Full Text
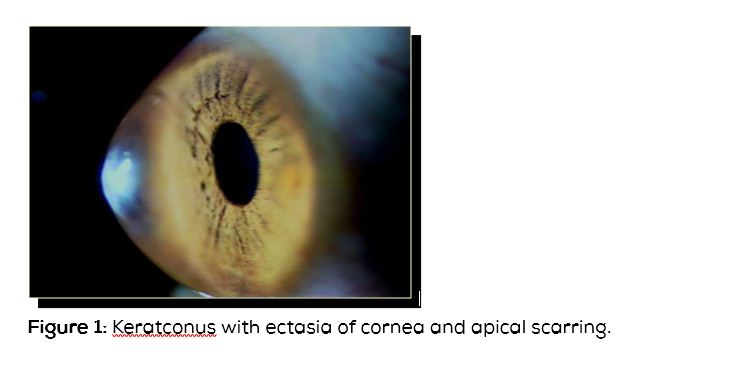
Keratoconus is a corneal thinning disorder in which the inferior paracentral cornea thins and protrudes forwards (Figure 1). Though keratoconus commonly involves inferior paracentral cornea, cases of superior keratoconus are also available in literature. The reported incidence of keratoconus is 1:1000 to 1:20000 [1]. Keratoconus seems to be commoner in Asians where it is of early onset and severe in nature. The onset is usually during the second decade [2]. The disease affects the quality of vision and hence causes reduced quality of life.
Presenting symptoms
Blurred vision and frequent changes of spectacle power are the common presenting symptoms.
Eye rubbing
In addition to heredity, there seems to be an association of eye rubbing and development of keratoconus. It looks like eye rubbing is also involved with progression of keratoconus and development of acute corneal hydrops [3].
Various reasons for eye rubbing in keratoconus patients are as follows: 1) Some patients of keratoconus say they rub their eyes as they felt it would improve their vision, 2) Patients of vernal keratoconjunctivitis and severe ocular allergy rub their eyes vigorously and later develop keratoconus (Figure 2). In patients with severe ocular allergy, topographic indices are found to be abnormal [4]. Any patient with myopic astigmatism should be followed up carefully for the development of keratoconus if they have severe allergy, 3) Lid margin disease – patient rub their eye because of irritation and itching, 4) Patients with Leber’s congenital amaurosis develop keratoconus as these patients rub their eyes to stimulate their retina, 5) Down’s syndrome patients rub their eyes as they are mentally retarded [5], 6) Oculodigital reflex - we have seen a child with acute corneal hydrops in left eye, right eye being absolutely normal. History revealed, child had habit of sucking the left thumb and whenever she sucks her thumb, she keeping on pressing the left eye with index finger.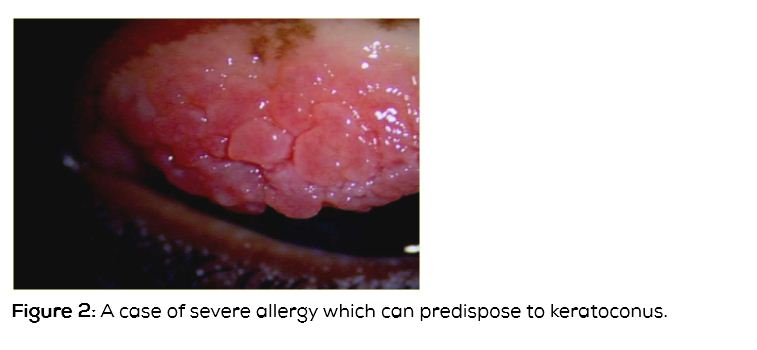
Clinical features
Any myopic astigmatism which is increasing or vision not improving to 6/6 or 20/20 should be suspected to have keratoconus.
Signs
a) Refraction: i. Myopic astigmatism, ii. Scissors reflex because of areas of myopic and hyperopic refraction, Slit lamp features showing the clinical findings on slit lamp examination drawings), b) Thinning of inferior paracentral cornea, c) Protrusion or ectasia of inferior cornea, d) The area of thinned ectatic Cornea is in the form of cone. Cones in keratoconus can be round/nipple shaped, oval/ sagging and global if the entire cornea is involved. In oval or a sagging kind of cone, a large area of ectatic thin cornea touching the limbus may be seen. In global type, the entire cornea is conical [6], e) Vogt’s stria-these are stria or folds just in front of Descemet’s membrane. They disappear on pressure over the eye, f) Apical sub-epithelial and Descemet’s level scarring, g) Increased visibility of endothelial reflex, h) Prominent corneal nerves, i) Fleischer's ring is deposit of iron in the base of the cone. Fleischer's ring is important for corneal surgeons as entire thinned cornea needs to be excised during surgery. If residual thinned Cornea is left, then significant astigmatism may remain following surgery requiring glasses or contact lens after surgery, h) Munson's sign – On looking down, the cone divides the lower lid margin (Figure 3), i) Rizzuti sign – When a torch light is thrown from the temporal side, in a normal cornea the nasal and the temporal cornea is equally illuminated. In a conical cornea, the light focused by the cone is seen as a vertical line on the nasal iris, j) Keratometry – Steep cornea. Any keratometry reading of more than 47 diopters should be carefully looked at. In keratoconus, the keratometer mires are malformed and in severe cases, may not be opposed, k) Topography - Any patient with topographic evidence of keratoconus with no clinical features is labelled as forme fruste keratoconus. Any island of steepening of inferior cornea should be suspected to have early or forme fruste keratoconus. Any patient with central cornea of more than 47D, difference in central cornea between the two eyes of more than 1D and difference between inferior and superior cornea at equidistant points of more than 1D should be suspected of keratoconus. Various indices including the Rabinowitz index and Klyce Maeda index are available to detect forme fruste keratoconus [6].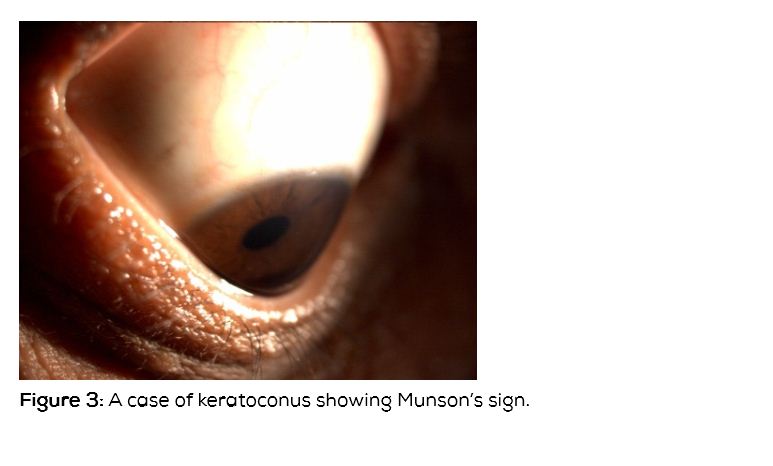
In addition to steep cornea in keratoconus, asymmetrical bow tie pattern of astigmatism with skewed radial axis are important topographic features of keratoconus.
Ocular and systemic associations of keratoconus
Though there a number of associations reported the following are seen in practice more often Retinitis pigmentosa, Leber's optic atrophy, and Ocular allergy including vernal keratoconjunctivitis
Systemic associations are Marfan’s syndrome and Ehler Danlos syndrome
Acute corneal hydrops
This is corneal edema happening in a patient with keratoconus. This occurs as a consequence of rapid progression of keratoconus resulting in Descemet's membrane tear. The cornea is swollen resulting in stromal edema and epithelial edema. Patient presents with rapid onset of loss of vision. Slit lamp examination will reveal tear in Descemet's membrane which may be centrally located or may extend to the peripheral cornea. Stromal cleft may be visible [7] (Figure 4). Anterior segment optical coherence tomography (OCT) will help to visualize Descemet's membrane tear in cases where it is not visible on slit lamp and also helps to find the dimensions of tear including the depth of the tear.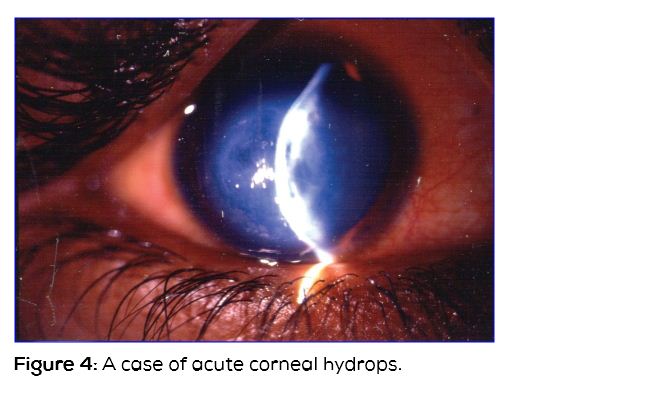
Management
For visual rehabilitation options are 1) Glasses, 2) Contact lenses, 3) Intra corneal rings, 4) Deep anterior lamellar keratoplasty (DALK), 5) Large or eccentric penetrating keratoplasty, 6) Large lamellar keratoplasty followed by penetrating keratoplasty, 7) Implantable contact lens – Spherical and toric.
General measures are avoiding eye rubbing, frequent washing of eyes, in allergy cases. Cold compression is suggested for relief of symptoms
1) Spectacles regular or toric spectacles are useful in mild cases, 2) Contact lens - In the initial stages, soft contact lens may be of use. Rigid gas permeable (RGP) lenses are recommended contact lenses in keratoconus patients with mild to moderate astigmatism. These lenses give good quality vision and also have minimal dryness and inflammation in patients using lenses for many years. Specially designed lenses like Rose K lenses are also useful. Rose K lenses have additional blends helping the contact lenses to stay on the cornea even in severe coning of cornea. In severe ectasia, piggy back contact lens, where in a small RGP contact lens is applied over a large soft lens. Softperm lens have central RGP with a peripheral skirt of soft lens help in similar situation. Scleral lens RGP lenses can be used in large ectasia. Scleral RGP contact lenses are large contact lenses which sit on the sclera, so that even in severe ectasia the patient is to be visually rehabilitated if the central cornea is clear [8].
3) Intracorneal ring segments- Implantation of PMMA intracorneal rings into the paracentral cornea has been found successful to reduce the spherical and astigmatism error [9]. These rings work on the principle of adding material on paracentral cornea to flatten the central cornea [10]. Intacs or Ferrara are the common prototypes of intracorneal rings available. The central cornea needs to be clear and the cornea needs to be at least 400 microns in thickness. The procedure involves making an incision with diamond knife, dissecting the grooves with a mechanical device or with a femtosecond laser. The incision is sutured at the end of surgery. The steps of surgery are shown in (Figure 5).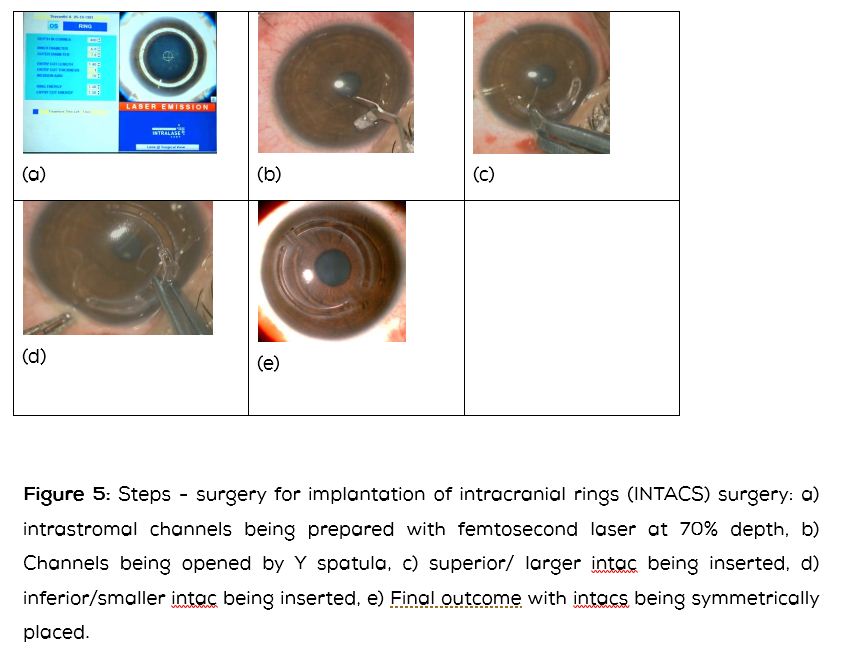
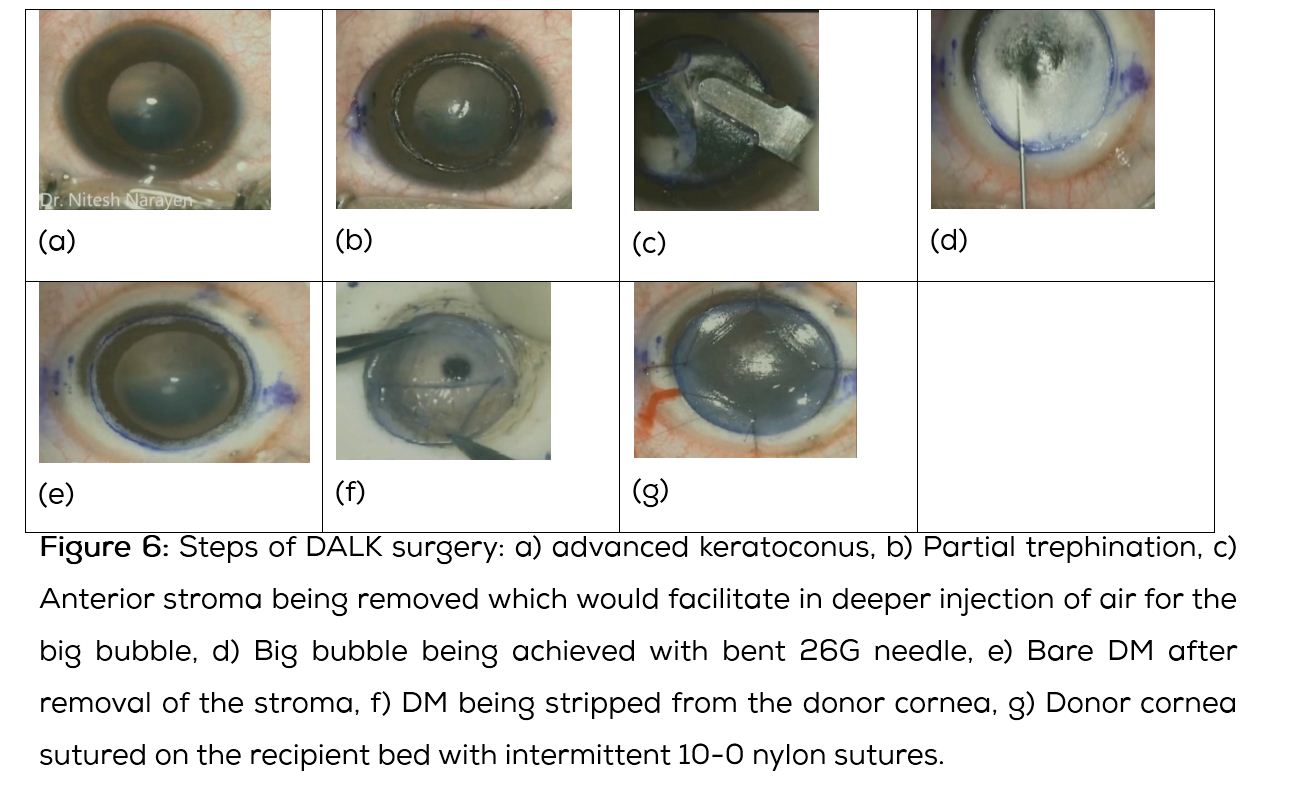
4) Deep anterior lamellar keratoplasty (DALK) - Since endothelium is relatively healthy, DALK is becoming the surgery of choice for patients who are not having good vision with contact lens or are not able to tolerate contact lens for a long time or if the contact lens is popping out often.
In this procedure, the dissection is performed at the level of Descemet’s membrane by injecting air bubble (viscoelastic) in front of Descemet’s membrane. The tissue in front of the Descemet’s membrane is carefully dissected (by a combination of blunt and sharp) and removed. The donor cornea is transplanted after removing the endothelium. The steps are shown in Table 6. DLAK can be performed even following hydrops with faint scar.
The advantages of DALK over full thickness penetrating keratoplasty include 1) we are leaving behind relatively healthy endothelium of patient 2) hence donor endothelium is not transplanted with less incidence of endothelium rejection and failure 3) Open eye situation with its disastrous consequences is avoided during surgery [11, 12].
5) Penetrating keratoplasy (PK)- This is suggested in patients with dense central scar which is deeper and involving the Descemet’s membrane. The principle of surgery is to excise the cone in totality. Fleischer’s ring on slit lamp shows base of the cone. Normally during transplantation graft of 0.5 mm or more is taken than the recipient bed. But in patients with keratoconus same sized graft or a donor cornea 0.2 mm more is preferred to reduce post-op myopia [13].
If the cone is sagging, oval or extending to periphery, a large eccentric penetrating keratoplasty can be considered. In this situation, the graft host junction coming close to the limbus needs to be carefully watched for loose sutures. Intraocular pressure needs to be monitored closely.
6) In patient with extensive limbus to limbus ectasia, a thin lamellar keratoplasty followed by a central PK may be done. If the thinning is limbus to limbus, performing lamellar keratoplasty may be technically very difficult. Removing the epithelium and putting a epikeratophakia kind of lenticule may be an alternate option.
7) Toric implantable contact lens (ICL) is useful in patients with high myopia and astigmatism. This option may be considered if the keratoconus is stable or is the progression is arrested by doing collagen cross- linking [15] or the irregular astigmatism is reduced with improvement of visual acuity on post implantation intracranial ring segments [16]. The central cornea needs to be clear with no scarring. The natural lens should be clear. It is easy to implant the ICL as the anterior chamber is deep [14].
Collagen cross linking
In keratoconus there is change in the intrinsic biomechanical properties of the corneal collagen. Collagen cross linking uses photosensitizer riboflavin and UVA 370nm. The photosensitizer is activated into its triplet state, generating reactive oxygen and to lesser degree superoxide anion radicals. The reactive oxygen can react further with various molecules including chemical covalent bonds thus bridging anion groups of collagen fibrils. The wavelength of 370nm has been chosen because it is the absorption peak of riboflavin [17]. The cross linking is formed maximum at the anterior 300 microns [18]. Topographic guided PRK can be performed at the same sitting or at a later stage for residual refractive error correction.
Minimum of 400 microns corneal thickness is required for collagen cross linking using isotonic riboflavin. If the thickness is low, endothelial toxicity may happen. If the corneal thickness is low, hypotonic riboflavin is used till about 360 microns. Using hypotonic riboflavin, cornea is swollen, corneal thickness measured and then the procedure is performed.
The procedure is performed under topical anesthesia. The corneal epithelium is removed with a blunt spatula or multiple tiny incisions are made. The cornea is soaked with riboflavin. A 0.1% riboflavin solution (10 mg riboflavin-5-phosphate in 10 ml dextran 20% solution) is applied every 5 min starting 5 min before the irradiation. The irradiation is performed from a 1 cm distance for 30 min using a UVA double diode at 370 nm and an irradiance of 3mW/cm2(equal to a dose of 5.4J/cm2). The required irradiance is controlled/ calculated in each patient directly before the treatment, to avoid a potentially dangerous UVA overdose. In regular procedure, 30 minutes of riboflavin soaking and 30 min of UV exposure is done. In accelerated riboflavin procedure using Avedro machine, the soaking time is 20 minutes with UV exposure of 4 min [19].
Corneal hydrops
This is a rare complication of keratoconus and other ecstatic disorder including pellucid marginal corneal degeneration (PMCD) and keratoglobus. In this condition, the Descemet's membrane ruptures, causing stromal edema and diminution of vision. Early onset of keratoconus and eye rubbing seems to predispose individuals to develop corneal hydrops [2].
Management
Cycloplegic and antibiotic ointment at bed time, intra cameral injection of air, SF6 or C3F8 gas has been found to enhance the resolution of hydrops [20]. Following resolution of corneal hydrops central cornea gets flattened and it may become possible to fit contact lens. In case there is significant central and dense corneal opacity corneal transplant may be required.
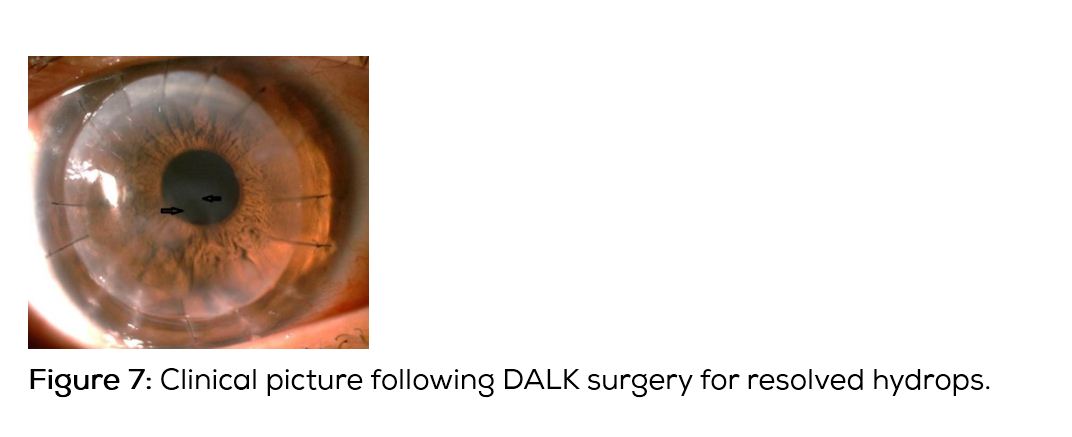
DALK can also be performed in cases of resolved hydrops with good visual results [21, 22] (Figures 6 and 7).
Differential diagnosis of keratoconus
1) Pellucid marginal corneal degeneration (PMCD) - There is an inferior band of narrow thinning and ectasia of the normal cornea above it (Figure 8). Though PMCD is normally seen inferiorly it is also seen in nasal and temporal cornea. On topography there is characteristic red band of steepening which goes across the nasal and temporal hemimeridians to form a loop cylinder; against the rule astigmatism with inferior loop cylinder is seen in PMCD. When the topography ring does not reach the entire cornea a butterfly pattern is seen. 2) Keratoglobus- There is limbus to limbus thinning and protrusion of the entire cornea. 3) Posterior keratoconus- In this situation, the anterior surface of cornea is normal. Ectasia of only posterior cornea is seen.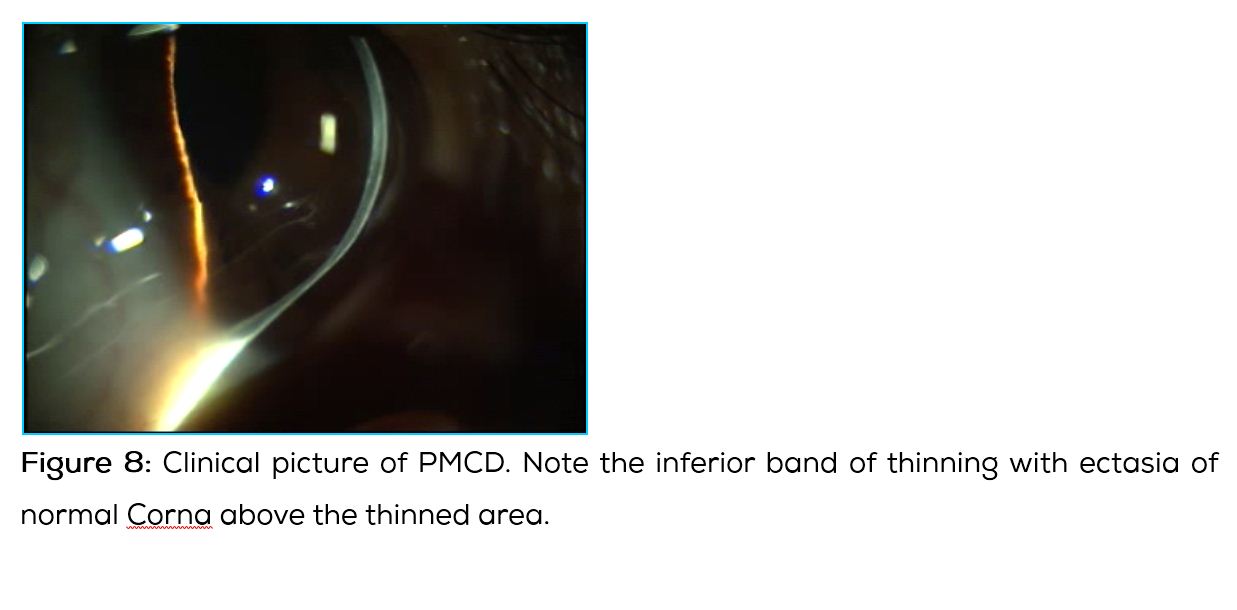
Conclusions
In the last decade or so considerable advances have happened in understanding and managing keratoconus. Eye rubbing as an important factor in causation and progression of keratoconus need to be addressed during management. Collagen cross linking has become the standard procedure to prevent progression of keratoconus. Intracorneal rings, implantable contact lens and deep anterior lamellar keratoplasty are common surgical options offered to patients with keratoconus. Penetrating keratoplasty has been reserved to dense scars with severe ectasia.
Conflict of interest
The authors declare no conflict of interest.
References
1. Rabinowitz YS. The genetics of keratoconus. Ophthalmol. Ophthalmol Clin North Am. 2003; 16(4):607–620.
2. Rabinowitz. Keratoconus. Surv Ophthalmol. 1998; 42(4):297–319.
3. Sharma N, Rao K, Maharana PK, Vajpayee RB. Ocular allergy and keratoconus. Indian J Ophthalmol. 2013; 61(8):407–409.
4. Cingu AK, Cinar Y, Turkcu FM, Sahin A, Ari S, et al . Effects of vernal and allergic conjunctivitis on severity of keratoconus. Int J Ophthalmol. 2013; 6(3):370–374.
5. Fong AH, Shum J, Ng AL, Li KK, McGhee S, et al. Prevalence of ocular abnormalities in adults with Down syndrome in Hong Kong. Br J Ophthalmol. 2013; 97:423–428.
6. Ortiz-Toquero S, Rodriguez G, de Juan V, Martin R. Repeatability of Placido-Based Corneal Topography in Keratoconus. Optom Vis Sci. 2014; 91(12):1467–1473.
7. McMonnies CW. Mechanisms for acute corneal hydrops and perforation. Eye Contact Lens. 2014; 40(4):257–264.
8. Rathi VM, Mandathara PS, Dumpati S. Contact lens in keratoconus.Indian J Ophthalmol. 2013; 61(8):410–415.
9. Rabinowitz YS. Intacs for keratoconus. Curr Opin Ophthalmol. 2007; 18(4):279–283.
10. Rabinowitz YS. INTACS for Keratoconus. Int Ophthalmol Clin. 2010; 50(3):63–76.
11. Romano V, Iovieno A, Parente G, Soldani AM, Fontana L. Long-term clinical outcomes of deep anterior lamellar keratoplasty in patients with keratoconus. Am J Ophthalmol. 2015; 159(3):505–511.
12. Maharana PK, Agarwal K, Jhanji V, Vajpayee RB. Deep anterior lamellar keratoplasty for keratoconus: a review. Eye Contact Lens. 2014; 40(6):382–389.
13. Choi JA, Lee MA, Kim MS. Long-term outcomes of penetrating keratoplasty in keratoconus: analysis of the factors associated with final visual acuities. Int J Ophthalmol. 2014; 7(3):517–521.
14. Kummelil MK, Hemamalini MS, Bhagali R, Sargod K, Nagappa S, et al. Toric implantable collamer lens for keratoconus. Indian J Ophthalmol. 2013; 61(8):456–460.
15. Shafik Shaheen M, El-Kateb M, El-Samadouny MA, Zaghloul H. Evaluation of a toric implantable collamer lens after corneal collagen crosslinking in treatment of early-stage keratoconus: 3-year follow-up. Cornea. 2014; 33(5):475–480.
16. Dirani A, Fadlallah A, Khoueir Z, Antoun J, Cherfan G, et al. Visian toric ICL implanta-tion after intracorneal ring segments implantation and corneal collagen crosslinking in keratoconus. Eur J Ophthalmol. 2014; 24(3):338–344.
17. Raiskup F, Theuring A, Pillunat LE, Spoerl E. Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressivekeratoconus: ten-year results. J Cataract Refract Surg. 2015; 41(1):41–46.
18. Brittingham S, Tappeiner C, Frueh BE. Corneal cross-linking in keratoconus using the standard and rapid treatment protocol: differences in demarcation line and 12-month outcomes. Invest Ophthalmol Vis Sci. 2014; 55(12):8371–8376.
19. Konstantopoulos A, Mehta JS. Conventional versus accelerated collagen cross-linking for keratoconus. Eye Contact Lens. 2015; 41(2):65–71.
20. Shah SG, Sridhar MS, Sangwan VS. Acute corneal hydrops treated by intracameral injection of perfluoropropane (C3F8) gas. Am J Ophthalmol. 2005; 139(2):368–370.
21. Nanavaty MA, Daya SM. Outcomes of deep anterior lamellar keratoplasty in keratoconic eyes with previous hydrops. Br J Ophthalmol. 2012; 96(10):1304–1309.
22. Narayan N, Sridhar MS. Perfluropropane (C3F8) gas injection followed by deep anterior lamellar keratoplasty (DALK) in severe keratoconus. Eye (Lond). 2014; 28(10):1260–1261.