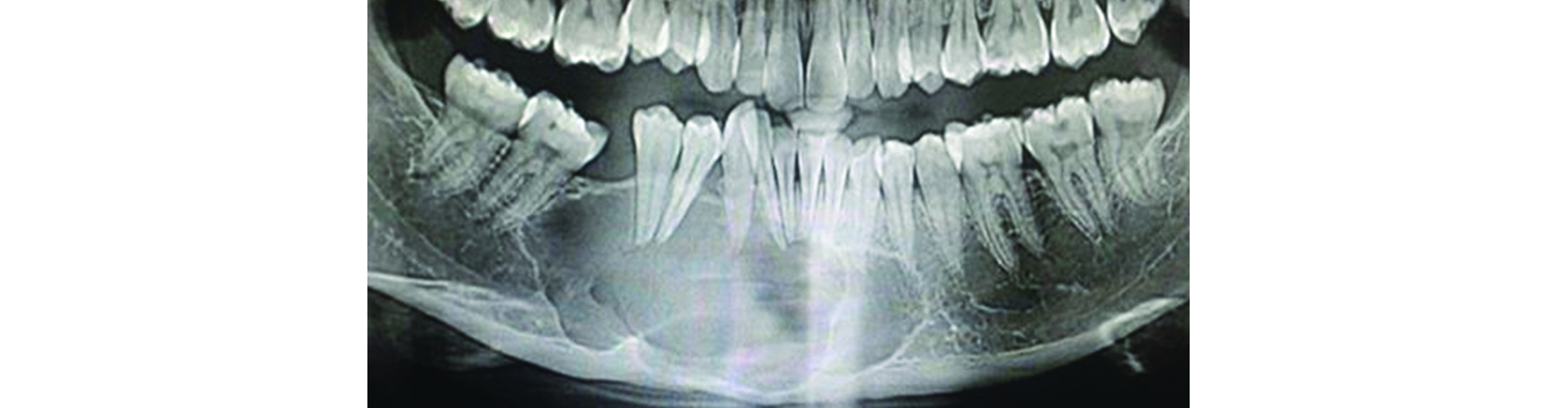
Figure 11: Giant cell reparative granuloma of the mandible.
Brown tumor
The name derives from the cross sectional appearance of this lesion which is brown because of the hemorrhage mixed with fibroblasts and giant cells. They are common in primary and secondary hyperparathyroidism. They can occur anywhere, although it is unusual in the jaw bones. The diagnosis is confidentially made by added finding of the absence of lamina dura of the teeth (Figure 12).

Figure 12: Brown tumors of primary hyperparathyroidism.
Hemangioma
It is the most common benign vascular tumor of the bones. Although, it is common in the vertebral bodies, but can occur in any bone. Hemangioma of the jaw bones is rare. Radiologically, a spoke wheel appearance with thickened trabeculae is common. These may be capillary, cavernous, mixed or venous (Figure 13a, b).

Figure 13: Hemangioma of mandible, (a) Orthopantomogram, (b) Conventional radiograph.
Periapical cyst
Periapical cyst is also known as radicular cyst, is the most frequent cystic lesion related to teeth and results from infection of the tooth. On imaging, they generally present as round or pear-shaped, unilocular, lucent lesions in the periapical region, measuring <1 cm. This is also called periapical granuloma (Figure 14a). This should be differentiated from tooth abcess (Figure 14b).

Figure 14: (a) Multiple periapical cysts at the roots of the teeth, (b) Tooth abscess.
Traumatic bone cyst (TBC)
It is also known as simple cyst or hemorrhagic cyst. This is an uncommon nonepithelial lined lucent cavity of the jaws. The lesion is mainly diagnosed in young patients most frequently during the second decade of life. The majority of TBCs are located in the mandibular body between the canine and the third molar.
Stafne cyst
Stafne cyst is also known as “lingual salivary gland inclusion defect’’. It is a cortical defect near the angle of mandible below the mandibular canal (Figure 15).
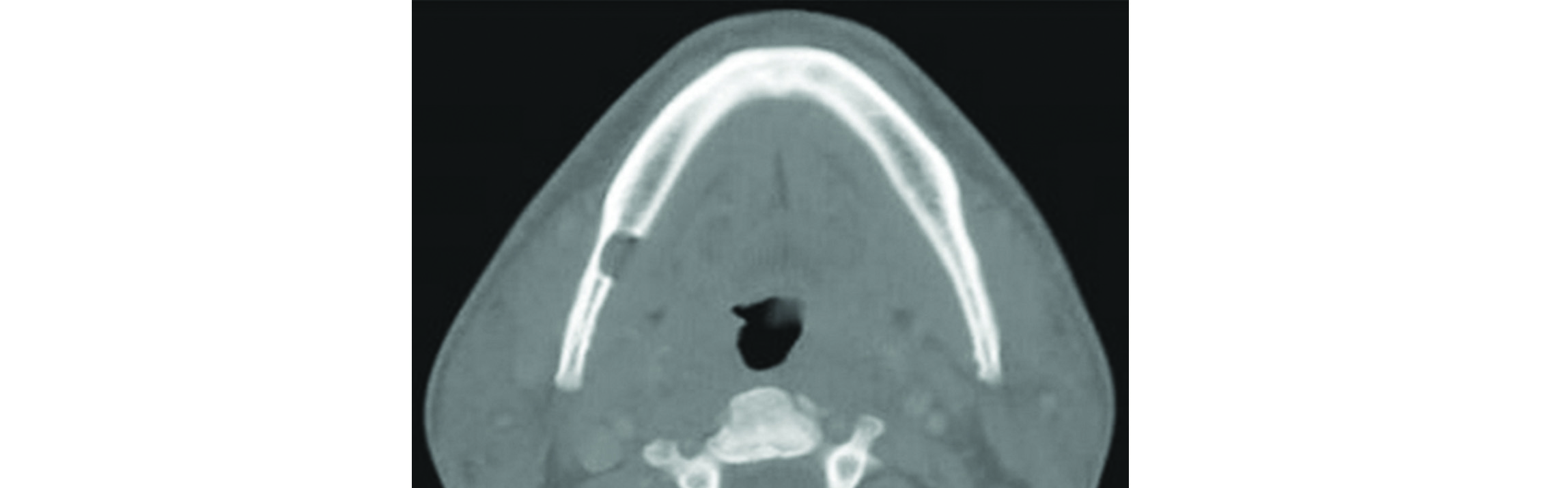
Figure 15: Stafne cyst of the mandible.
Langerhans cell histiocytosis is a complex syndrome with three subtypes, 1. Eosinophilic granuloma, 2. Hand-schuller Christian disease and 3. Letterer-siwe disease. It is a rare multi system disease and the incidence in India is not known. This term is replaced by the older term, Histiocytosis X. The etiology is unknown although, various theories have been proposed. Of these, eosinophilic granuloma is common. It may be monostotic or polyostotic and may occur at any age. Skull and jaw bones are common sites. Radiologically, a lucent lesion with bevelled edges and floating teeth are common manifestations (Figure 16a, b).
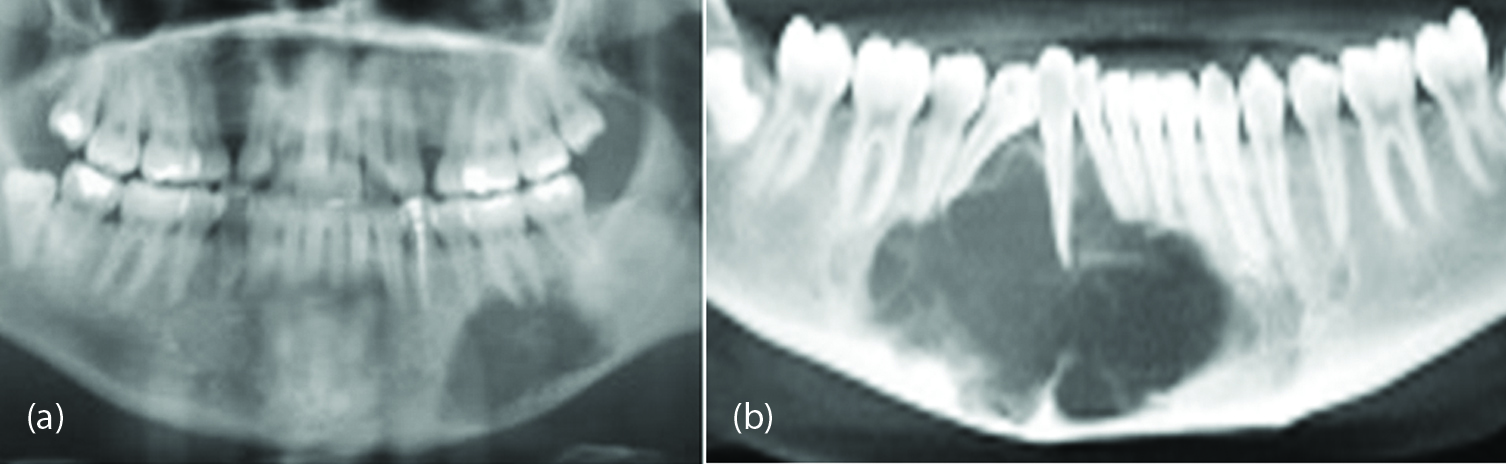
Figure 16: Langerhans cell histiocytosis, (a) Mandible, (b) With a floating tooth.
Aneurysmal bone cyst (ABC)
This may be primary or secondary most commonly seen in metaphyses of long and flat bones. These rare jaw lesions are encountered in the body and ramus of the mandible. It is commonly reported in the second and third decades of life, ABC's are characterized by a rapid growth pattern with resultant bony expansion and facial asymmetry. A large lucent lesion without any mineralisation of the matrix is a common feature (Figure 17). In secondary ABC’s, the benign primary lesions include giant cell tumor, osteoblastoma and chondroblastoma. On CT and MRI imaging, the presence of fluid fluid levels is characteristic.
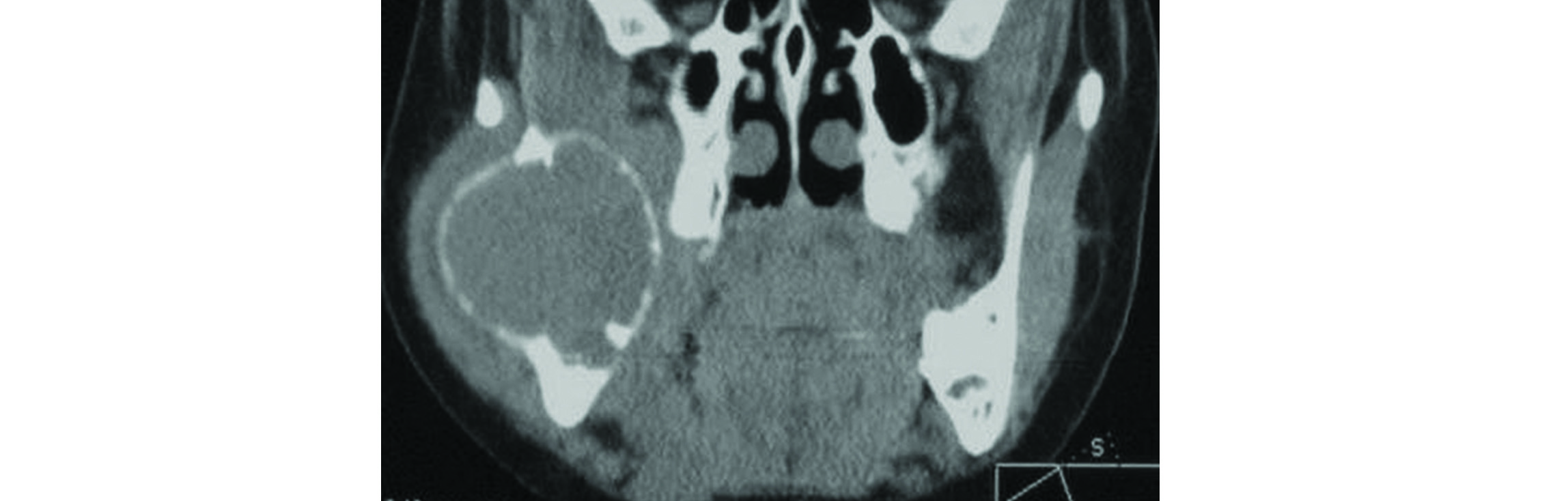
Figure 17: Aneurysmal bone cyst of mandible.
Conclusion
Cystic and predominantly lucent lesions of the jaws are relatively common. They may be odontogenic or non-odontogenic. Imaging characteristics of these are described in detail. Conventional radiology, orthopantomogram, CT and coned beam CT are the usual methods to arrive at a diagnosis. Cyst like lesions are many and their imaging findings are also described.
Acknowledgements
NIMS, Hyderabad, and Krest Museum, Shaikpet, Hyderabad, India.
Conflicts of interest
Author declares no conflicts of interest.
References
[1] Weber AL, Kaneda T, Scrivani SJ, Aziz S. Jaw: cysts, tumors and nontumorous lesions. In: Som PM, Curtin HD, eds. Head and neck imaging, 4th ed. St. Louis, MO: Mosby, 2003:930–994.
[2] Raviraj Patel Yasin Vaja Guided By: Dr. Tarnjeet Kaur, Department Of Oral and Maxillofacial Surgery, Gov. Dental College And Hospital, Jamnagar. PowerPoint Presentation.
[3] Scholl RJ, Kellett HM, Neumann DP, Lurie AG. Cysts and cystic lesions of the mandible: clinical and radiologic-histopathologic review. Radiographics. 1999; 19(5):1107-1124.
[4] Manor E, Kachko L, Puterman MB, Szabo G, Bodner L. Cystic lesions of the jaws - a clinicopathological study of 322 cases and review of the literature. Int J Med Sci. 2012; 9(1):20–26.
[5] Kramer IRH, Pindborg JJ, Shar M. Histological typing of odontogenic tumors, In: WHO – International histological classification of tumors. 2nd ed. Berlin, Germany: Springer – Verlag, 1992; 1–42.
[6] Prof Frank Gaillard et al., Mandibular lesions; Available at https://radiopaedia.org/articles/mandibular-lesions
[7] Resnick D, Kyriakos M, Greenway GD. Tmors and tumor like lesions of bone: imaging and pathology of specific lesions. In: Resnick D, ed. Diagnosis of bone and joint disorders. 4th ed. Philadelphia, Pa: Saunders, 2002; 3763–4128.
[8] Yoshiura K, Weber AL, Runnels S, Scrivani SJ. Cystic lesions of the mandible and maxilla. Neuroimaging Clin N Am. 2003; 13(3):485–494.
[9] Stafne EC: Stafne’s radiographic diagnosis (5th edition) : Philadelphia: WB Saunders, 1985.
[10] Eversole LR, Rovin S. Differential radiographic diagnosis of lesions of the jawbones. Radiology 1972;105:277–284.
[11] Dunfee BL, Sakai O, Pistey R, Gohel A. Radiologic and pathologic characteristics of benign and malignant lesions of the mandible. Radiographics. 2006; 26(6):1751–1768.