Case Report
2017
September
Volume : 5
Issue : 3
Post-surgical giant pseudo meningocele in a patient with cervical neurofibroma: Case report and literature review
Raghavendra H, Varsha KS, Arun Reddy, Samsun Sujith, Kalyan Rao T, Sunanda G, Swarna latha
Pdf Page Numbers :- 98-101
Raghavendra H1,*, Varsha KS2, Arun Reddy1, Samsun Sujith1, Kalyan Rao T2, Sunanda G2 and Swarna latha3
1Department of Neurosurgery, ESIC Medical College and Super Speciality Hospital, Hyderabad-500038, Telangana, India
2Department of Anaesthesiology, ESIC Medical College and Super Speciality Hospital, Hyderabad-500038, Telangana, India
3Department of Radiology, ESIC Medical College and Super Speciality Hospital, Hyderabad-500038, Telangana, India
*Corresponding author: Dr. Raghavendra H, Department of Neurosurgery, ESIC Medical College and Super Speciality Hospital, Hyderabad-500038, Telangana, India. Email: harpanahalli.raghavendra@gmail.com
Received 8 April 2017; Revised 16 May 2017; Accepted 26 June 2017; Published 30 June 2017
Citation: Raghavendra H, Varsha KS, Reddy A, Sujith S, Rao KT, Sunanda G, latha S. Post-surgical giant pseudo meningocele in a patient with cervical neurofibroma: Case report and literature review. J Med Sci Res. 2017; 5(3):98-101. DOI: http://dx.doi.org/10.17727/JMSR.2017/5-18
Copyright: © 2017 Raghavendra H et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
A patient aged 48-year-old, presented to the outpatient department with neck pain and weakness of all the limbs for three months. On examination, he had power 3/5 in all the limbs with bilateral hand grip weakness of 50%. Neuroimaging study showed a dumbell shaped lesion with compression of the spinal cord in the cervical region that was identified as a C4/C5 neurofibroma. Cervical laminectomy and excision of the tumour and unilateral lateral mass screw and rod fixation was done. Post operatively patient was discharged with improved motor power. One month after surgery, he presented with bulging at the operative site, which was diagnosed as a pseudo meningocele that did not respond to conservative therapy. As swelling was increasing size and becoming tense and also complaining of severe neck pain and postural hypotension, it was managed surgically, three months after first surgery, by excision of pseudo meningocele with primary repair of dural defect with muscle graft and lumbar drain inserted intraoperatively which was removed after five days. Patient’s neck pain and hypotensive episode were improved after repair. Possible causes for the development of post-operative pseudo meningocele can be soft tissue and paravertebral muscle damage or high intradural pressures that causes leakage of cerebrospinal fluid from a very small dural defect. Shunt insertion should be reserved for patients with impaired cerebrospinal fluid absorption or those with a refractory fistula, despite medical therapies and direct surgical repairs.
Keywords: post-surgical; pseudo meningocele; cervical neurofibroma
Full Text
Introduction
Pseudo meningocele is an extradural collection of cerebrospinal fluid (CSF) in an arachnoid-lined capsule that can occur following dural tearing or inadequate closure during spinal surgery [1]. There are 3 types of extradural pseudo meningocele: congenital, iatrogenic and traumatic. However, postsurgical pseudo meningoceles are uncommon complications after spinal surgery [2]. The lesion size depends on the size of the defect in the dura-arachnoid, the pressure of spinal fluid and the resistance from the surrounding soft tissues of the pseudocyst. Pseudo meningocele can appear with symptoms such as wound swelling, headache, and focal neurological defects [3]. In a small dural tear the intradural pressure causes a constant extravasation of spinal fluid, that can lead to a gradual enlargement of the lesion and eventually formation of a giant pseudocyst compressing the spinal cord, causing several neurological defects. The management and approach of this pseudocyst depends on the size, symptoms of the patient and the period between surgery and appearance of this pseudocyst. This article is a case report with review of the literature concerning diagnostic methods and management of pseudo meningocele and their follow up.
Case presentation
The patient was a 48-year-old gentleman with neck pain and weakness of all the limbs for a duration of three months. on examination, he had power 3/5 in all the limbs with bilateral hand grip weakness-50%. Neuroimaging study showed a dumbell shaped lesion with compression of the spinal cord in the cervical region that was identified as C4/C5 neurofibroma. Cervical laminectomy and excision of tumour and unilateral lateral mass screw and rod fixation was done. Post operatively patient was discharged with improved motor power. One month after surgery, he presented with bulging at the operative site, which was diagnosed as a pseudo meningocele that did not respond to conservative therapy. The swelling was increasing in size and becoming tense and patient was complaining of severe neck pain and postural hypotension (Figure 1). MRI cervical spine was repeated which shows giant pseudo meningocele sac with intradural extension (Figure 2). Hence it was managed surgically, after three months of first surgery by excision of pseudo meningocele with primary repair of dural defect (Figure 3) with muscle graft and lumbar drain inserted intraoperatively which was removed after five days. Patients neck pain and hypotensive episode were improved after repair.

Figure 1: Giant pseudomeningocele with impending rupture.
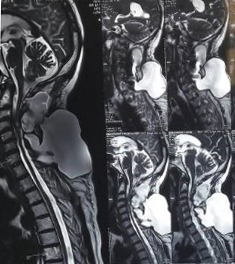
Figure 2: Giant pseudomeningocele with intradural extension.
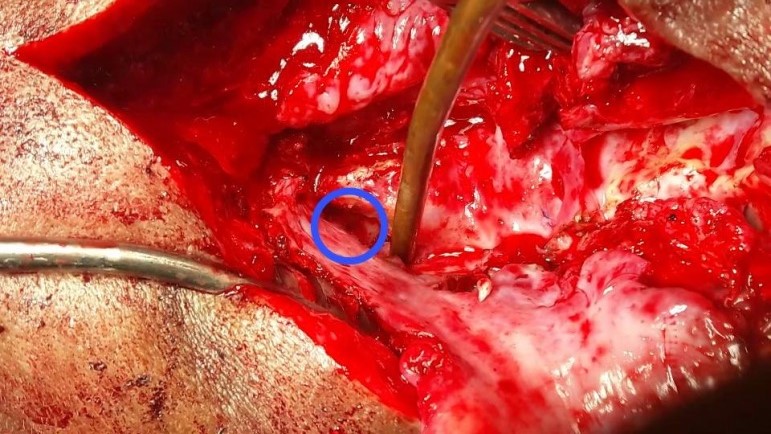
Figure 3: Intra operative dural defect.
Discussion
The formation of pseudo meningocele can be due to congenital, iatrogenic or traumatic causes [4]. Congenital pseudo meningoceles often are associated with neurofibromatosis and Marfan syndrome and mostly occur in the thoracic or thoracolumbar region [5]. The traumatic pseudo meningoceles are often in the cervical area [2] in which, the iatrogenic pseudo meningoceles are the most common ones. The incidence of formation of this pseudocysts are often during spinal or intradural surgery [4]. The post-operative pseudocysts are mostly seen after lumbar spinal surgery [6]. The intradural pressure is higher in the lumbar spine than in the cervical spine; this potentially explains why pseudo meningoceles occurs more often at the lumbar level. A giant pseudo meningocele can develop in patients with a large dural defect or high intradural pressure. A giant pseudo meningocele is defined as a lesion ≥8 cm in diameter. The reports of such pseudocysts are rare and they are not well known [7]. There is a variety in symptoms of patients with pseudo meningocele from asymptomatic to common symptoms such as postural headache, localized back pain and radiculopathy. The patient with giant pseudo meningocele is mostly symptomatic and the most common symptom is headache [2]. The incidence of pseudo meningocele has been reported to be about 0.068 % to 2% after laminectomy [8]. Injury of the dura at the time of surgery can lead to pseudo meningocele. If the patient had complications after surgery, this diagnose should be considered and evaluated. In the article from Rinaldi (1970) myelography is the initially recommended method to establish the diagnosis of pseudomeningocele [9]. CT and MRI are recommended as the choice of diagnostic modality [10] and MRI showed to be the most effective method [2]. There are some controversies in the treatment of pseudocysts, especially in asymptomatic patients. The method of approach mostly depends on the pseudocysts size, location and symptoms of patient [8]. Conservative management is preferred in asymptomatic patients or in patient with early symptomatic and in CSF fistula the treatment should contain a spinal drainage and in patients with late symptoms (after weeks or months) surgery should be considered. Mostly, pseudo meningoceles are surgically explored and gradually been dissected from the circumambient tissue and nerve roots and the fistulous tracts should be excised and the dural tear should be repaired and a subarachnoid catheter is implanted for drainage [2]. For giant pseudocysts, a combined treatment protocol is advised that contains surgery for extirpation of pseudo meningoceles, repair of the dural tears, and implant of a subarachnoid catheter for drainage [2].
Conclusion
Possible causes for the development of post-operative pseudo meningocele can be damage of soft tissues and paravertebral muscles or high intradural pressures that lead to leakage of cerebrospinal fluid from a very small dural defect. Shunt insertion should be reserved for patients with impaired CSF absorption or those with a refractory fistula, despite medical therapies and direct surgical repairs.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Phillips CD, Kaptain GJ, Razack N. Depiction of a postoperative pseudomeningocele with digital subtraction myelography. Am J Neuroradiol. 2002; 23(2):337–338.
[2] Weng YJ, Cheng CC, Li YY, Huang TJ, Hsu RW. Management of giant pseudomeningoceles after spinal surgery. BMC Musculoskelet Disord. 2010; 21:11–53.
[3] Kotani Y, Abumi K, Ito M, Terae S, Hisada Y, et al. Neurological recovery after surgical treatment of giant cervical pseudomeningoceles extending to lumbar spine associated with previous brachial plexus injury. Eur Spine J. 2010; 19 (Suppl 2):S206–S210
[4] Couture D, Branch CL Jr. Spinal pseudo meningoceles and cerebrospinal fluid fistulas. Neurosurg Focus. 2003; 15(6):E6.
[5] Sutterlin CE, Grogan DP, Ogden JA. Diagnosis of developmental pathology of the neuraxis by magnetic resonance imaging. J Pediatr Orthop. 1987; 7(3):291–297.
[6] Lee KS, Hardy IM. Post laminectomy lumbar pseudo meningocele: Report of four cases. Neurosurgery. 1992; 30(1):111–114.
[7] Hader WJ, Fairholm D. Giant intraspinalpseudo meningoceles cause delayed neurological dysfunction after brachial plexus injury: report of three cases. Neurosurgery. 2000; 46(5):1245–1249.
[8] Nairus JG, Richman JD, Douglas RA. Retroperitoneal pseudo meningocele complicated by meningitis following a lumbar burst fracture. Spine (Phila Pa 1976). 1996; 21(9):1090–1093.
[9] Rinaldi I, Hodges TO. Iatrogenic lumbar meningocele: Report of three cases. J Neurol Neurosurg Psychiatry. 1970; 33(4):484–492.
[10] Murayama S, Numaguchi Y, Whitecloud TS, Brent CR. Magnetic resonance imaging of post-surgical pseudo meningocele. Comput Med Imaging Graph. 1989; 13(4):335–339.