Case Report
2016
December
Volume : 4
Issue : 4
Omental torsion with multiple congenital anomalies
Prasad MBV, Sanjeeva Rao K
Pdf Page Numbers :- 164-168
1Department of Surgical Gastroenterology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India
*Corresponding authors: Dr. MBV. Prasad, FRCS (UK), MS (PGI, Chandigarh), Consultant Surgical Gastroenterologist, Department of Gastroenterology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India. Email: bmallipudi@hotmail.com and Dr. Sanjeev, Department of Gastroenterology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India. Email: drsanjeevkommoju@gmail.com
Received 08 July 2016; Revised 23 August 2016; Accepted 01 September 2016; Published 08 September 2016
Citation: Prasad MBV, Sanjeeva Rao K. Omental torsion with multiple congenital anomalies. J Med Sci Res. 2016; 4(4):164-168. DOI: http://dx.doi.org/10.17727/JMSR.2016/4-036
Copyright: © 2016 Prasad MBV, et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: We report two rare cases with complete omental torsion with right sided inguinal hernia, maldescended testis and Meckel’s diverticulum along with review of literature.
Patients: Two patients presenting with acute abdomen and inguinal hernia, diagnosed preoperatively as omental torsion and undescended testis and Meckel’s diverticulum were managed operatively with omentectomy, hernioplasty and orchidectomy.
Results: Both patients recovered well postoperatively and have remained asymptomatic.
Conclusion: Omental torsion is one of the rare causes of acute abdomen and may mimic various other causes. It is quite often possible to diagnose preoperatively by USG and CT scan abdomen. Symptomatic patients with preoperative diagnosis need omentectomy preferably through laparoscopy.
Keywords: Omental torsion; inguinal hernia; maldescended testis; meckel’s diverticulum; laparoscopic omentectomy
Full Text
Introduction
Torsion of the omentum is a clinical condition in which the organ rotates on its long axis compromising its vascularity. Segmental torsion of the greater omentum is more common. Primary torsion of the omentum was first described in 1899 [1]. Omental torsion can be either primary (idiopathic) or secondary, depending on the predisposing factors that cause it. Primary torsion (idiopathic) is less common [2], whereas secondary torsion is associated with pre-existing conditions including longer than normal omentum, internal hernias, inflammatory pathologies of other organs such as acute cholecystitis, pancreatitis, and adnexitis, tumors, and postsurgical adhesions [2]. When the greater omentum is twisted around its axis, perfusion defects and vascular impairment of the organ are possible. As a result, different pathological modifications are possible, from simple edema to ischemia and gangrene of the omentum [3]. The condition is more common in males, with a ratio of 2:1 in the third decade of life and 5:1 in the fourth decade of life [2, 4], but it can occur at any age [5].
There are also predisposing factors such as sex, obesity, sudden strong increase in intra-abdominal pressure (brought on by coughing or violent exercise), trauma, large pedicle, (larger or more twisted than normal epiploic blood vessels), hyperperistalsis and surgical adherences causing displacement of the omentum [5, 6].
Omental torsion presents with wide variety of symptoms from moderate abdominal pain to mimicking acute appendicitis and could be a challenging task for preoperative clinical diagnosis. Ultrasound and computed tomography (CT) are useful tools for establishing a preoperative diagnosis [7, 8].
We report two rare cases with omental torsion with right sided inguinal hernia, maldescended testis and Meckel’s diverticulum.
Case 1
A 30-year-old male presented to KIMS hospital with pain in the right lower abdomen for one week and lump in the right groin for two months. The pain was initially mild to moderate for 4 days and then increased in severity and did not settle with medication. He was having a lump in the right groin for two months which was intermittent; disappearing on lying down and increasing on straining. There was no history of fever, vomiting, cough or weight loss. Bowel and bladder habits were normal. He had no other significant past medical history.
On examination, abdomen was soft with tenderness in right iliac fossa, no guarding, no rigidity. A swelling was noted in the right groin with positive deep ring occlusion test. Right testis could not be palpated. CT scan of the abdomen (Figure 1) showed omental inflammation and caking and with a diagnosis of omental torsion, he was posted for surgery. It was originally planned to excise the omentum through the inguinal incision, by extending it laterally. However, the omentum was noted to have torted much higher and could not be delivered into the groin incision. Laparoscopy was attempted, but was not successful due to the bulk of omentum and jejunal adhesions to the infarcted omentum.

Figure 1: CT scan showing omental inflammation and caking.
Intraoperatively we noted maldescended right testis lying in superficial inguinal pouch, Meckel’s diverticulum with wide base approximately 1 inch in length, normal sub caecal appendix, torted and infarcted omentum (Figure 2). Torsion was at the attachment of omentum to transverse colon, and proximal jejunal loops were adherent to the torted omentum. Therefore a decision was taken to proceed with laparotomy with omentectomy (Figure 3), right orchidopexy and repair of right inguinal hernia. Testis was fixed at the superficial inguinal ring as it could not be brought down further. Orchidectomy was not done at that time due to consenting issues. However in view of delayed diagnosis of maldescended testis he was advised to have orchidectomy, which he had six months later. Postoperatively he recovered well.

Figure 2: Omental torsion at laparotomy.
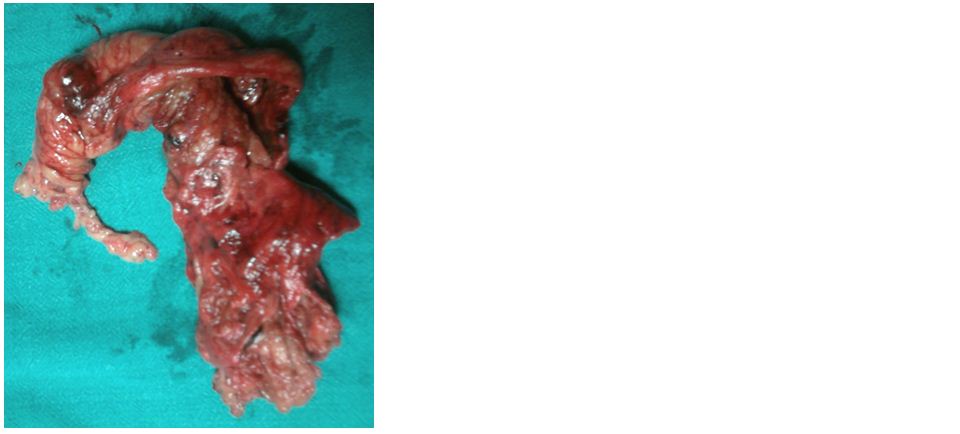
Figure 3: Resected omentum.
Case 2
A 51-year-old male presented to KIMS Hospital with pain in the right inguinal region and continuous fever for two days. He had a diagnosed right inguinal hernia since 2011. There was no history of vomiting, diarrhea, constipation or urinary symptoms. Bowel and bladder habits are normal. Patient was a known hypertensive on medication.
On examination, abdomen was soft with tenderness in right iliac fossa and right inguinal region. Swelling in the right inguinal region extending upto the base of scrotum, and was soft to firm in consistency and irreducible. Right testis could not be palpated. Ultrasonography showed free fluid in the right side of the pelvis with large right scrotal swelling with internal stranding. CT scan of the abdomen showed right sided inguinal hernia with omentum associated with torsion and minimal fluid. After preoperative blood investigations surgery was planned. Diagnostic laparoscopy showed omental torsion (Figure 4), right undescended intra-abdominal rudimentary testis and indirect inguinal hernia with torted omentum as content. Laparoscopic omentectomy with right open inguinal hernioplasty and right orchiectomy were done. Excised omentum (Figure 5) was delivered through the inguinal wound and sent for histopathology. He had an uneventful Recovery.

Figure 4: Omental torsion as seen at laparoscopy.

Figure 5: Resected omentum.
Discussion
Omental torsion is a kind of volvulus that occurs due to a twist in the omentum along its long axis and may result in ischemia and necrosis, and rarely presents as acute condition [7, 9]. Morris classified greater omental torsion into 11 subtypes depending on the presence or absence of hernia or tumor [10].Omental torsion is divided into two groups: primary and secondary [11]. The secondary type is more commonly seen.
Primary torsion is usually seen in children, particularly in the age range of 9 to 16 years. Although primary torsion does not have a known etiology, it is usually caused by benign conditions, such as obesity, and it is associated with anatomic variations, such as accessory, bifid, or tongue-shaped omental structures [12].
Secondary omental torsion is often associated with intra-abdominal pathologies, such as adhesion, hernia, giant abdominal tumor, and omental cyst [12, 13]. Although the etiologies of primary and secondary torsion are different, the triggering factors are similar. In both conditions, triggering factors such as a sudden increase in intra-abdominal pressure, including effort, coughing, and sneezing, cause the torsion due to the occurrence of a sudden shift in the omentum [13, 14].
The typical clinical features of omental torsion include pain of sudden onset and duration, which is usually constant and gradually increases in severity. Clinically, the differential diagnoses of omental torsion include acute appendicitis, acute cholecystitis, diverticulitis, epiloic appendagitis, caecal or sigmoid volvulus and many more [8]. Patients present with acute onset of severe abdominal pain that is localized to the right side of the abdomen in 80% of cases [15]. Nausea and vomiting may be present, but they are not predominant findings. The patient’s temperature is usually normal, and palpation of the abdomen demonstrates localized abdominal tenderness with guarding, suggesting peritonitis. A mass may be palpable if the involved omentum is sufficiently large. Most cases are often located in the right lower or upper quadrant. This has been attributed to an embryologic variant of the blood supply of the right portion of the omentum, predisposing to venous thrombosis [16].
US and CT play important roles in making an accurate preoperative diagnosis. Typical US findings are a hyperechoic, noncompressible, intrabdominal mass and central hypo-echoic changes [17, 18]. Diagnosis of omental torsion is rarely made preoperatively but should become more frequent with the increasing use of CT in the diagnosis of acute abdominal conditions [8]. The CT findings of fatty mass with a whirling pattern in the greater omentum suggest omental torsion. Although this typical CT finding has been documented in literature [19, 20], it should be made clear that not all omental torsions show this relatively characteristic appearance. The whirling pattern may not be apparent in cases where the axis of rotation is not perpendicular to the transverse scanning plane. The key to the correct diagnosis of omental torsion is the characteristic presence of concentric linear strands [21, 22].
Free serosanguinous fluid in the absence of any other intraabdominal pathology is another finding suggestive of omental torsion. When torsion occurs, venous return is compromised; the distal portion of the omentum becomes congested and oedematous and causes haemorrhagic extravasation of serosanguinous fluid into the peritoneal cavity [8]. Although cases of conservative treatment of primary torsion have been described in cases of partial volvulus, the treatment of complete torsion of the greater omentum with secondary necrosis is surgical [8]. Conservative management for omental torsion has been reported but carries the risk of abscess formation, which may result in prolongation of the abdominal pain and hospital stay [18, 23].
A laparoscopic approach should be considered because it is less invasive and associated with lower morbidity. Moreover, when preoperative diagnosis is not clear by imaging techniques, laparoscopy is useful for both diagnosis and treatment [24, 25]. The advantages of laparoscopy include the following: (i) complete examination of the abdominal cavity under visualization to confirm the diagnosis; (ii) facilitation of aspiration and washing of the peritoneum; and (iii) minimization of surgical invasiveness, postoperative pain, and complications related to the laparotomy wound [24].
Laparoscopy may not be possible in a few cases as in our first case due to bulk of omentum and jejunal adhesions to the infarcted omentum. Laparotomy may have to be resorted to. There are conflicting views in the surgical treatment of incarcerated hernias. Laparoscopic repair even for incarcerated and non-reducible groin hernias is advised by the European Association for Endoscopic Surgery [26]. However in omental torsion the bulk and weight of the torted omentum makes laparoscopic manoeuvring difficult. Delivering the resected omentum also requires a sizeble incision. This necessitated open inguinal hernia repair in our cases.
In both of our cases there was associated right inguinal hernia and maldescended right testis. In the first case, Meckel’s diverticulum was also present. Maldescended testis and Meckel’s diverticulum are perhaps only incidental findings. No association with omental torsion is reported in the literature. The prognosis for primary omental torsion is good with fast postoperative recovery and minimal morbidity [24].
Conclusion
Omental torsion can mimic various other causes of acute abdomen, which can be diagnosed preoperatively by USG and CT scan of the abdomen. It is not known to be associated with other congenital anomalies. Ours is the first reported case in literature with associated Meckel’s diverticulum. Symptomatic patients with preoperative diagnosis can be managed with omentectomy preferably by minimal access surgery.
Acknowledgements
The Department of Radiology & Imageology, Krishna Institute of Medical Sciences (KIMS), Secunderabad.
Conflicts of interest
The authors declare no conflicts of interest.
References
[1] Eitel GG. Rare omental torsion. N Y Med Rec. 1899; 55: 715–716.
[2] Montiel-Jarquin A, Lopez-Colombo A, Nava A, Juarez-Santiesteban R, Leyva-Trejo H, et al. Clinical characteristics of torsion of the omentum. Gastroenterol Res. 2009; 2(4):220–223.
[3] Adams JT. Torsion of the omentum. Abdominal wall, omentum, mesentery and retroperitoneum. In: Schwartz SI, Shires GT, Spencer FC, editors. Principles of surgery. 5th ed. New York, NY: McGraw-Hill, 1989: 1495–1496
[4] Jeganathan R, Epanomeritakis E, Diamond T. Primary torsion of the omentum. Ulster Med J. 2002; 71(1):76–77.
[5] Modaghegh MH, Jafarzadeh R. Primary omental torsion in an old woman: Imaging techniques can prevent unnecessary surgical interventions. Case Rep Med. 2011; 2011:541324.
[6] Theriot JA, Sayat J, Franco S, Buchino JJ. Childhood obesity: A risk factor for omental torsion. Pediatrics. 2003; 112(6 Pt 1):e460.
[7] Tamamoto F, Ishizaki H, Takanashi T, Shimoji K, Okamura T, et al. Omental torsion with right-sided inguinal hernia. Radiat Med. 2005; 23(8):566–569.
[8] Kim J, Kim Y, Cho OK, Rhim H, Koh BH, et al. Omental torsion: CT features. Abdom Imaging. 2004; 29:502–504.
[9] Xavier S, John P. Torsion of the greater omentum with inguinal hernia. Indian J Gastroenterol. 2003; 22(5):194–196.
[10] Morris JH. Torsion of the omentum: Its clinical importance. Arch Surg. 1932; 24(1):40–76.
[11] Albuz O, Ersoz N, Kilbas Z, Ozerhan IH, Harlak A, et al. Primary torsion of omentum: A rare cause of acute abdomen. Am J Emerg Med. 2010; 28(1):115.e5–7.
[12] al-Husaini H, Onime A, Oluwole SF. Primary torsion of the greater omentum. J Natl Med Assoc. 2000; 92(6):306–308.
[13] Al Tokhais TI, Bokhari AA, Noureldin OH. Primary omental torsion: A rare cause of acute abdomen. Saudi J Gastroenterol. 2007; 13(3):144–146.
[14] Hirano Y, Oyama K, Nozawa H, Hara T, Nakada K, et al. Left-sided omental torsion with inguinal hernia. World J Gastroenterol. 2006; 12(4):662–664.
[15] Mainzer RA, Simoes A. Primary idiopathic torsion of the omentum. Arch Surg. 1964; 88:974–981.
[16] Epstein LI, Lempke RE. Primary idiopathic segmental infarction of the greater omentum. Ann Surg. 1968; 167(3):437–443.
[17] Van Breda Vriesman AC, Puylaert JBCM. Epiploic appendagitis and omental infarction: pitfalls and look-alikes. Abdom Imaging. 2002; 27(1):20–28.
[18] Puylaert JB. Right-sided segmental infarction of the omentum: Clinical, US and CT findings. Radiology. 1992; 185(1):169–172.
[19] Maeda T, Mori H, Cyujo M, Kikuchi N, Hori Y, Takaki H. CT and MR findings of torsion of greater omentum: A case report. Abdom Imaging. 1997; 22(1):45–46.
[20] Yager A, Carmeci C. Torsion of the greater omentum: CT findings. AJR Am J Roentgenol. 1999; 173(4):1139–1140.
[21] Kudo A, Kawasaki T, Jibiki M, Hayashi S, Yabata E, et al. A case of idiopathic omental torsion with trans-epiploic hernia. Jpn J Gastrroenterol Surg. 2001; 34(12):1761–1764.
[22] Naffaa LN, Shabb NS, Haddad MC. CT findings of omental torsion and infarction: case report and review of the literature. Clin Imaging. 2003; 27(2):116–118.
[23] Paroz A, Halkic N, Pezzetta E, Martinet O. Idiopathic segmental infarction of the greater omentum: A rare cause of acute abdomen. J Gastrointest Surg. 2003; 7(6):805–808.
[24] Cianci R, Filippone A, Basilico R, Storto ML. Idiopathic segmental infarction of the greater omentum diagnosed by unenhanced multidetector-row CT and treated successfully by laparoscopy. Emerg Radiol; 2008, 15(1):51–56.
[25] Siddika A, Jamal-Hanjani M, Coker JB, Ullah MZ. Laparoscopy: A tool for the diagnosis and treatment of omental torsion. Int J Clin Pract. 2008, 62(11):1807–1808.
[26] Poelman MM, Van den Heuvel B, Deelder JD, Abis GS, Beudeker N, et al. EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg Endosc. 2013; 27(10):3505–3519.