Full Text
Introduction
The scapula (shoulder blade) is a flat, broad and triangular bone, which lies obliquely over the posterior aspect of the chest wall extending over the first seven ribs bilaterally. It consists of two surfaces, three borders and three angles. Enneking et al. [1], have given a classification system for diagnosing the tumors of the shoulder girdle. Accordingly, the scapula is divided into two zones, one, the acromio glenoid complex designated as S2 region and two, the spine and blade portion as S1 region, as illustrated in (Figure 1). This system helps the surgeon for resections and reconstructions.
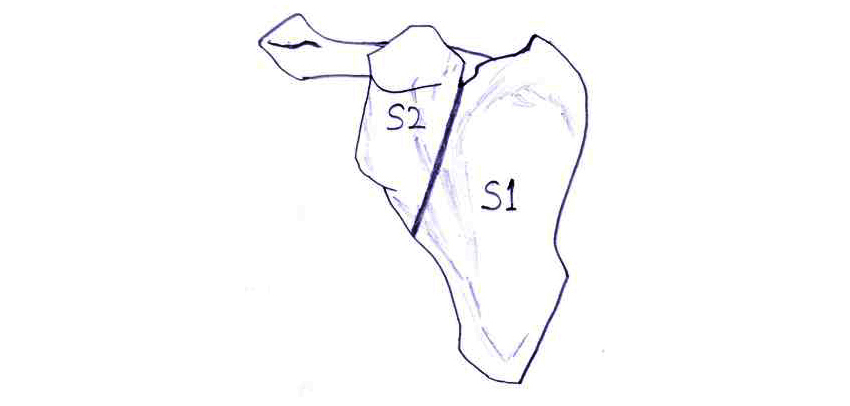
Figure 1: Diagram showing the system for classification of skeletal resection advised by committee of Muskuloskeletal Tumor Society. S1 – Blade of scapula, S2 – Glenoid acromial complex.
The tumors of the S1 region are those that commonly develop in flat bones such as, osteosarcoma, round cell tumor, chondrosarcoma and multiple myeloma. The tumors that develop in S2 region include those that commonly develop at the ends of the long bones, which include osteochondroma, giant cell tumor and chondroblastoma. Other focal lesions include developmental, infective, Langerhans cell histiocytosis and other benign miscellaneous lesions such as, hydatid cyst, radiation induced malignancies etc. Systemic benign disorders, such as skeletal dysplasias, metabolic and haematological may also involve the scapula (Table 1).
Table 1: Lesions of the scapula: Focal and systemic.
|
Focal
|
Systemic
|
- Developmental
- Inflammations
- Infections
- Neoplastic – benign & malignant
|
- Dysplasias
- Metabolic
- Hematological
- Neoplastic – Malignant, metastasis, myeloma and lymphoma.
|
The simple and most preferred investigation is conventional radiography. However, recent imaging modalities such as, MDCT, MRI, scintigraphy and PET-CT are adopted to arrive at a definitive diagnosis. The imaging methods are listed in Table 2. The benign neoplasms are listed in Table 3, tumor like lesions in Table 4 and malignant lesions in Table 5.
Table 2: Imaging methods.
- Conventional/Digital
- MDCT
- MRI
- Radionuclide Scan
- PET-CT
|
Review of the literature
The literature is scanty regarding the tumors and tumoral lesions of scapula. However Enneking et al. [1] mentioned the division of scapula into two major areas which helps the surgeon for resections and reconstructions of the tumors. Blacksin et al. [2] described the radiological findings of neoplasms of the scapula. Tumoral conditions were included in the article by Brtkova et al. [3]. Several other authors have mentioned individual entities and described the radiological findings but not in a consolidated fashion.
Discussion
Tumors of the scapula are relatively rare. Statistically, most frequently encountered include are tumours of cartilaginous origin. In our experience, more than 1/3 of all cases are osteochondromas, which show a typical appearance radiologically. These are encountered predominantly in the first 3 decades in males and are located most often in the body of the scapula. The other benign tumors include osteoma, osteoid osteoma, osteoblastoma, hemangioma, aneurysmal bone cyst and giant cell tumor (Table 3). The tumoral conditions include cystic type of osteomyelitis, Langerhans cell histiocytosis and simple bone cyst. Radiological manifestations have been described by several authors [4-7]. The most common malignant lesion of the scapula is chondrosarcoma, which generally occurs in the 4th-7th decades of age. Chondrosarcoma is located mainly at the lateral scapular margin over the inferior angle, in the acromion and coracoid process and their appearances range from typical characteristics to falsely benign lesions. The other primary malignant tumors include osteosarcoma, Ewing’s sarcoma, plasmacytoma, lymphoma, hemangioendothyleoma and malignant fibrous histiocytoma. Of all the malignant bone tumors, metastases are the most common. The primary sites include majorly, carcinoma of the breast, lung, kidney and thyroid [8]. Infact, any primary malignancy from any organ can produce metastases in the bones. The radiological appearances vary from lytic, mixed to diffusely sclerotic. Sclerotic metastases are primarily from carcinoma of the prostate, but can be from carcinoids, malignancies from gastrointestinal and genitourinary tracts. Soft tissue lesions such as, fibromatosis may involve scapula [9]. Metabolic and endocrine disorders may reflect upon scapula [10]. Hemoglobinopathies and malignancies of the hemopoietic system, eg. Leukemia and lymphoma may involve the scapula. Miscellaneous lesions include Paget disease. These may be confined to scapula but most often these are polyostotic [11, 12].
Imaging spectrum:
Table 3: Benign bone tumors.
- Osteoid osteoma
- Osteoblastoma
- Osteochondroma
- Hemangioma
- Aneurysmal bone cyst
- Giant cell tumor
- Neurofibroma/Schwannoma – focal or in NF1
|
Osteoid osteoma
It is a rare benign bone neoplasm, mostly occur in long bones. Osteoid osteoma of the scapula is quite rare. A focal sclerotic lesion is noted with a central lucent nidus. This may not be obvious on conventional films. CT is the best mode of imaging. However, MRI and radio nuclide scans may also be adopted. Radiological appearances of osteoid osteoma are the same as noted elsewhere in the body. Identification of the nidus is essential for which CT scan may be preferred (Figure 2).

Figure 2: CT osteoid osteoma, note the nidus.
Osteoblastoma
It produces excessive new bone formation with a large nidus more than 2cms in diameter. The nidus may be obscured by new bone. It is rare in the scapula. CT is essential to confirm the diagnosis (Figure 3). There is no preferential site for this in the scapula.
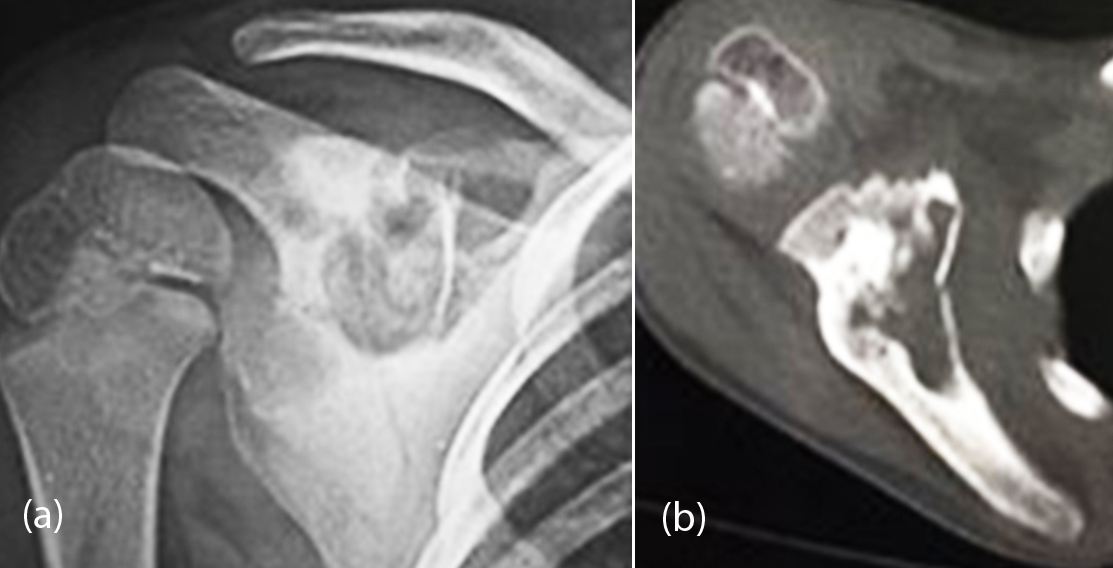
Figure 3: Osteoblastoma, (a) Plain radiograph, (b) CT showing the large nidus and new bone formation.
Osteochondroma
This is the most common primary benign neoplasm of the scapula. Usually, it is a single lesion located on the anterior surface of the scapular body like an osteocartilaginous exostosis. The radiologic presentation of osteochondroma is characterized depending on whether the lesion is pedunculated with a narrow pedicle or, sessile with a broad base of implantation in the cortex. The most important feature is the long continuity of the cortical bone with the cortex of osteochondroma (Figure 4a-c). Other important features are calcifications in the cartilaginous cap with a thickness which ranges from 1mm-3mm. This is better displayed on MRI as a cap of high intensity in gradient echo sequences and T2 weighted images. Osteochondroma may be a part of hereditary multiple exostoses (Figure 4 d, e). Complications of osteochondroma include compression of nerves, blood vessels, fracture and bursal formation (Figure 4f). Deformity and malignant transformation to chondrosarcoma are the other complications. Enchondromas and other cartilaginous lesions such as, chondroblastoma rarely involve the scapula.

Figure 4: (a, b) Sessile osteochondroma of the scapula; (c) Osteochondroma arising from the scapula; (d, e) Multiple hereditary exostoses involving the scapula and humerus; (f) CT exostosis bursatum (white arrow).
Hemangioma
It is a benign vascular tumor, which commonly occur in the vertebral bodies and skull. They may be capillary, cavernous, or venous. In the skull, they produce a spoke wheel appearance. Hemangiomas of the scapula are rare and the capillary hemangiomas produce the same radiological appearance as seen elsewhere. Cavernous hemangiomas produce large lucent areas with little surrounding sclerosis (Figure 5a). Scapula may be involved in cystic angiomatosis of the skeleton which is a diffuse systemic disorder. Multiple lucent areas are noted with surrounding sclerosis (Figure 5b).
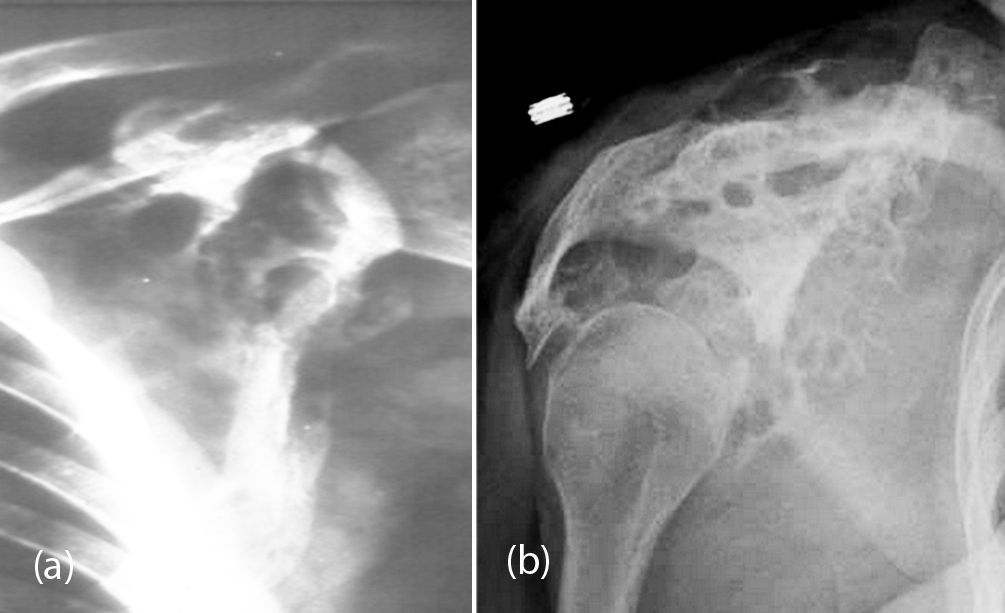
Figure 5: (a) Cavernous hemangioma, (b) Cystic angiomatosis.
Aneurysmal bone cyst (ABC)
This accounts for 6% of primary lesions of bone. It occurs in children younger than 20 years old. Histologically, it consists of multiple sinusoids filled with blood, alternating with more solid areas. Multicystic eccentric lucencies involves the bone with a thin shell of periosteal response. Conventional radiography may be sufficient for diagnosis (Figure 6a, b). But the use of MDCT allows us to assess the cortical bone and fine internal septa (Figure 6c-f). MRI findings are quite characteristic showing a well-defined lesion with a lobulated edge and cystic cavities with fluid-fluid levels (Figure 6g-i). Secondary ABC’s may be encountered in giant cell tumors, chondroblastoma and some malignant tumors, such as telangiectatic osteosarcoma.
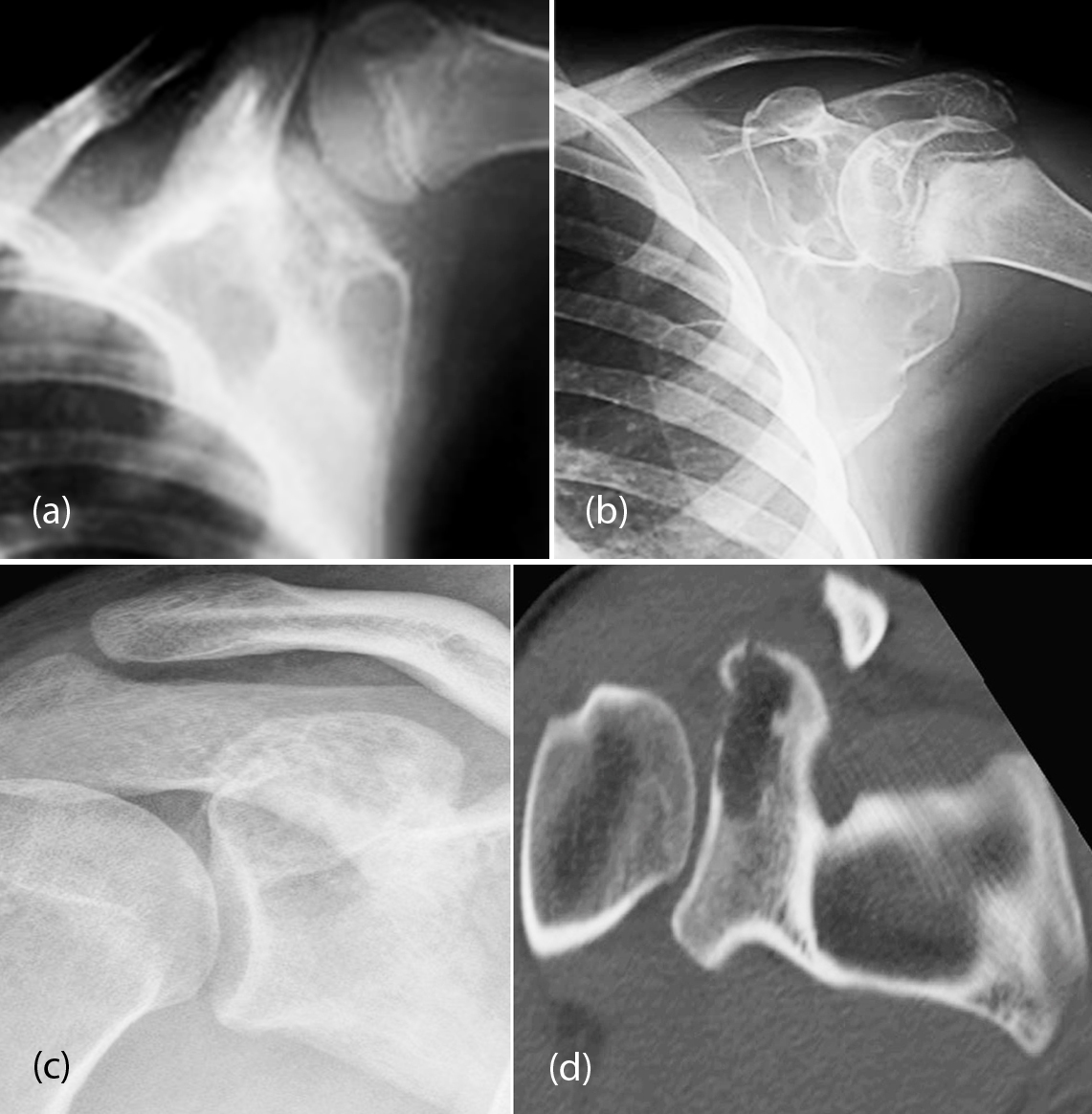
Figure 6a-d: (a, b) ABC of scapula; (c, d) ABC of the glenoid; (c) Plain, (d) CT.
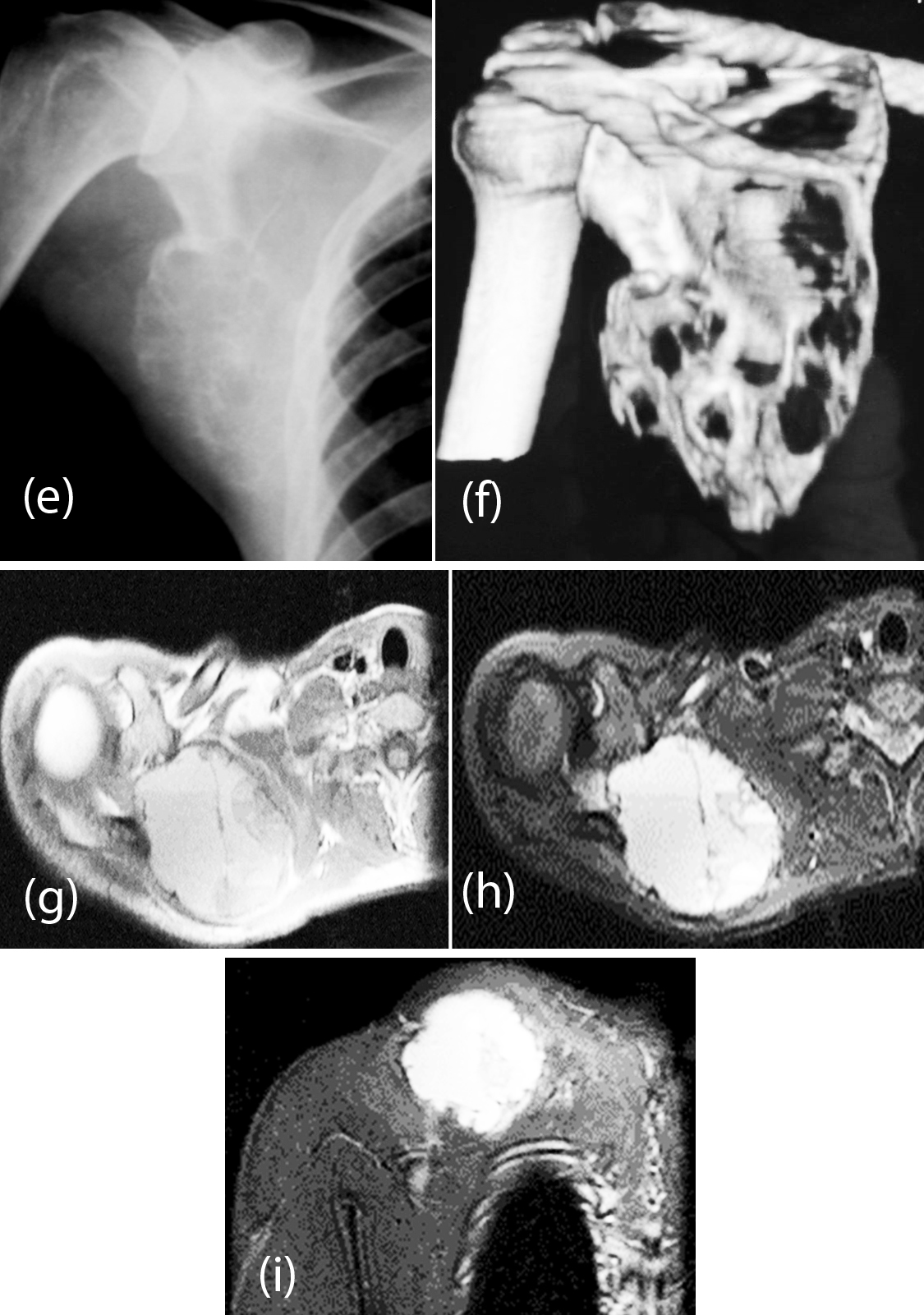
Figure 6e-i: (e, f) ABC; (e) Plain film, (f) 3d CT; (g, h, i): MRI ABC of scapula (note the fluid levels).
Giant cell tumor
It is an aggressive lesion characterized by a highly vascularized tissue containing stromal cells and osteoclasts. It affects men and women between 20-40 years old, although more common in women. Radiologically displayed an osteolytic lesion with a thin margin and narrow-transition. In general no periosteal reaction is noted unless there is a fracture. There is usually a soft tissue mass when the cortex is broken. CT and MRI play an important role in studying the matrix and soft tissue components. These benign bone tumors generally occur in the ends of long bones. In the flat bones they occur near the articular margins. Radiologically a lucent lesion with trabeculae in the matrix giving a soap bubble appearance is noted. They may be aggressive with cortical disruption with a pathological fracture. The margins of the lesion are rarely sclerotic (Figure 7a, b). In the differential diagnosis, aneurysmal bone cyst and chondroblastoma are to be considered. Infact, giant cell tumor and aneurysmal bone cyst may coexist in about 20% of cases.
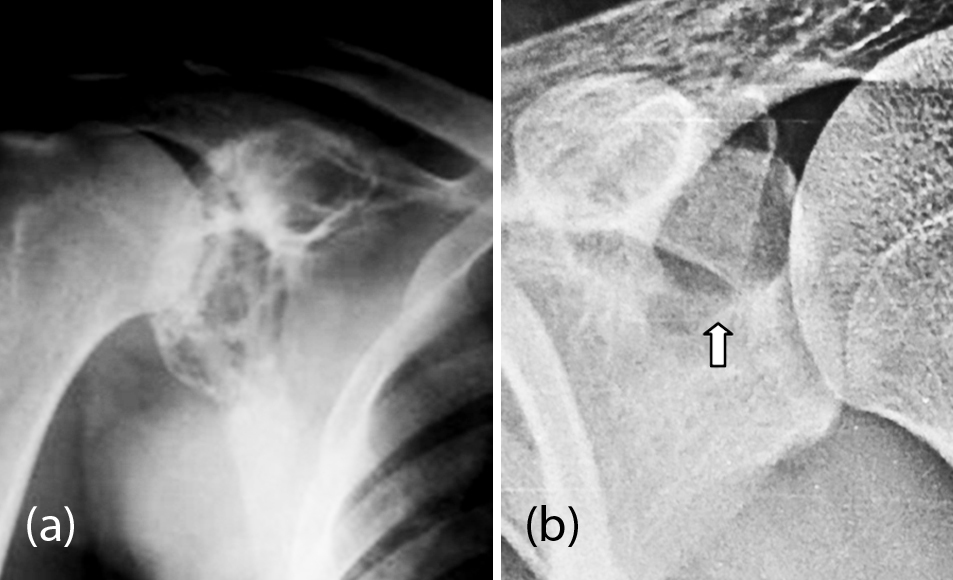
Figure 7: (a) 30M, Giant cell tumor involving the glenoid; (b) 25M, GCT involving the superior portion of the glenoid.
Neurofibroma/ Schwannoma
These are very rare tumors primarily arising from the scapula. However, in neurofibromatosis 1 (NF1) the scapula may be involved with associated mesenchymal dysplasia. Localised neurofibroma may produce irregular lucent defect in the scapula with variable surrounding sclerosis. It is a histological diagnosis. However, in NF1 patients, it can be diagnosed because of the associated findings in the rest of the body. Distortion of the architecture of the scapula is noted with variable lucencies with surrounding sclerosis (Figure 8a, b).
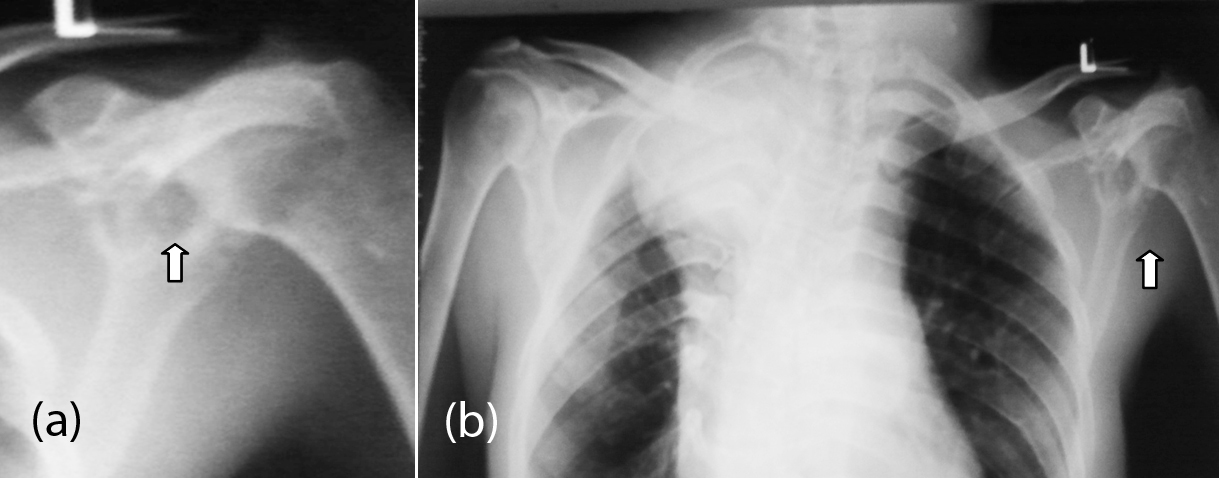
Figure 8: (a) Neurofibroma of left scapula, (b) same patient chest in NF1.
Table 4: Primary malignant neoplasms of the scapula.
- Osteosarcoma
- Ewing sarcoma
- Chondrosarcoma
- Fibrosarcoma/ Malignant fibrous histocytoma
- Lymphoma
- Plasmacytoma/ Multiple myeloma
- Hemangioendothelieoma
|
Osteosarcoma
It is a relatively frequent malignant neoplasm of the scapula. Occurs between 11 and 30 years. Several histological types, such as chondroblastic, osteoblastic and telangiectatic types have been reported. Radiological features include an amorphous, osteoid tumor and bone density with bulky soft-tissue masses (Figure 9a, b). Sun ray spicules may extent to the soft tissues. It may be lytic with broken cortex and extend into the soft tissues.
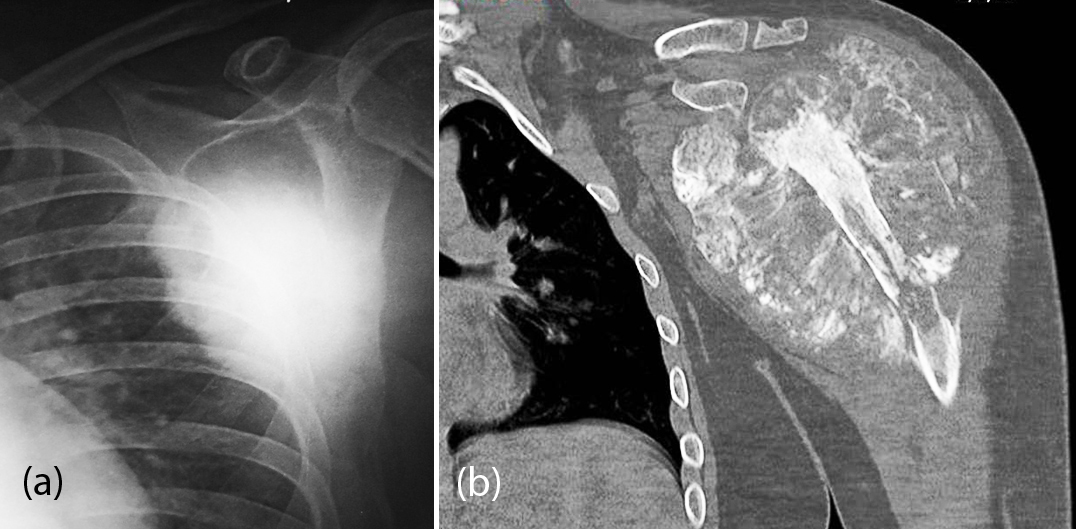
Figure 9: Osteosarcoma of the scapula; (a) Osteoblastic, (b) Classical.
Chondrosarcoma
It is the most common malignant neoplasm of the scapula. Chondrosarcoma is a malignant bone tumor producing cartilage. Its main radiological features include an expansive lesion, disruption of bone, annular calcifications and comma-shaped tumor matrix, thickening of the bone cortex, and the presence of soft tissue mass (Figure 10a, b). Secondary chondrosarcoma arising from exostosis may be seen but radiological characteristics include the appearance of the pre existing lesion with a thick cartilage (Figure 10c).
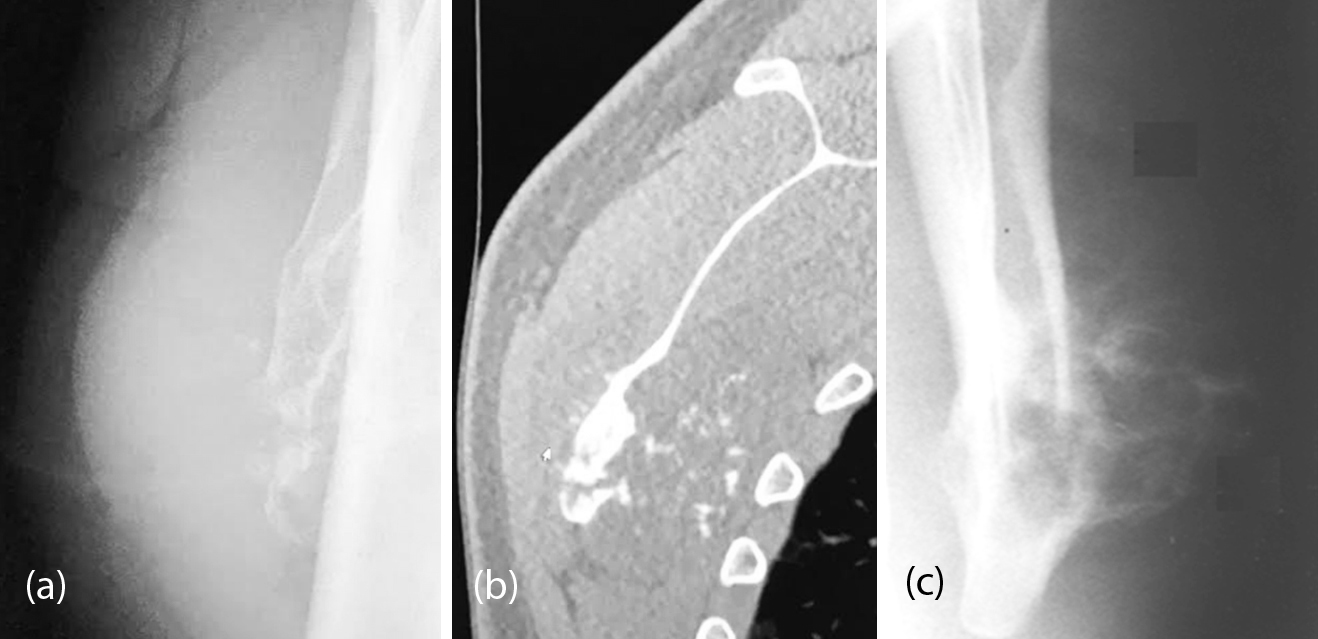
Figure 10: Primary chondrosarcoma of the scapula; (a) Tangential plain film, (b) CT; (c): Malignant transformation of osteochondroma.
Ewing sarcoma
This is commonly encountered in the long bones and pelvic bones. It may be encountered in the scapula. The age is between 5-30 years. From the radiological point of view it is permeable lytic lesion with a large soft tissue mass. Reactive new bone may be seen (Figure 11a, b). Soft tissue mass is better demonstrated by CT/MRI (Figure 11c).
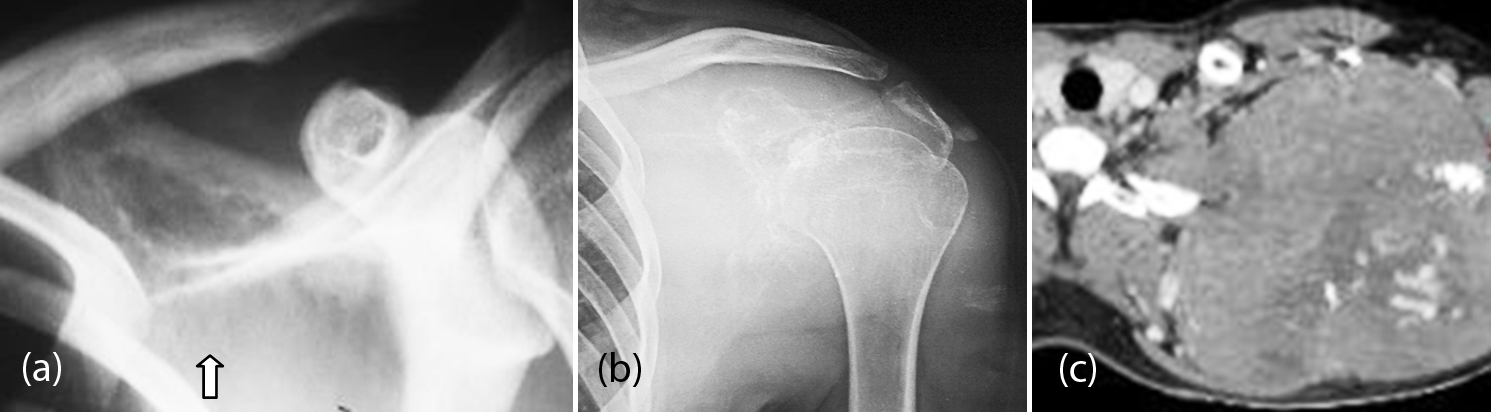
Figure 11: Ewing Sarcoma; (a) Supra scapular, (b) Body, (c) CT of the same.
Fibrosarcoma/ Malignant fibrous histiocytoma
Most of the malignant fibrous histiocytomas were designated as fibrosarcomas in the previous years. It is a primary bone tumor of the appendicular skeleton and can occur at any age Radiological features are non specific which include a lytic lesion with cortical destruction and soft tissue mass. It is difficult to differentiate from fibrosarcoma (Figure 12). On MR imaging, malignant fibrous histiocytoma, often shows only heterogeneously increased signal intensity on T2-weighted sequences.

Figure 12: Malignant fibrous histiocytoma.
Multiple myeloma
This originates from plasma cells of the bone marrow. This is the most common primary malignant bone tumor. It occurs between 50-70 years of age. From the radiological point of view a localised form known as plasmacytoma shows a large lytic lesion with well-defined borders. Multiple myeloma is more commonly encountered than plasmacytoma in scapula. Multiple well defined lytic lesions, diffuse infiltrative pattern and moth eaten lytic areas are common radiological findings (Figure 13a, b).
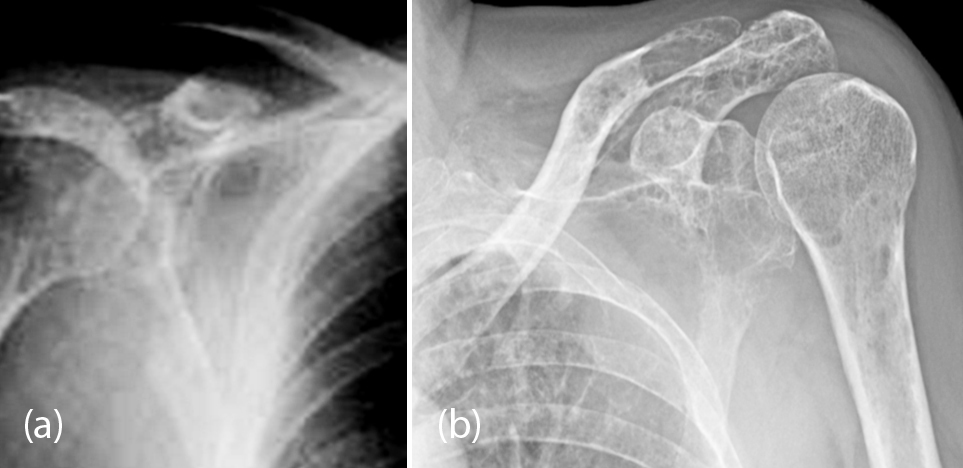
Figure 13: (a, b) Multiple myeloma involving the scapulae.
Lymphoma, leukemia
Isolated lymphoma/ leukemia involving the scapula is quite rare. However, scapular involvement in systemic lymphoma is occasionally noted. Based on radiological findings, it is difficult to make a firm diagnosis. It may be lytic, sclerotic or mixed (Figure 14a, b, c).

Figure 14: Lymphoma; (a) Plain film, (b) CT showing para aortic enlarged nodes, (c) CT of scapula.
Metastatic disease
They are the most common malignant bone tumors. It should always be taken into account in the differential diagnosis when dealing with malignant bone tumors, particularly in older patients. By frequency, carcinomas of the breast, lung, thyroid, kidney and prostate are responsible for most of the metastasis. While expanding osteolytic lesions are common from primary neoplasms of the kidney, lung, breast, thyroid and gastrointestinal tract, osteoblastic lesions are common in carcinoids, gastrointestinal tract and prostatic malignancies (Figure 15).
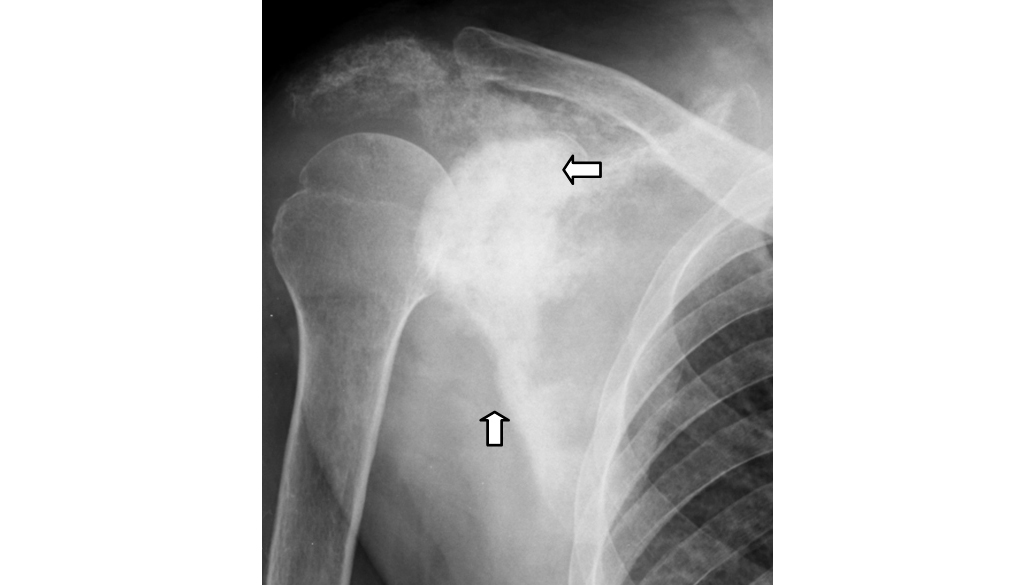
Figure 15: Prostatic metastasis to scapula.
Tumor like lesions of scapula are listed in Table 5.
Table 5: Tumor like lesions.
- Congenital glenoid dysplasia
- Gorham disease
- Langerhans histiocytosis X
- Brodie’s abscess
- Tuberculosis
- Brown tumors of hyperparathyroidism
- Fibrous dysplasia
- Paget disease
|
Congenital glenoid dysplasia
It can be unilateral or bilateral and the etiology is similar to acetabular dysplasia. It is characterized by underdevelopment of the bony glenoid and adjacent part of the scapular neck which may be seen as isolated. However, it is also noted in several syndromes and in patients with mucopolysaccharidoses. Radiologically, the findings vary with the degree of the dysplasia. The normal concavity of the glenoid fossa assumes a flat shape with a short neck, elongation of the glenoid and changes in the shape of the coracoid and clavicle. The glenoid typically shows notching and irregularity in its inferior aspect. In long standing cases secondary changes may occur in the head and neck of the humerus [9-11] (Figure 16a, b).

Figure 16a, b: Glenoid dysplasia: (b) 1-year-old – glenoid dysplasia (note the inferior notch).
Gorham syndrome
Gorham disease is also known as Gorham vanishing bone disease and phantom bone disease. It is a very rare skeletal lesion of unknown cause although vascular origin is postulated. Radiologically, extensive and progressive lytic lesions are noted which extend to the adjacent bones (Figure 17). These consist of thin-walled vascular or lymphatic channels within bone, which lead to resorption of bone.
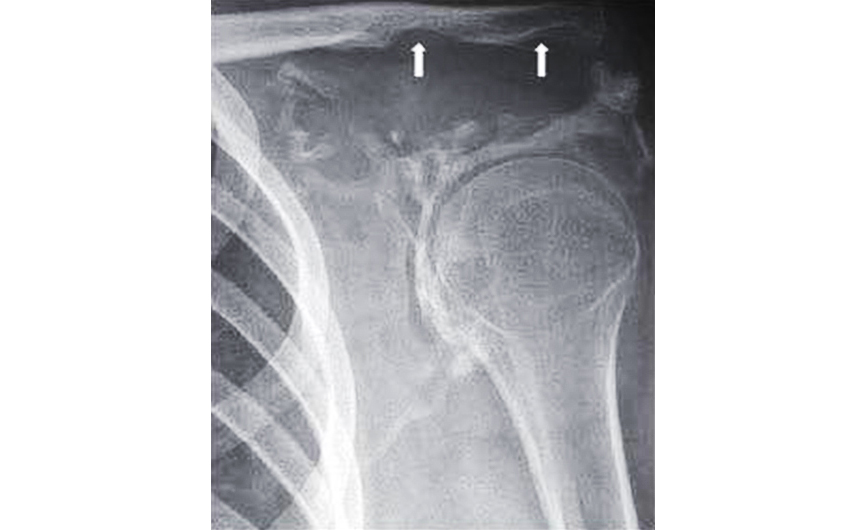
Figure 17: Gorham disease (note the large lytic areas).
Inflammatory
Langerhans cells histiocytosis/ local manifestation as eosinophilic granuloma is a non-neoplastic proliferation characterized by granulomatous reticular cells. Usually occurs in children aged 1 to 15 years. The most common sites are the flat bones, spine, skull and long bones. These are lytic lesions, polyostotic, which may show an aggressive look like with destruction of cortical bone and soft tissue mass. CT demonstrates a lytic lesion with scalloped borders (Figure 18). MRI most often displays a focal lesion surrounded by a large area of alteration of signal due to a reaction of soft tissue and bone marrow, with low signal intensity on T2 is considered to correspond to bone marrow edema or parts soft due to the flare phenomenon.
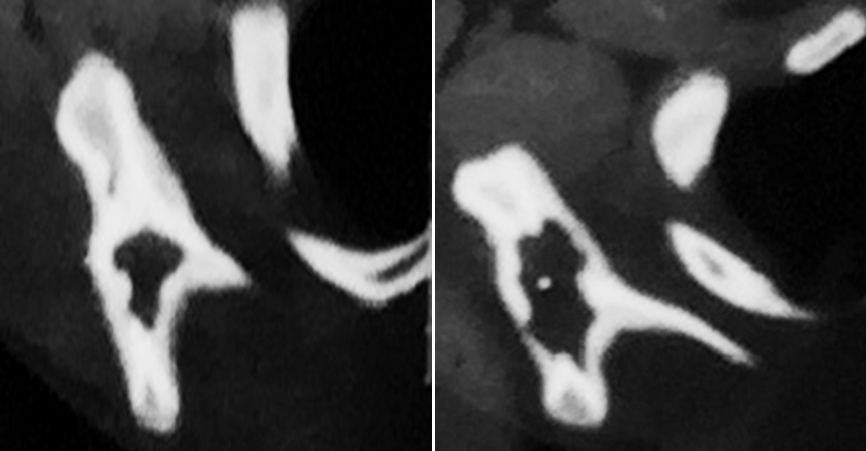
Figure 18: CT – Eosinophilic granuloma of scapula.
Infections
Infectious disease is represented by osteomyelitis of the scapula. It can be acute, subacute or chronic. Radiologically, the subacute form assumes Brodie’s abscess with a central lucency surrounded by sclerosis (Figure 19a). The etiology may be bacterial or fungal (Figure 19b). Tuberculosis primarily involving the scapula is very rare. However, cystic type of tuberculosis may be encountered in children (Figure 19c).
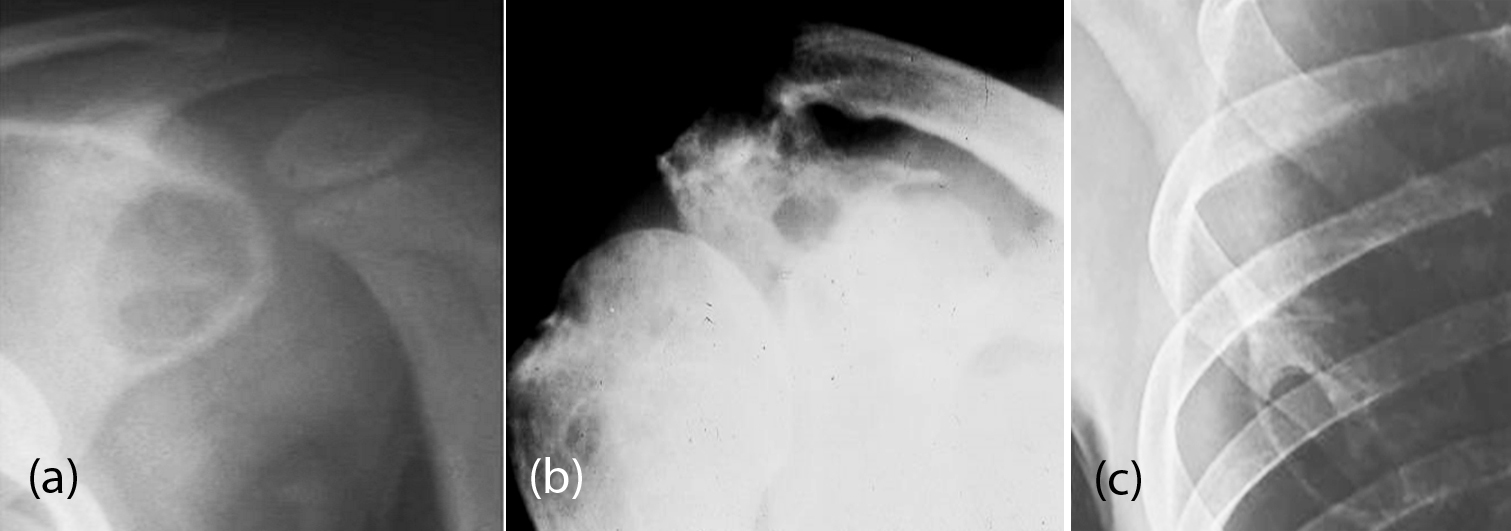
Figure 19: (a) Subacute osteomyelitis of the scapula – Brodie’s abscess; (b) Actinomycosis; (c) Tuberculosis of scapula (note the cystic nature).
Brown tumors
In both primary and secondary hyperparathyroidism, brown tumors in bones are encountered, although rare in scapula. Radiologically, a lytic lesion with ill-defined borders is noted in an osteoporotic bone (Figure 20a). In secondary hyperparathyroidism, brown tumors are associated with osteosclerosis (Figure 20b).
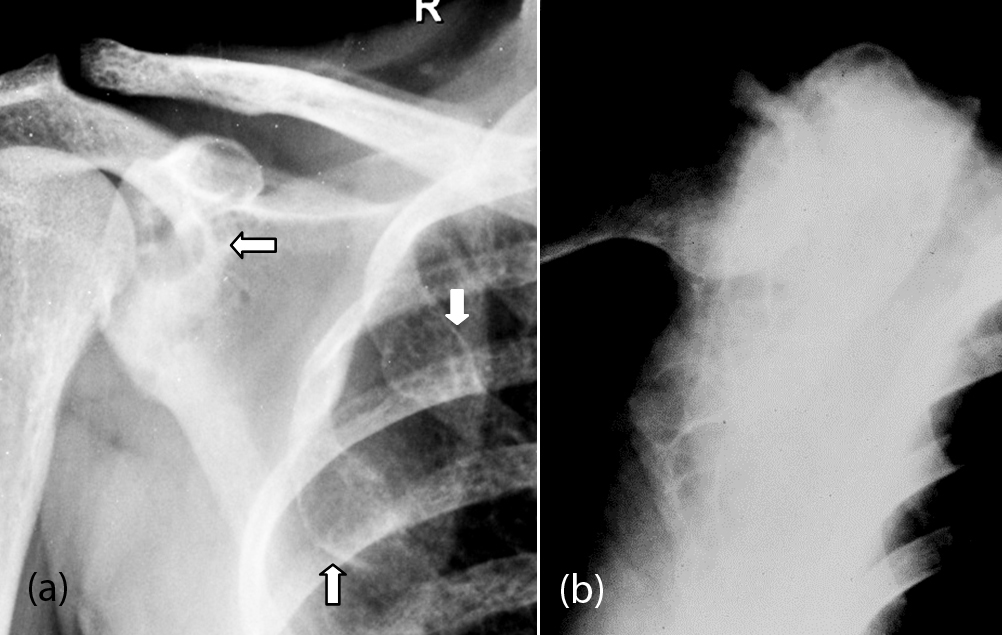
Figure 20: Brown Tumors of hyperparathyroidism; (a) Scapula and ribs, (b) Scapula.
Fibrous dysplasia
It is an aberrant formation of fibrous tissue in the bone and is developmental in origin. It can be monostotic, polyostotic or associated with other syndromes. Radiologically, it may appear as a lucent lesion with a sclerotic rind (Figure 21a, b). It may also be mixed, sclerotic and lucent (Figure 21c). Rarely, it is purely sclerotic with a matrix of ground-glass appearance.
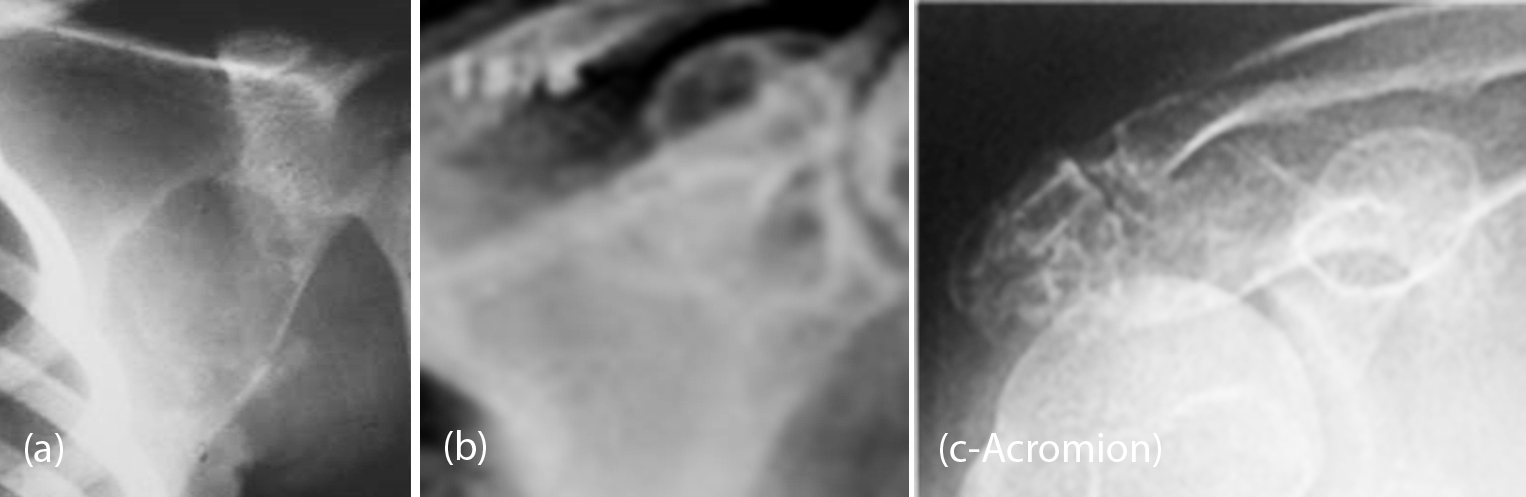
Figure 21: Fibrous dysplasia, (a) Cystic type, (b, c) Mixed type.
Hemangiopericytoma
This tumour is frequently encountered in middle-aged adults (4th decade). However, scapula is a rare site. Hemangiopericytoma, arises from the cells of Zimmerman, which surround vessels. Both benign and malignant forms are encountered. Radiologically the appearance varies from aneurysmal bone cyst to hemangioma of bone.
Conclusion
Non traumatic isolated scapular lesions are not uncommon. The etiology includes congenital, inflammatory, infective, neoplasms of benign and malignant nature. Systemic disorders include endocrinal, metabolic and neoplastic. Conventional radiography is adequate to make an initial diagnosis. However, advanced imaging combined with laboratory and histology findings is necessary to make a firm diagnosis. Imaging features of various entities involving the scapula are described with the help of illustrations.
Acknowledgements
NIMS, KIMS, KREST Museum Hyderabad, India.
Conflicts of interest
Author declares no conflicts of interest.
References
[1] Enneking W, Dunham W, Gebhardt M, Malawar M, Pritchard D. A system for the classification of skeletal resections. Chir Organi Mov 1990; 75(suppl 1): 217–240.
[2] Marcia MF, Joseph B. Neoplasms of the scapula – Pictorial essay; American Journal of Roentgenology, 2000; 174:1729–1735.
[3] Pourfeizi HH, Sales JG, Elmi A, Tabrizi A. Osteoid osteoma of a scapula: a case report in a 34 years old woman. Med J Islam Repub Iran. 2012; 26(3):143–146.
[4] Sharma R, Weerakkody Y et al. Osteoblastoma; Radiopaedia, RID:10960.
[5] Brtková J1, Nidecker A, Zídková H, Jundt G. Tumours and tumour-like lesions of scapula, Acta Medica (Hradec Kralove). 1999; 42(3):103–110.
[6] Kakarla S. Benign Cartilaginous Lesions. J Med Sci Res. 2013; 1(1): 29–36.
[7] Nam SJ, Kim S, Lim BJ, Yoon CS, Kim TH, et al. Imaging of primary chest wall tumors with radiologic-Pathologic correlation. Radiographics. 2011; 31:749–770.
[8] Ogose A, Sim FH, O'Connor MI, Unni KK. Bone tumors of the coracoid process of the scapula. Clin Orthop Relat Res. 1999; 358:205–214.
[9] Currarino G, Sheffield E, Twickler D. Congenital glenoid dysplasia. Pediatr Radiol. 1998; 28(1):30–37.
[10] Wirth MA, Lyons MB, Rockwood CA. Hypoplasia of the glenoid. A review of sixteen patients. J Bone Joint Surg Am. 1993; 75(8):1175–1184.
[11] Resnick D, Walter RD, Crudale AS. Bilateral dysplasia of the scapular neck. AJR Am J Roentgenol. 1982; 139(2):387–389.
[12] Cory DA, Fritsch SA, Cohen MD, Mail JT, Holden RW, et al. Aneurysmal bone cysts: imaging findings and embolotheraphy. AJR Am J Roentgenol. 1989; 153(2):369–373.
[13] Kakarla S. Imaging of blow out metastases of bone-Pictorial essay. J Med Sci Res. 2016; 4(4):181–189.
[14] Robbin MR, Murphey MD, Temple HS, Kransdorf MJ, Choi JJ. Imaging of Musculoskeletal Fibromatosis. Radiographics. 2001; 21(33):585–599.
[15] Kakarla S. Musculoskeletal fluorosis- imaging spectrum, J Med Sci Res. 2013; 1(3):117–123.
[16] Kakarla S. Imaging in fibrous dysplasia. J Med Sci Res 2013; 1(2):74–81.
[17] Kakarla S. Paget disease of skeleton – Pictorial essay. J Med Sci Res. 2014; 2(1):34–40.
[18] Isaac J, Shyamkumar NK, Karnik SV. Intraosseus schwannoma. J Postgrad Med. 2004; 50:127–128.