Full Text
Introduction
Hypertension is a major health issue in India, the prevalence being 13.8% to 30.7% [1]. Recent studies report an increasing prevalence with more persons diagnosed with target organ damage, including hypertensive retinopathy [2].
Precise pathogenesis of hypertensive retinopathy (HR) has not been recognized. Hypertension alone does not lead to hypertensive retinopathy. Other factors like platelet activation have been shown to influence development of hypertensive retinopathy [3].
Several laboratory tests have been designed recently to determine platelet activation; however, these are expensive and their usefulness in resource poor setting is doubtful [4]. Mean platelet volume (MPV) is an indicator of platelet activation. MPV is a simple, easy, cost effective tool and the values are easily available from automated haematology analyser. Large platelets have more granules and aggregate readily. Studies have documented an important relationship between raised MPV and occurrence of vascular complications in diseases like diabetes mellitus, myocardial infarction and renal artery stenosis [5].
Similarly, studies have documented MPV values to be higher in hypertensives as compared to normotensives [6]. However, there are few studies done on determining the relationship of MPV in hypertensive retinopathy.
Bhatti et al observed that MPV was elevated in hypertensive retinopathy and that a between elevated MPV and various grades of hypertensive retinopathy [7]. Similar findings were observed by Hussain et al & Yadav et al [2, 8]. However, there are few studies which demonstrate that not all patients with hypertensive retinopathy show increased platelet activation [9]. Presence of hypertensive retinopathy indicates occurrence of complications like nephropathy along with an increased risk of subsequent stroke independent of the underlying co morbid conditions [10]. Hence early diagnosis of hypertensive retinopathy is important to prevent these incidents as well as to initiate preventive measures.
In view of limited number of studies and conflicting results this study is planned with the aim to determine role of MPV in predicting severity in hypertensive retinopathy in a rural set up.
Materials and methods
Prior to the commencement of study, institutional ethical committee (IEC) clearance was obtained. Informed written consent was obtained from the participants. The study done is a cross sectional observation study for the duration of two months. The main objectives of the study were to determine the MPV levels in cases having Hypertensive retinopathy and also to determine the severity by comparing the grade of HR with levels of MPV. By convenient sampling, the sample size of 100 patients was taken. The patients selected were from the out-patient Department of Ophthalmology, & Department of SAHRC. Patients aged 31 to 80 years of age having HR were selected. Direct and indirect ophthalmoscopy were done to diagnose hypertensive retinopathy.
Patients excluded from the study were patients having anemia, diabetes mellitus, infections, malignancy, patients taking antiplatelet drug and patients with idiopathic thrombocytopenic purpura.
Definition of variables
Hypertension was considered when the systolic blood pressure was >140 mmHg and diastolic blood pressure >90mmHg. HR was recorded after administration of 1% mydriacyl eye drop and was classified as per Keith, Wagener and Barker classification into 4 grades (with grade 1 being mild and grade 4 being severe).
Grade 1 retinopathy when there was mild generalized retinal arteriolar narrowing or sclerosis.
Grade 2 retinopathy was characterized by definite focal narrowing and arteriovenous crossings. There was moderate to marked sclerosis of retinal arterioles and exaggerated arterial light reflex.
Grade 3 retinopathy when retinal haemorrhages, exudates and cotton-wool spots were seen. Presence of sclerosis and spastic lesions of retinal arterioles also classified a lesion in this grade.
Grade 4 was considered when severe grade 3 findings and papillo-oedema was present.
Statistical analysis
The statistical analysis was made by entering the data in excel sheets, which was then expressed as mean values, standard deviations and proportions. Thereafter by using one way analysis of variance (ANOVA) a comparison between levels of MPV and grade of Hypertensive retinopathy was made.
Similarly a correlation between MPV, age, haemoglobin levels and platelet count was made using Pearson’s correlation in all the cases of hypertensive retinopathy. P value <0.05 was considered to be significant.
Results
Data of 100 cases with hypertensive retinopathy was recorded and analysed. The mean age of patients with hypertensive retinopathy was 59.448 (±11.642) years for Grade 1, 56.166 (±10.037) years for Grade 2, 58(±19.37) years for Grade 3 (Table 1).
Table 1: Age wise distribution of all 100 cases across various grades of hypertensive retinopathy.
|
Age group
|
Number of patients in each grade
|
Total
|
|
Grade 1
|
Grade 2
|
Grade 3
|
|
31-40
|
2
|
-
|
2
|
04
|
|
41-50
|
8
|
10
|
-
|
18
|
|
51-60
|
30
|
8
|
-
|
38
|
|
61-70
|
6
|
12
|
-
|
18
|
|
71-80
|
12
|
6
|
4
|
22
|
|
Total
|
58
|
36
|
06
|
100
|
Among these 100 cases, 58 patients had Grade 1 HR, 36 patients had Grade 2 HR, 6 patients had Grade 3 HR (Figure 1). From these 100 patients 56 were female patients and 44 were male patients (Table 2).
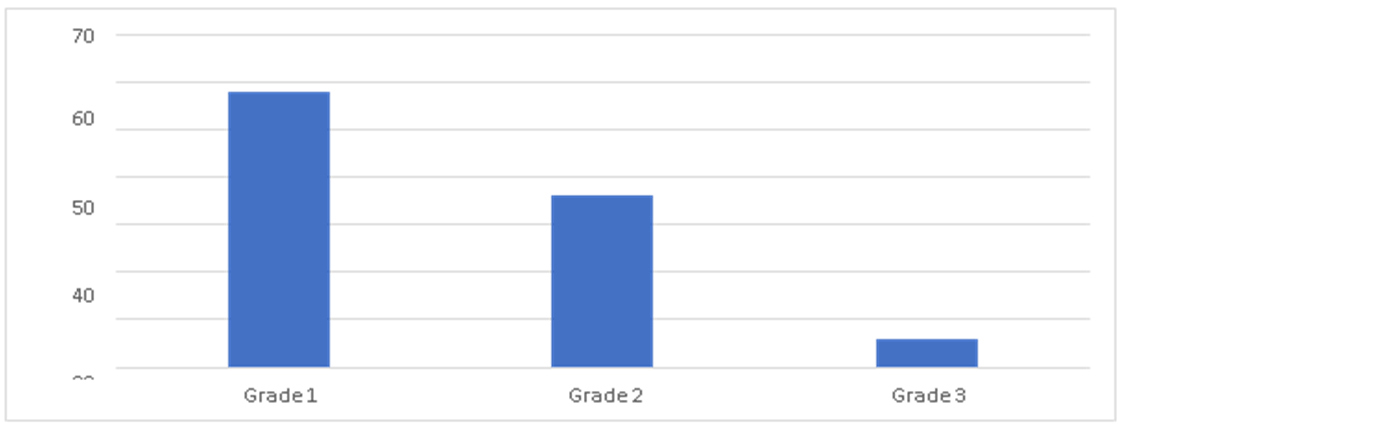
Figure 1: Bar diagram showing distribution of cases in various grades of hypertensive retinopathy.
Table 2: Gender wise distribution.
|
Gender
|
Frequency (N)
|
Percent (%)
|
|
Female
|
56
|
56
|
|
Male
|
44
|
44
|
|
Total
|
100
|
100
|
Gender Frequency (N) Percent (%) Female 56 56 Male 44 44 Total 100 100 For all the 100 cases, mean and standard deviation of age, hemoglobin levels, platelet count and mean platelet volume were calculated (Table 3).
Table 3: Shows mean, standard deviation values of age, hemoglobin, platelet count and mean platelet volume in all 100 cases of hypertensive retinopathy.
|
Parameters
|
N
|
Mean
|
Std. deviation
|
|
Age (Years)
|
100
|
54.123
|
10.031
|
|
Hb (g/dl)
|
100
|
13.245
|
1.761
|
|
Platelet count (*Lakhs/cumm)
|
100
|
2.145
|
0.230
|
|
MPV (fL)
|
100
|
8.676
|
0.8887
|
Hemoglobin levels in various grades of hypertensive retinopathy were noted. Hemoglobin levels were 13.492±1.093 g/dl in grade 1, 13.544±1.461 g/dl in grade 2 and 13.733±0.8115 g/dl in grade 3 hypertensive retinopathy (Table 4).
Table 4: Hemoglobin levels in various grades of hypertensive retinopathy.
|
Grades of HR
|
N
|
Hemoglobin levels (gm/dl) ± Std. deviation
|
|
1
|
58
|
13.492 ± 1.093
|
|
2
|
36
|
13.544 ± 1.461
|
|
3
|
N
|
13.733 ± 0.8115
|
The severity of hypertensive retinopathy and levels of MPV were compared by analysis of variance (ANOVA) and p value < 0.05 is considered to be significant. The MPV was 8.55± 0.576 in Grade 1 HR, 9.17± 0.8224 for Grade 2 HR and 9.6± 1.5594 for Grade 3 HR (Table 5). This shows that there is a significant increase in levels of MPV in increasing severity of hypertensive retinopathy (P value< 0.0001).
Table 5: Shows the mean MPV values and platelet count in various grades of hypertensive retinopathy.
|
Parameters
|
Grade 1 HR (N-58)
|
Grade 2 HR (N-36)
|
Grade 3 HR (N-06)
|
p value
|
|
Mean platelet volume (fl)
(Std. Deviation)
|
8.55 ± 0.576
|
9.17 ± 0.8224
|
9.6 ± 1.5594
|
0.0001*
|
|
Platelet count
(Lakh/cumm)
(Std. Deviation)
|
3.21 ± 0.321
|
2.52 ± 0.375
|
2.1 ± 0.912
|
0.412
|
Pearson’s correlation was applied to determine the relationship between mean platelet volume and other continuous variables like age, hemoglobin and platelet count. Statistical significance was set at p<0.05. There was no significant correlation between MPV and platelet count (r=0.45, p<0.657). There was no significant correlation between MPV and hemoglobin levels (r=-0.167, p<0.096). However, a significant positive correlation was observed between MPV and age of the cases with HR (r=0.357, p<0.0001) (Table 6).
Table 6: Shows correlation between age, hemoglobin, platelet count and MPV in all 100 cases of hypertensive retinopathy.
|
Parameters
|
Age
|
HB (g/dl)
|
Platelet count
|
MPV (fl)
|
|
Age
|
Pearson correlation
|
1
|
-0.044
|
0.110
|
0.357**
|
|
Sig. (2-tailed)
|
|
0.660
|
0.277
|
0.000
|
|
N
|
100
|
100
|
100
|
100
|
|
HB (g/dl)
|
Pearson correlation
|
-0.044
|
1
|
0.017
|
-0.167
|
|
Sig. (2-tailed)
|
0.660
|
--
|
0.868
|
0.096
|
|
N
|
100
|
100
|
100
|
100
|
|
Platelet count
|
Pearson correlation
|
0.110
|
0.017
|
1
|
0.045
|
|
Sig. (2-tailed)
|
0.277
|
0.868
|
--
|
0.657
|
|
N
|
100
|
100
|
100
|
100
|
|
MPV (fl)
|
Pearson correlation
|
0.357**
|
-0.167
|
0.045
|
1
|
|
Sig. (2-tailed)
|
0.000
|
0.096
|
0.657
|
--
|
|
N
|
100
|
100
|
100
|
100
|
**Correlation is significant at the 0.05 level (2-tailed).
Discussion
Hypertension is one of the most important causes of premature death worldwide. In India, it is responsible for 57% of all stroke deaths and 24% of all coronary artery diseases. The prevalence of hypertension in India is around 13.8% to 30.7% [1].
It is seen that there is a high prevalence of HR among all age groups hypertensive patients [2]. Hypertensive retinopathy is mainly characterized by presence of various retinal vascular changes [7]. If left untreated, hypertensive retinopathy can cause significant damage to the vision but if treated early the vascular changes are stopped [1, 2].
Additionally, presence of retinal microvascular changes lead to 2 to 3 times increased risk of stroke within three years, independent of the presence of hypertension, diabetes mellitus or other risk factors [10]. Early detection of hypertensive retinopathy and its severity is essential for accurate management. The precise pathogenesis of hypertensive retinopathy is not known. Nevertheless, current evidence favour platelet activation, an important contributor to hypertension, to be responsible for complications, including hypertensive retinopathy.
Mean platelet volume is the measure of the average platelet size and platelet activity. So, an increase in mean platelet volume is seen with formation of larger platelets when they become active. Larger platelets have more tendency to aggregate and are more suggestive of thrombus formation [4]. Thus, mean platelet volume can be considered as an indicator of platelet activation. Also mean platelet volume is a simple, easy and cost-effective tool whose values are easily available from automated hematology analyser. Hence the present study was conducted with the aim to assess relationship of MPV with various grades of hypertensive retinopathy.
In the present study, we see that the mean age of patients with hypertensive retinopathy was 59.448 (±11.642) years for Grade 1, 56.166 (±10.037) years for Grade 2, 58 (±19.37) years for Grade 3 (Table 1). This is in accordance with the findings reported by Coban et al., who found the mean age in years to be 56.8 (±9.74) for Grade 1 and 58.1 (±10.3) for Grade 2 [3]. Similar findings were also observed in other studies in the literature [17]. Significant correlation was noted between age of the patient and MPV values, implying increase in MPV values with the age of the study population. Similar findings were reported by Bhatti et al [7].
Maximum number of cases in the present study was diagnosed with Grade 1 HR which was in accordance with the findings reported by Hussain et al, wherein most cases (86.9%) belonged to Grade 1 or Grade 2 HR [2]. In our study, none of the cases had Grade 4 HR (Figure 1). In the study by Hussain et al, Grade 4 HR construed less than 3% of the cases [2].
In the present study, female patients were more commonly affected than males (ratio being, male: female= 1:1.272). This is similar to the findings reported by Hussian et al, who had more female cases with HR (22 out of 41) than male cases [2]. Growing evidence has suggested the role of MPV in predicting severity and complications in many diseases including diabetes, cardiovascular diseases, stroke etc [18]. Similar data is available for hypertension as well. Coban et al reported significantly higher MPV values in essential and white coat hypertension as compared to normotensives [19].
Likewise, other studies have documented strong relationship between various other platelet parameters like platelet distribution width (PDW), platelet count, platelet large cell ratio (PLCR) and occurrence of target organ damage amongst hypertensive patients [6-8]. These findings depict the important role of MPV in predicting complications in hypertensive cases. Another interesting finding was reported by Varol et al and Yazici et al who observed that MPV was increased in prehypertensives as compared to normotensives, suggesting the utility of MPV in early identification of at risk cases [12, 13]. Similarly, Inanc et al mentioned a significant finding of elevated MPV in non-dippers as compared to dippers and controls, implicating its role in predicting risk of atherosclerosis in non-dippers as compared to dippers [20].
In a recent meta-analysis by Shabrina et al MPV was found to be significantly associated with retinal vein occlusion in hypertensive cases [21]. In the present study, MPV values increased with the increasing severity of HR (Table 5). Our findings were comparable with that reported in the literature [2, 3, 7]. Similarly, findings of Yadav et al involving 250 cases of HR in Indian population attested the role of MPV in predicting worse outcome in microvascular complications [8].
Platelet indices like MPV, PDW, PLCR have been shown to be useful prognostic markers in diabetic retinopathy [22]. In a large population based longitudinal study conducted by Yang et al., involving 6515 cases, authors did not find any association between platelet count and hypertension [23]. Similarly, amongst 2881 cases of hypertension, studied by Gang et al in their study, no association was found between platelet count and hypertension [24]. There are very few reports on association of hypertensive retinopathy and platelet count [3-4].
In the current study, along with MPV, the relationship between platelet count and various grades of HR was also analyzed. A decrease in platelet count with increasing severity of HR was noted though this relationship was not statistically significant. Decrease in platelet count in patients with branch retinal vein occlusion has been reported earlier [25].
The limitation of the present study is the small sample size, which limits generalization of the findings to the population. However, further studies with large sample size and inclusion of a control group are needed to ascertain the utility of this cost effective and easy tool as significant biomarker in predicting severity in hypertensive retinopathy.
Conclusion
We established a significant relationship between mean platelet volume and severity grades of hypertensive retinopathy. MPV, a cheap and easily available biomarker can be used for predicting severity in hypertensive retinopathy. Acknowledgement Short Term Studentship-Indian Council of Medical Research (STS-ICMR) for the financial support and encouragement provided to complete the project. Funding source Short Term Studentship from Indian Council of Medical Research (STS-ICMR).
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Ramakrishnan S, Zachariah G, Gupta K, Rao JS, Mohanan PP, et al. Prevalence of hypertension among Indian adults: Results from the great India blood pressure survey. Indian Heart J. 2019; 71(4):309–313.
[2] Husain A, Nagra MH, Farooq A. Frequency of increased mean platelet volume in patients suffering from hypertensive retinopathy. APMC. 2010; 4:57–61.
[3] Coban E, Adanir H, Bilgin D. The association of mean platelet volume levels with hypertensive retinopathy. Platelets. 2008; 19(2):115–118.
[4] Kannana M, Ahmad F, Saxena R. Platelet activation markers in evaluation of thrombotic risk factors in various clinical settings. Blood Rev. 2019; 37:100583.
[5] Bath PM, Missouris CG, Buckenham T, MacGregor GA. Increased platelet volume and platelet mass in patients with atherosclerotic renal artery stenosis. Clin Sci. 1994; 87(2):253–257.
[6] Surgit O, Pusuroglu H, Erturk M, Akgul O, Buturak A, et al. Assessment of mean platelet volume in patients with resistant hypertension, controlled hypertension and normotensives. Eurasian J Med. 2015; 47(2):79–84.
[7] Bhatti A, Ali F, Satti S. Relationship of hypertensive retinopathy with mean platelet volume among hypertensive patients. Cureus. 2015; 7(12):e422.
[8] Yadav V, Jain P, Singhai A, Jha RK. Mean platelet volume as an indicator of severity of hypertensive retinopathy in hypertensive subjects. Int J Res Med Sci. 2017; 5(4):1471–1473.
[9] Minuz P, Patrignani P, Gaino S, Seta F, Capone ML, et al. Determinants of platelet activation in human essential hypertension. Hypertens. 2004; 43(1):64–70.
[10] Wong TY, McIntosh R. Hypertensive retinopathy signs as risk indicators of cardiovascular morbidity and mortality. Br Med Bull. 2005; 73–74:57–70.
[11] Sansanayudh N, Anothaisintawee T, Muntham D, McEvoy M, Attia J, et al. Mean platelet volume and coronary artery disease: a systematic review and meta-analysis. Int J Cardiol. 2014; 175(3):433–440.
[12] Varol E, Akcay S, Icli A, Yucel H, Ozkan E, et al. Mean platelet volume in patients with prehypertension and hypertension. Clin Hemorheol Microcirc. 2010; 45(1):67–72.
[13] Yazici M, Kaya A, Kaya Y, Albayrak S, Cinemre H, et al. Lifestyle modification decreases the mean platelet volume in prehypertensive patients. Platelets. 2009; 20(1):58–63.
[14] Nadar SK, Blann AD, Kamath S, Beevers DG, Lip GY. Platelet indexes in relation to target organ damage in high-risk hypertensive patients: a substudy of the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT). J Am Coll Cardiol. 2004; 44(2):415–422.
[15] Radha RKN, Selvam D. MPV in uncontrolled & controlled diabetics- Its role as an indicator of vascular complication. J Clin Diag Res. 2016; 10(8):EC22–EC26.
[16] Ji S, Zhang J, Fan X, Wang X, Ning X, et al. The relationship between mean platelet volume and diabetic retinopathy: a systematic review and meta-analysis. Diabetol Metab Syndr. 2019; 11:1–8.
[17] Yu T, Mitchell P, Berry G, Li W, Wang JJ. Retinopathy in older persons without diabetes and its relationship to hypertension. Arch Ophthalmol. 1998; 116(1):83–89.
[18] Chu SG, Becker RC, Berger PB, Bhatt DL, Eikelboom JW, et al. Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta-analysis. J Thromb Haemost. 2010; 8(1):148–156.
[19] Coban E, Yazicioglu G, Berkant Avci A, Akcit F. The mean platelet volume in patients with essential and white coat hypertension. Platelets. 2005; 16(7):435–438.
[20] Inanc T, Kaya MG, Yarlioglues M, Ardic I, Ozdogru I, et al. The mean platelet volume in patients with non-dipper hypertension compared to dippers and normotensives. Blood Press. 2010; 19(2):81–85.
[21] Shabrina NN, Sawitri RD, Shabrina TN, Ningrum NR. Elevated mean platelet volume and retinal vein occlusion in hypertensive patients: a meta-analysis. J Hypertens. 2020; 38:e5–e6.
[22] Yilmaz T, Yilmaz A. Relationship between altered platelet morphological parameters and retinopathy in patients with type 2 diabetes mellitus. J Ophthalmol. 2016; 2016:9213623.
[23] Yang K, Tao L, Mahara G, Yan Y, Cao K, et al. An association of platelet indices with blood pressure in Beijing adults applying quadratic inference function for a longitudinal study. Medicine. 2016; 95(39):e4964.
[24] Gang L, Yanyan Z, Zhongwei Z, Juan D. Association between mean platelet volume and hypertension incidence. Hypertens Res. 2017; 40(8):779–784.
[25] Onder HI, Kilic AC, Kaya M, Bulur S, Onder E, et al. Relation between platelet indices and branch retinal vein occlusion in hypertensive patients. Indian J Ophthalmol. 2013; 61(4):160–162.