Full Text
Introduction
The clavicle is roughly "S-shaped" with a flattened, concave, lateral one-third and a thickened, convex, medial two-thirds. On the inferior surface of lateral third is the conoid tubercle for the attachment of the conoid ligament and lateral to this is the trapezoid line for attachment of the trapezoid ligament. The apophysis is on the medial side towards the sternum [1].
The clavicle is an unusual bone in more than one way. It lacks a definite medullary cavity and ossifies by membranous ossification. It has two primary centres of ossification and only one secondary centre of ossification, the sternal end. It is the first bone to ossify in the embryo (fifth month). This bone is subcutaneous throughout its length, and it is occasionally pierced by the middle supraclavicular nerve. Fortunately, the clavicle is a bone that can be resected without causing significant disability [2]. The clavicle has several characteristics that distinguish it from other long bones and from flat bones. The ossification centre at the sternal end fuses around the age of 25 years. It contains minimal amounts of red marrow; and it has a poor vascular supply. These are the two factors responsible for the low incidence of bone tumors [3]. The non-traumatic lesions include congenital/ developmental, infective, inflammatory, neoplastic, and other miscellaneous causes. The aim of this paper is to illustrate the radiological features of each entity with a differential diagnosis whenever possible. The imaging methods are listed in Table 1.
Imaging features and discussion
Table 1: Imaging methods.
- Conventional
- CT
- MRI
- PET CT
|
Etiological analysis of clavicular lesions are mentioned in Table 2.
Table 2: Etiology of clavicular lesions other than trauma.
- Congenital/ Developmental
- Infective
- Inflammatory
- Metabolic and endocrinal
- Neoplastic – Benign
- Malignant – Primary, secondary
- Miscellaneous
|
A normal variant is the Rhomboid Fossa on the inferomedial aspect of the medial end of the clavicle simulating a lytic pathological lesion (Figure 1a). This is the site of attachment of the costoclavicular ligament. It may be unilateral or bilateral when present.
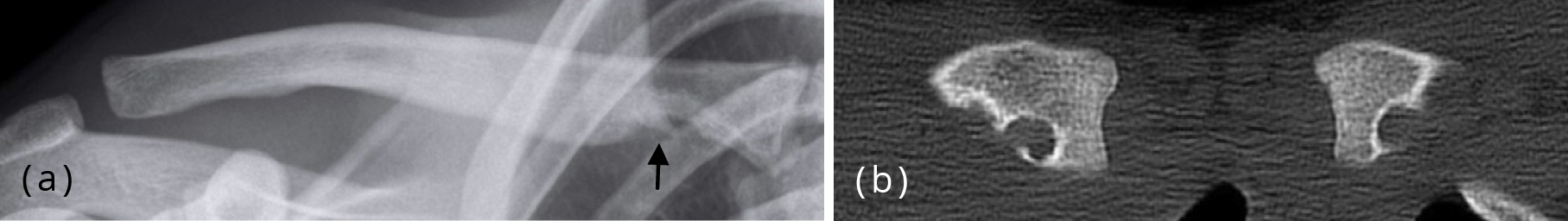
Figure 1a,b: (a) Rhomboid Notch at the attachment of costoclavicular ligament. (b) Rhomboid fossa clavicle bilateral, CT.
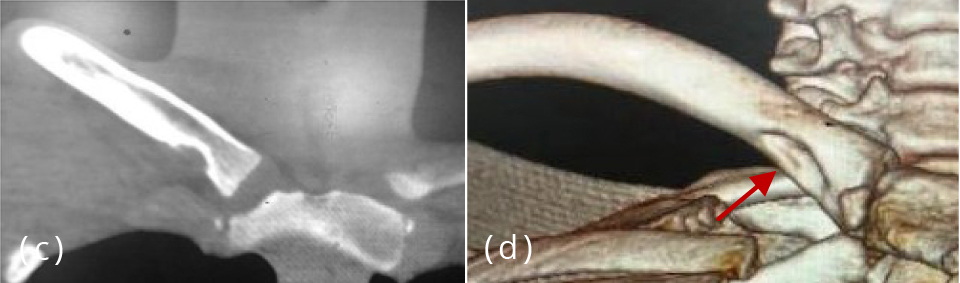
Figure 1c, d: Rhomboid notch - A prominent rhomboid notch is seen along the inferior aspect of the medial portion of the right clavicle.
Congenital / Developmental
Duplication of the clavicle is very rare. It may be partial or complete, bilateral or unilateral [4].
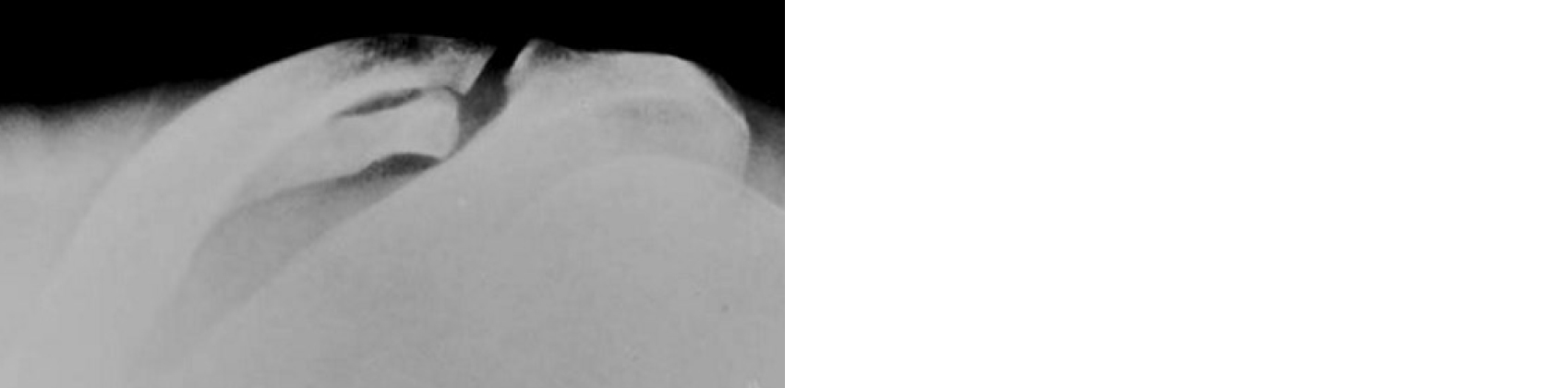
Figure 2: Duplication of the lateral end of the clavicle.
Partial or complete absence of clavicles is noted in skeletal dysplasias and congenital syndromes. It can be isolated also (Figure 3a,b). The other entities include crainocleidodysostosis (Figure 3c,d) and pycnodysostosis (Figure 3e) [5]. Handlebar shaped clavicles are encountered in many disorders including asphyxiating thoracic dysplasia, campomelic dysplasia (Figure 3f), diastrophic dysplasia, Holt-Oram syndrome, mucolipidosis, mucopolysaccharidosis, TAR syndrome and trisomy 18 [6, 7]. In many neoplastic conditions, the clavicle may have to be completely removed (Figure 3g).
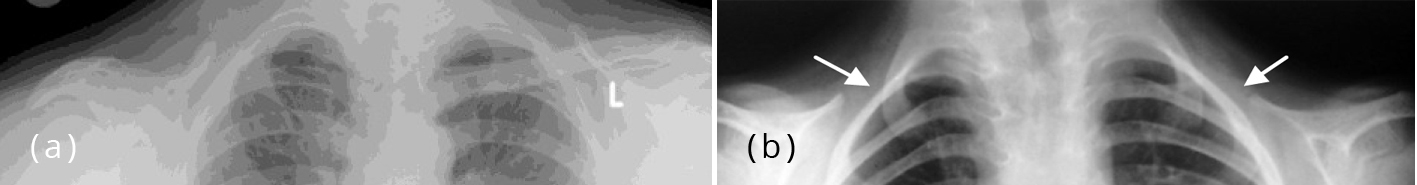
Figure 3a, b: (a) Complete absence of right clavicle. (b) Absence of both clavicles.
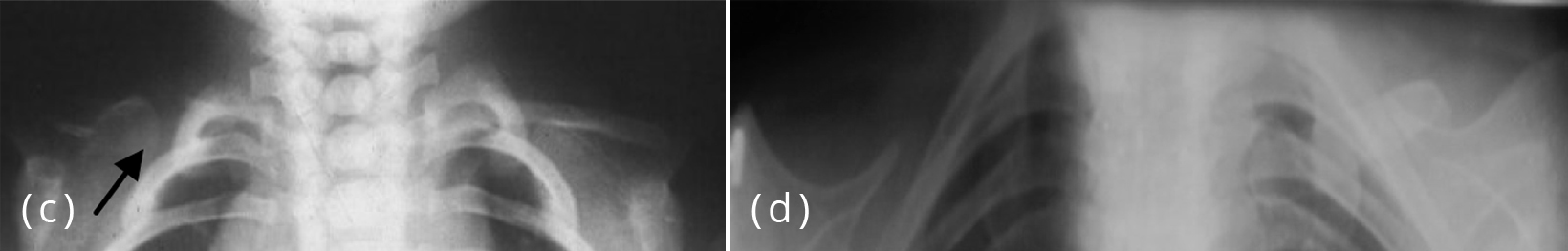
Figure 3c,d: Cleidocranial dysostosis with total absence of the right clavicle and rudimentary left clavicle (arrow).

Figure 3e, f, g: (e) Pycnodysostosis with dysplastic clavicles. (f) Handlebar shaped clavicles. (g) Post surgical resection of clavicle.
In osteopetrosis, the clavicle is dense and may show bone in a bone appearance (Figure 4a). In osteopoikilosis, dense spotty lesions are noted at the lateral end of the clavicle (Figure 4b). In metaphyseal dysplasia (Pyle’s disease), the medial ends of the clavicles are involved with widening of the metaphyses (Figure 4c). While polyostotic fibrous dysplasia is relatively common, isolated focal lesion of this is rarely encountered. It may be expansile, lytic, sclerotic or mixed (Figure 4de) [8]. Melorheostosis is another sclerosing skeletal dysplasia which may involve the clavicle. Dense flowing hyperostosis is noted (Figure 4f). In systemic and enzymatic disorders, the clavicles may be involved. For example, in Hurler’s syndrome, the lateral end of the clavicle is shortened and distorted (Figure 4g) whereas in oxalosis, the ends of the clavicle are widened, dense and bulbous (Figure 4h). In osteogenesis Imperfecta (OI), the bones are thinned out with fractures and presence of abundant callus (Figure 4i) [9].
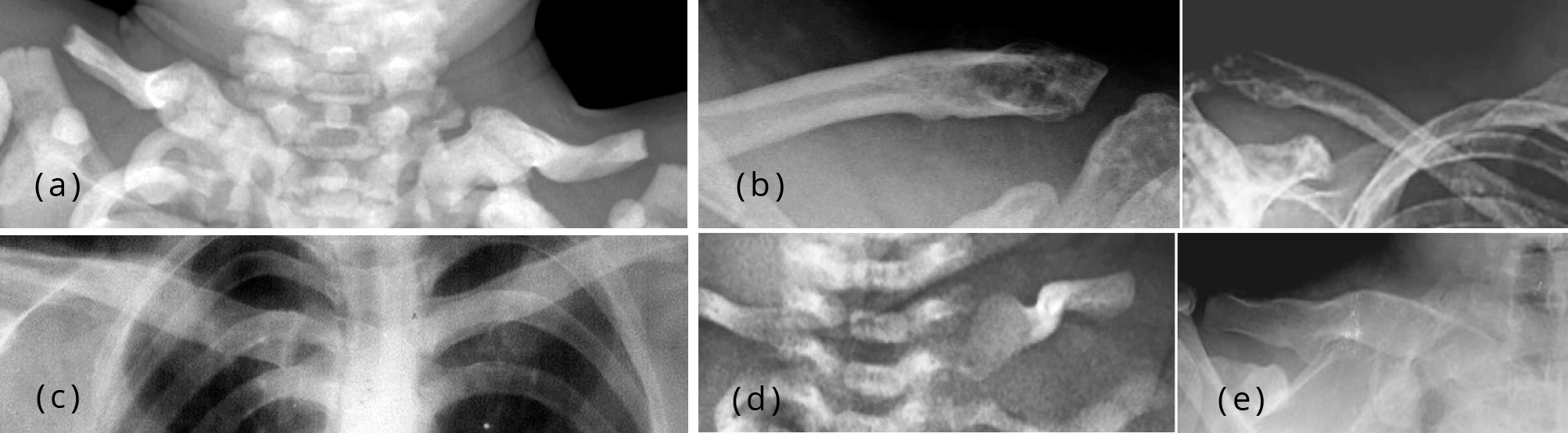
Figure 4a-e: (a) Osteopetrosis, bone in a bone with dense bones. (b) Osteopoikilosis lateral ends of clavicles. (c) Metaphyseal dysplasia (Pyle’s disease). (d,e) Bulbous expansion medial end of clavicles in fibrous dysplasia.
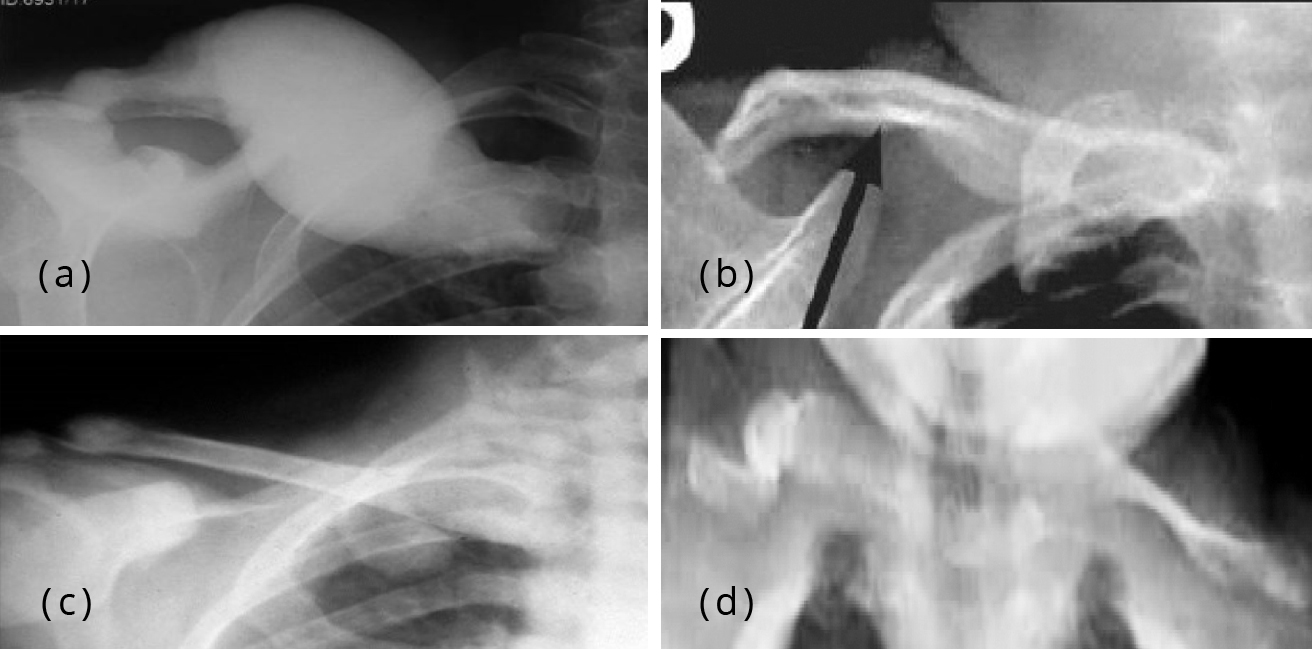
Figure 4f-i: (f) Melorheostosis of the right clavicle, note the extensive bone proliferation along the midshaft. (g): Hurler’s syndrome, short and thickened clavicle. (h) Oxalosis showing “drum-stick” clavicles with sclerosis and bulbous deformity of the medial and lateral end of the clavicle. (i) Osteogenesis imperfecta, thinned out and distorted fractured clavicles, bulbous ends are also noted.
Infections
Osteomyelitis of the clavicle is rare. It may be found in acute, subacute and chronic stages and the imaging findings are the same as seen in the long bones. Often the infection from the sternoclavicular joints spreads to the clavicle [10]. Pyogenic infections may produce reactive bone. There is a type of chronic osteomyelitis which is called sclerosing osteomyelitis where there is diffuse sclerosis and periostitis is present (Figure 5a). In Tuberculosis the sternoclavicular (SC) joint may be involved with an abscess formation [11]. Here the new bone is scanty but there may be association of lymphadenopathy (Figure 5b,c).
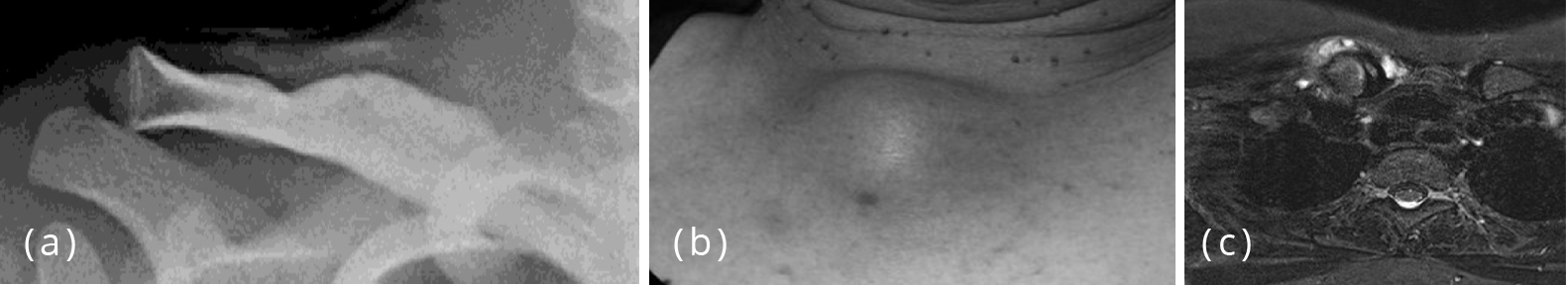
Figure 5: (a) Sclerosing osteomyelitis of the right clavicle. (b,c) TB Abscess medial end of the clavicle, involvement of the SC joint, (b) Clinical, (c) MRI.
Inflammatory
Condensing osteitis of the clavicle is a rare entity. It is radiologically characterized by focal sclerosis of the medial end of the clavicle. No periosteal reaction is noted. The sternoclavicular joint is not involved (Figure 6) [12, 13].
Figure 6: Condensing osteitis of the right clavicle with sclerosis of its medial end.
SAPHO syndrome
SAPHO (synovitis, acne, pustulosis, hyperostosis and osteitis) syndrome is a distinct clinical entity representing involvement of the musculoskeletal and dermatologic systems. SAPHO and related conditions have three components of progression, which are include: costoclavicular ligament ossification, arthropathy of the sternoclavicular joint, osteitis of the medial end of the clavicle, first rib and sternum as well as hypertrophy of the costal cartilages [14]. Radiologically, there is sclerosis of the medial half of the clavicle with periosteal reaction and soft tissue swelling (Figure 7a-c).
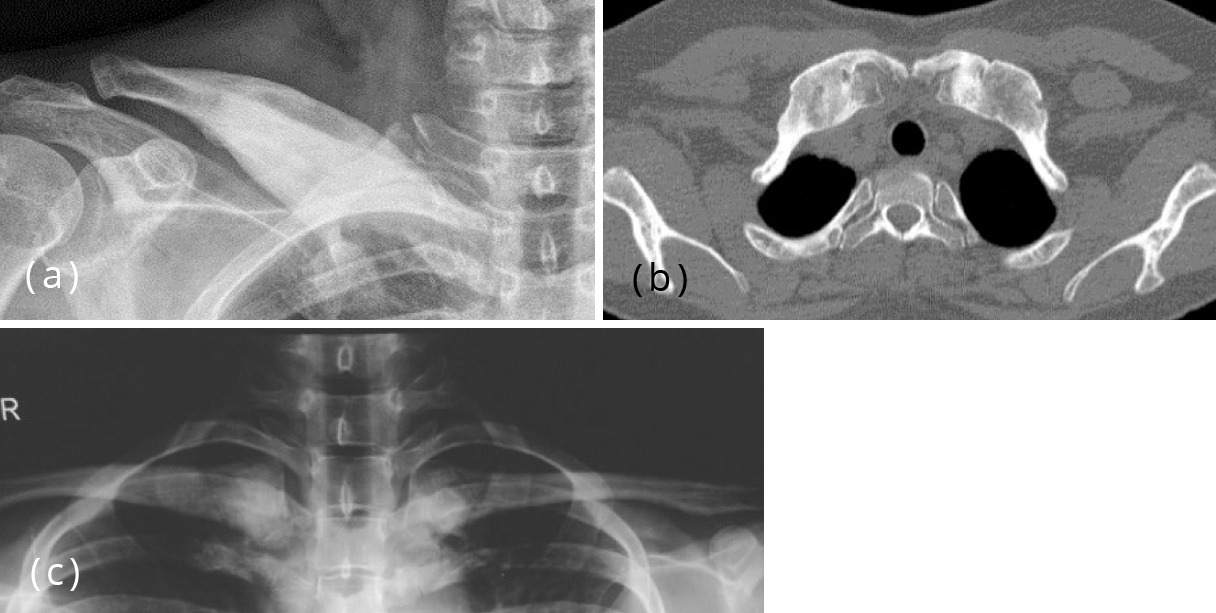
Figure 7: (a) SAPHO Syndrome, sclerosis and periosteal reaction of the clavicle, involvement of the SC joint, (b) CT Sternoclavicular joints. (c) SAPHO syndrome, sclerosis of the medial ends of the clavicles.
Metabolic and enzymatic disorders
Primary and secondary hyperparathyroidism, oxalosis, gout and hypophosphatasia may have changes in the clavicle.
Hyperparathyroidism, primary or secondary, shows subperiosteal resorption of bone as a classical hallmark [15]. Brown tumors may also be noted in the clavicle (Figure 8a). Loozer zones and pathological fractures may be seen (Figure 8b).

Figure 8a: Hyperparathyroidism with brown tumor, note the resorption of the lateral end of the clavicle.

Figure 8b: Hyperparathyroidism, resorption of medial and lateral ends of clavicles, loozer zone of the left clavicle.
Gout is a crystal arthropathy due to deposition of monosodium urate crystals in and around the joints. It is a polyarticular disease and joints of the feet are the common sites for involvement. Shoulder joint and clavicle also may be involved [16]. The lateral end of the clavicle is resorbed with minute calcific densities representing tophi (Figure 9).

Figure 9: Gouty deposit, note the osteolysis of the clavicle.
Neoplastic: Benign tumors
These tumors may be osseous, cartilaginous, or vascular origin. Tumors of osseous origin are noted in Table 3.
Table 3: Osseous origin.
- Osteoma
- Osteoid osteoma
- Osteoblastoma
|
Bone islands and osteomas are rarely present in clavicle. Osteoid osteoma presents the same imageological picture as is encountered in any long bone. There is a central nidus of about 1.5 cm diameter with reactive sclerosis surrounding it (Figure 10a) [17]. Osteoblastoma is similar in appearance as Osteoid osteoma except the nidus is more than 1.5 cm in diameter. Occasionally an aneurismal bone cyst may be associated with osteoblastoma.
Cartilaginous origin [18]
• Enchondroma
• Exostosis
• Chondroblastoma
Enchondroma is not as common as is seen in other bones; however the radiological appearance is the same as is encountered in other areas. A large lucency with central mineralisation in the form of dense rings, arcs and nuggets is noted. It is well circumscribed indicating the benign nature (Figure 10b,c).
The clavicle may also be involved in multiple hereditary osteochondromata which is generalized (Figure 10d,e). It may be pedunculated or sessile. When it is large malignant transformation is considered. Chondroblastoma is rare in the clavicle.
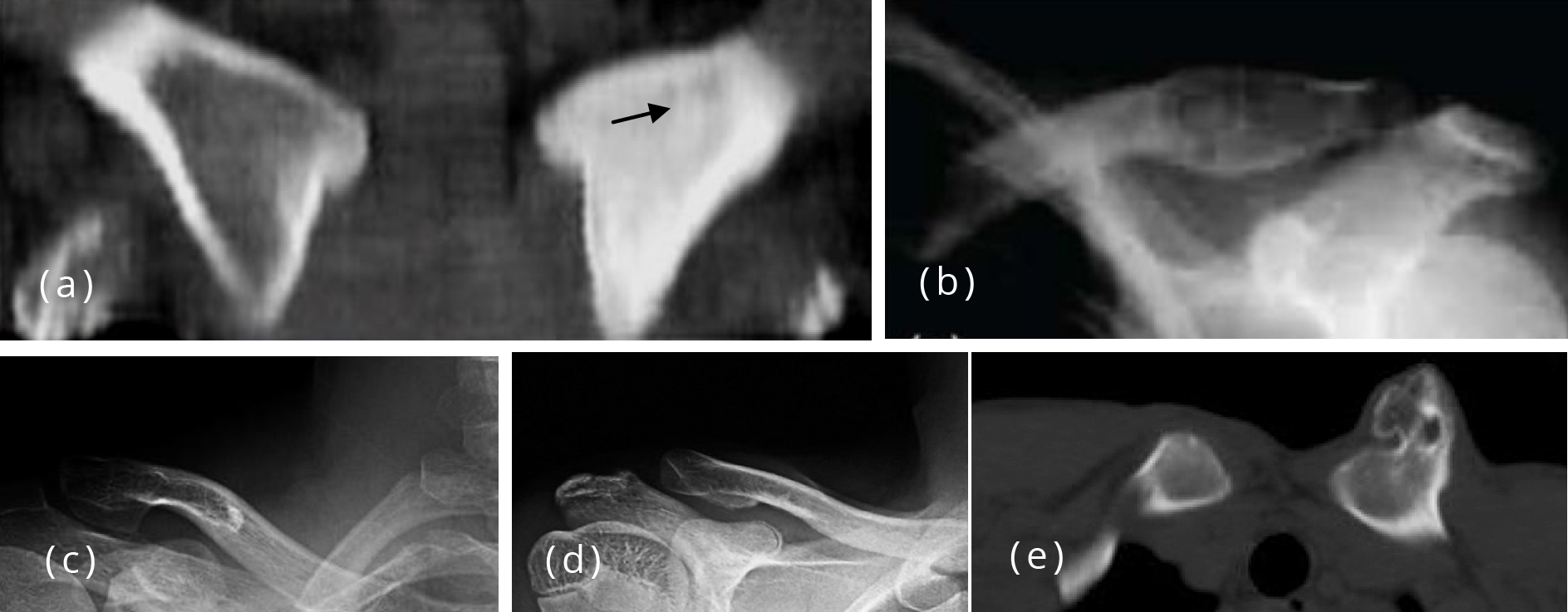
Figure 10: (a) Osteoid osteoma left clavicle with a nidus in CT. (b) Enchondroma clavicle. (c) Enchondroma lateral end of clavicle. (d,e) Osteochondroma lateral end of the clavicle.
Langerhans cell histiocytosis
There are 3 major forms and localised eosinophilic granuloma (EG) is occasionally encountered in clavicle [19]. Generally it is a lytic lesion with bevelled edges with or without periosteal reaction (Figure 11a,b). Occasionally the reactive sclerosis is abundant (Figure 11c).

Figure 11: (a,b) EG medial end of clavicle, (a) Conventional, (b) MRI. (c) Langerhans cell histiocytosis – Unusually sclerotic lesion with reparative new bone.
Malignant tumors of the clavicle The age, transitional zone, mineralisation, periosteal reaction and soft tissue swelling are characteristic and distinguishable from benign tumors [20].
• Osteosarcoma
• Ewing’s sarcoma
• Chondrosarcoma
• Plasmacytoma
• Lymphosarcoma
• Fibrosarcoma / Malignant fibrous histocytoma
Osteosarcoma could be lytic, sclerotic or mixed. Tumoral new bone is noted with a soft tissue swelling (Figure 12a). Periosteal reactions of various types are noted of which sunburst appearance is a prominent feature (Figure 12b).
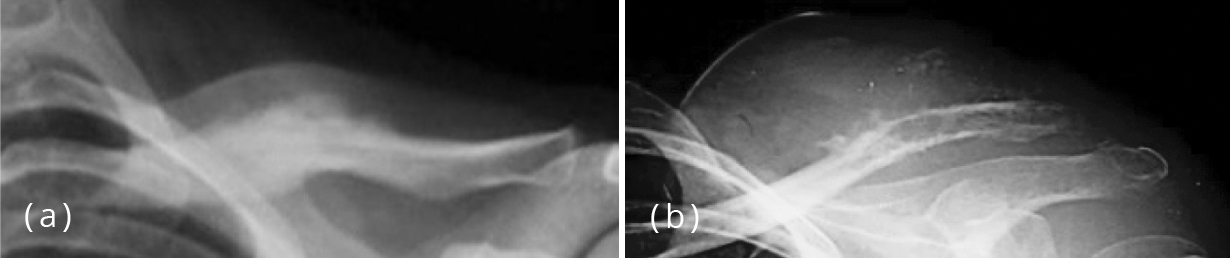
Figure 12: (a) Osteosarcoma medial end of left clavicle with new bone formation. (b) Osteosarcoma lateral end of clavicle with sunray spicules.
Ewing’s sarcoma is one of the round cell tumors mostly encountered in children. The diaphysis of the long bones is one of the common sites (Figure 13a). Several morphological features are noted including lysis varying from moth eaten to balloon type (Figure 13b). Similarly, mineralisation due to reactive bone is noted from minimum to dense ivory type. Soft tissue swelling is a prominent feature in some instances (Figure 13c-e).
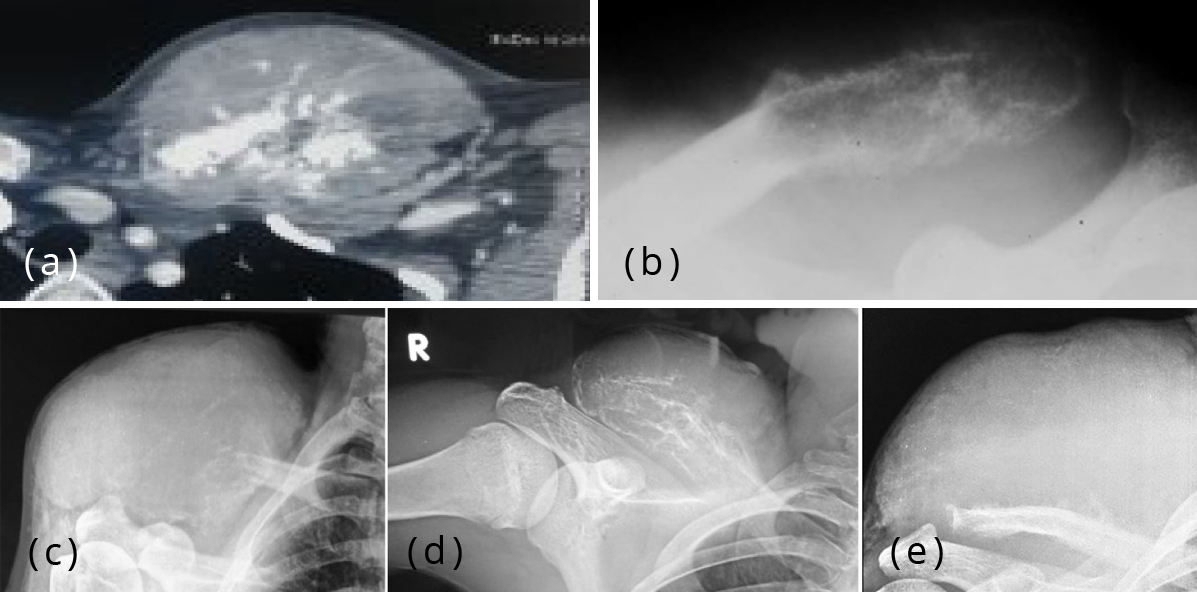
Figure 13: (a) Ewing’s sarcoma medial end of the clavicle, CT showing extensive new bone. (b) Ewing’s sarcoma, Note the bone expansion with “sun-burst” appearance. (c-e) Ewing’s sarcoma lateral end of clavicle.
Chondrosarcoma of the clavicle is quite rare. It is generally a primary malignant lesion. All the features of a malignant bone tumor are present. However, the mineralization is different and is of cartilaginous type namely arcs, rings, circles and nuggets [21]. Osteochondroma may undergo malignant transformation (Figure 14).
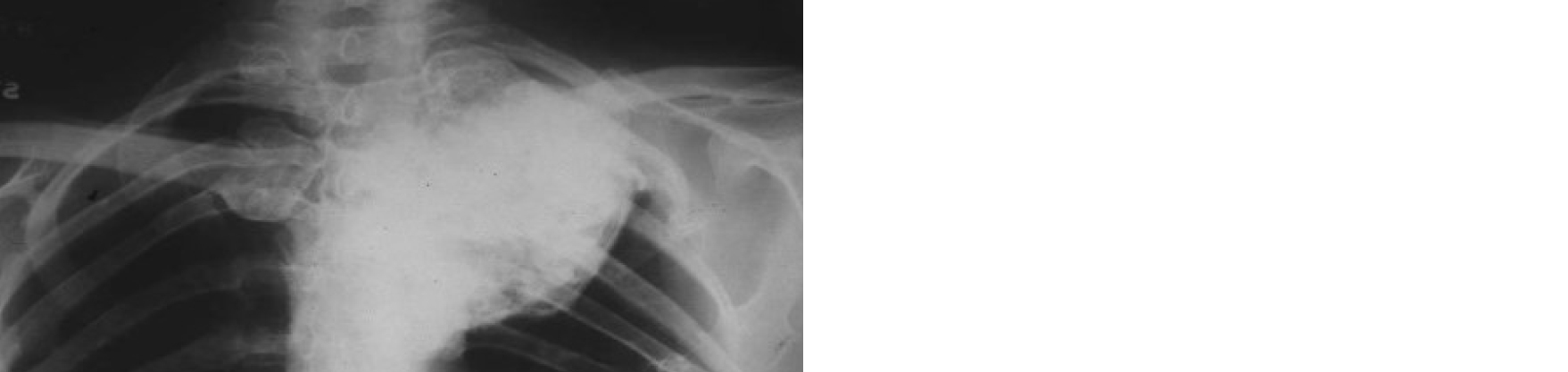
Figure 14: Multiple exostosis. Malignant transformation of the lesion in the medial end of the clavicle.
Plasmacytoma is a focal form of multiple myeloma. Isolated Plasmacytoma of the clavicle is rare. A lytic and expansile lesion with little new bone formation is noted (Figure 15a). Periosteal reaction is rare without a pathological fracture [22]. Soft tissue swelling is occasionally present. Multiple myeloma manifests as multiple punched out areas (Figure 15b) [23].

Figure 15: (a) Plasmacytoma of the right clavicle in a case of multiple myeloma. (b) Multiple myeloma involving the clavicle and scapula.
Primary lymphoma of the clavicle is rare [24]. When encountered a large lytic area that is variable, reactive bone and a soft tissue swelling is noted (Figure 16). There may or may not be any significant periosteal reaction. The bone involved may be completely dense.

Figure 16: 12-year-old boy, lymphoma of the right clavicle presenting as a pathological fracture and a soft tissue swelling.
Fibrosarcoma and malignant fibrous histiocytoma of the clavicle are rare. Metastases to clavicle are not unusual but not as common as encountered in the rest of the bones [25]. They may appear as mixed, lytic or sclerotic lesions. Solitary metastasis to the clavicle is rare and usually the primary malignancy is noted in the lung, breast, kidney and other organs (Figure 17a-c). Pathological fractures may be seen (Figure 17d).
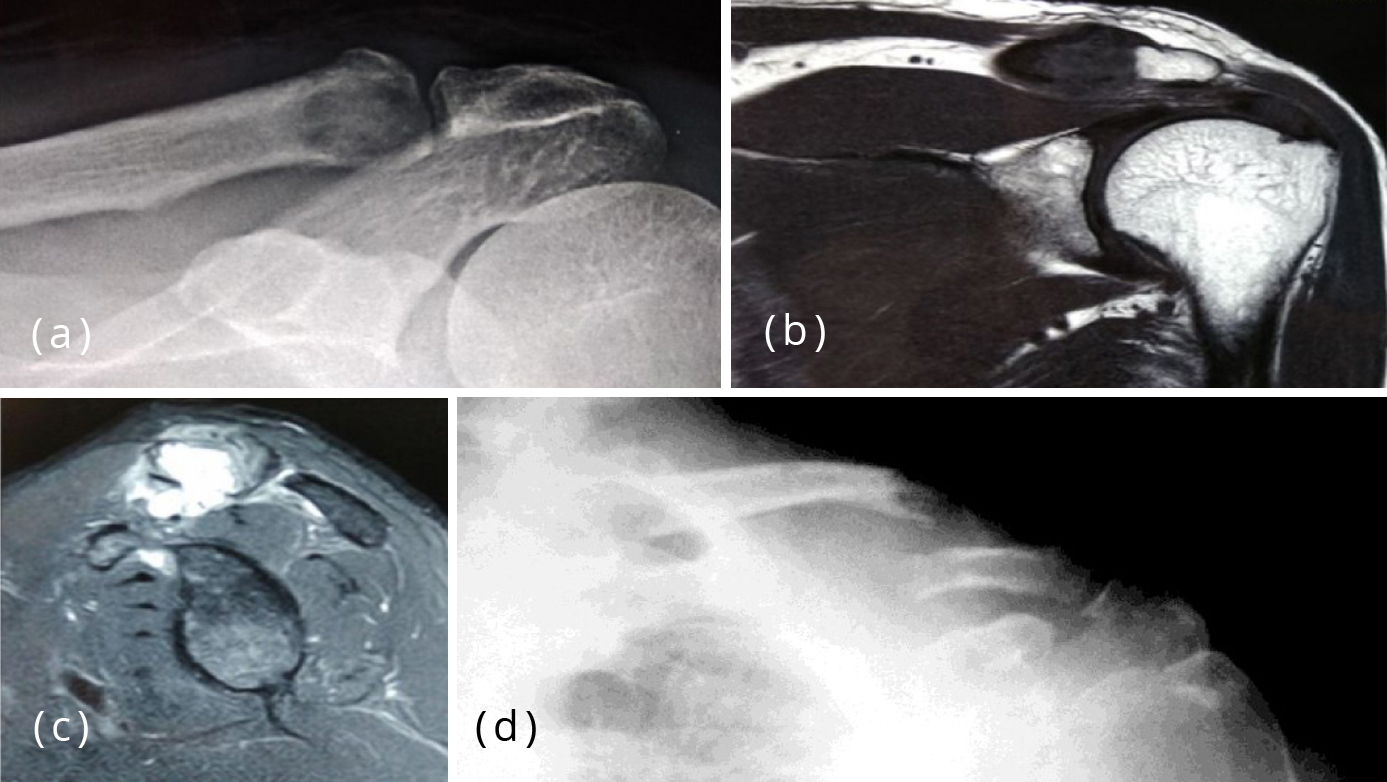
Figure 17: (a-c) 58 M, Mets from lung adeno CA, (a) Conventional, (b,c) MRI. (d) Metastasis, pathological fracture primary in the lung.
Miscellaneous
Degenerative arthritis may also involve the acromioclavicular joint. The radiological appearances include narrowing of the joint space, lack of paraarticular osteoporosis, eburnation and enthesopathy. Subluxation is a later phenomenon (Figure 18a,b). A pesudojoint may be formed between the conoid tubercle and the coracoid process (Figure 18c).

Figure 18: (a,b) Degenerative arthritis. (c) Pseudojoint coracoclavicular area.
Caffey disease, otherwise called infantile cortical hyperostosis, often presents with diffuse periosteal reaction and cortical thickening. Clavicle is one of the common sites. The entire clavicle may be involved with sclerosis and new bone formation. It may be bilateral (Figure 19).
Figure 19: Caffey’s disease involving both clavicles.
Paget disease is considered to be an unusual metabolic disorder which may involve any part of the skeleton from head to toe. A viral theory has been proposed but no exact etiology is established so far. It may be monostotic or polyostotic. There are three phases, one – lytic, two – lytic and sclerotic and three – completely sclerotic. Main radiological features include involvement of the bone upto the articular end and the involved bone is bigger than the normal. In the clavicle sclerotic phase is more common (Figure 20a-d) [26]. Monostotic clavicular involvement is rare.
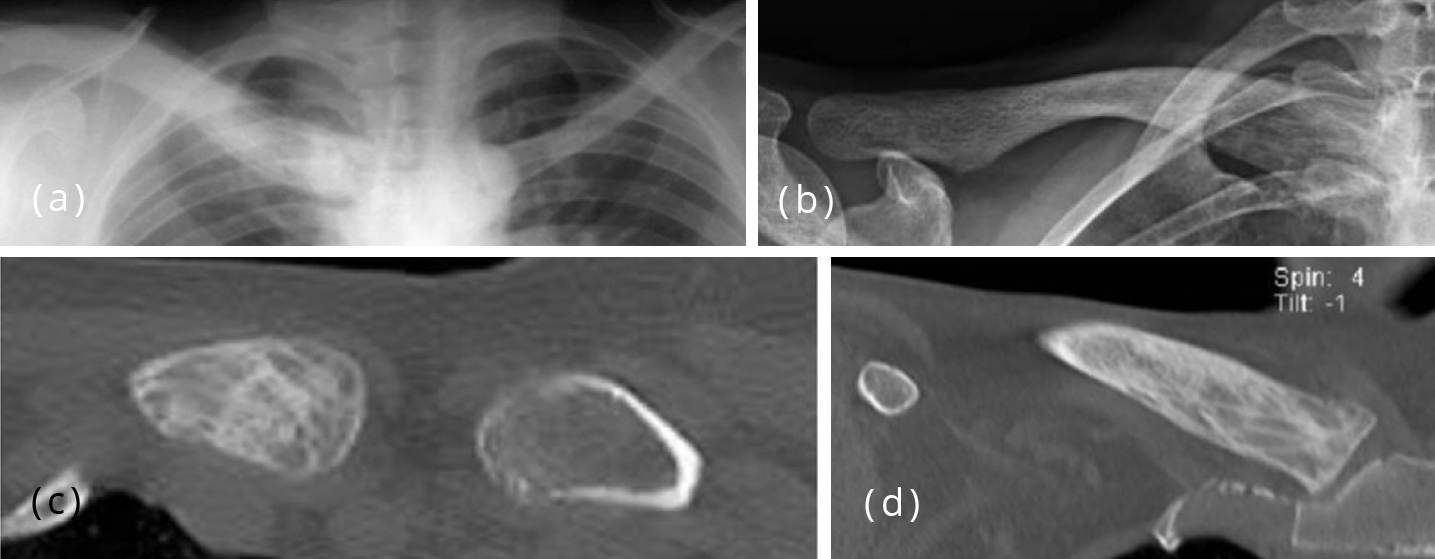
Figure 20: (a) Paget of right clavicle with diffuse sclerosis. (b-d) Paget medial end of clavicle.
Conclusion
The clavicle is not generally imaged except in trauma. Tumors of the clavicle are not common but one may encounter benign lesions such as osteoid osteoma, enchondroma and osteochondroma. The primary malignant bone tumors such as osteosarcoma, Ewing’s sarcoma, chondrosarcoma, plasma cell myeloma, and their radiological features are described. Tumoral lesions like condensing osteitis, tuberculosis, Langerhans cell histiocytosis may pose difficulty in diagnosis and the differentiating features are illustrated. Miscellaneous lesions like metastasis and metabolic disorders are also shown. Paget disease which rarely involves the clavicle is illustrated.
Acknowledgements
NIMS, KIMS, KREST Museum Hyderabad
Conflicts of interest
Author declares no conflicts of interest.
References
[1] Kumar R, Madewell JE, Swischuk LE. The clavicle: Normal and abnormal - RadloGraphics. 1989; 9(4):677–706. Available from: https://pubs.rsna.org/doi/pdf/10.1148/radiographics.9.4.2756192
[2] Kapoor S, Tiwari A, Kapoor S. Primary tumours and tumorous lesions of clavicle – Int Orthop. 2008; 32(6):829–834.
[3] Priemela MH, Stiel N, Zustin J, Luebke AM, Schlickewei C, et al. Bone tumours of the clavicle: Histopathological, anatomical and epidemiological analysis of 113 cases - J Bone Oncol. 2019; 16:100229.
[4] Dwivedi AD, Shukla R, Gaharwar S, Patwari S. Duplication of clavicle, poorly understood and a very rare incidental congenital anomaly: Radiographic and multislice CT demonstration. Available from: https://www.eurorad.org/case/9376
[5] Kabbani AA, Bhattacharya B. Cleidocranial dysostosis. Radiopaedia. Available from: https://radiopaedia.org/articles/cleidocranial-dysostosis [6] Magni F. Handlebar Clavicle. Available from: https://www.gamuts.net/display.php?id=12293
[7] Royal SA. Taybi, and Lachman's Radiology of Syndromes, Metabolic Disorders and Skeletal Dysplasias, 5th ed. - American Journal of Roentgenology. 2008; 190(3):W226-W226. Available from: https://www.ajronline.org/doi/full/10.2214/AJR.07.3136
[8] Kakarla S. Imaging in fibrous dysplasia. J Med Sci Res. 2013; 1(2):74–81.
[9] Kakarla S. Imaging spectrum of Osteogenesis Imperfecta – Pictorial essay. J Med Sci Res. 2019; 7(4):109–114.
[10] Khoshhal K, Letts RM, Mehlman CT. Subacute Osteomyelitis (Brodie Abscess). Medscape. Available from: http://emedicine.medscape.com/article/1248682-overview#a0101
[11] Gandhi A. Tuberculosis affecting the left sternoclavicular joint. Radiopaedia. Available from: https://radiopaedia.org/cases/tuberculosis-affecting-the-left-sternoclavicular-joint
[12] Greenspan A, Gerscovich E, Szabo RM, Matthews JG. Condensing osteitis of the clavicle: A rare but frequently misdiagnosed condition. AJR Am J Roentgenol. 1991; 156(5):1011–1015.
[13] Mitra R. Osteitis condensans ilii. Rheumatol Int. 2010; 30(3):293–296. [14] Khanna L, El-khoury GY. SAPHO Syndrome – A pictorial assay. The Iowa Orthop J. 2012; 32:189–195.
[15] Bennett J, Suliburk JW, Morón FE. Osseous manifestations of primary hyperparathyroidism: Imaging findings - Int J Endocrin. 2020; 3146535. Available from: https://doi.org/10.1155/2020/3146535
[16] Kakarla S. Radiology of crystal arthropathies. J Med Sci Res. 2015; 3(4):187-191.
[17] Davies M, Cassar-Pullicino VN, Davies AM, Mc-Call IW, Tyrrell PN. The diagnostic accuracy of MR imaging in osteoid osteoma. Skeletal Radiol. 2002; 31(10):559–569.
[18] Kakarla S. Benign Cartilaginous Lesions. J Med Sci Res. 2013; 1(1):29-36.
[19] Kakarla S. Imaging of langerhans histiocytosis - Pictorial essay. J Med Sci Res. 2017; 5(1):33–39.
[20] Kakarla S. Imaging Approach to Malignant Bone Tumors. Nepalese Journal of Radiology. 2013; 3(1):1–13.
[21] Abdehgah AG, Molavi B, Mehrpour SR, Radmard AR, Mahjori M, et al. Clavicular Chondrosarcoma: A Case Report and Brief Review of the Literature. Int J Hematol Oncol Stem Cell Res. 2016; 10(3):191–194.
[22] Deng F, Muzio BD, et al. Plasmacytoma. Radiopaedia. Available from: https://radiopaedia.org/articles/plasmacytoma
[23] Filho AGO, Carneiro BC, Pastore D, Silva IP, Yamashita SR, et al. Whole-Body Imaging of Multiple Myeloma: Diagnostic Criteria. RadioGraphics. 2019; 39(4):1077–1097.
[24] Bickle I, Knipe H, et al. Primary bone lymphoma. Radiopaedia. Available from: https://radiopaedia.org/articles/primary-bone-lymphoma
[25] Kakarla S. Imaging of blow out metastases of bone Pictorial essay. J Med Sci Res. 2016; 4(4):181–189. [26] Kakarla S. Paget disease of skeleton – Pictorial essay. J Med Sci Res. 2014; 2(1):34–40.