Full Text
Introduction
Most common malignant tumors involving the vertebral column are metastatic. Primary malignant tumors involving the axial skeleton are rare. The primary function of spine is anatomical, and is involved in the erect posture of human beings. The physiological function is primarily hemopoietic. The segments of the spine include cervical with seven vertebrae, dorsal with twelve vertebrae, lumbar with five vertebrae, sacral with fused five vertebrae and coccygeal with fused four vertebrae.
Imaging methods of spine include conventional, CT, MRI, Radio nuclide, PET CT and Angiography. Conventional radiology most often reveals the nature of the lesion. However, when the lesions are multiple routine skeletal survey may not be adequate. MRI Radionuclide scintigraphy and PET CT scan are more sensitive and may pickup multiple lesions.
Myeloma, a common malignant tumor in old age manifests as 1) Solitary – plasmacytoma, 2) Multiple myeloma, and 3) Poems syndrome
Plasmacytoma
It is a solitary lesion and can be encountered in any bone. However, it is common in the spine. Most of the benign looking plasmacytomas when followed may develop into multiple myeloma eventually. Radiologically, a plasmacytoma is an expanding lytic lesion without any calcification or new bone formation. When it involves the vertebral body a compression fracture may be seen. When marked compression is seen vertebral plana is noted (Figure 1abc). To differentiate from metastasis, it is stated that in metastasis pedicles are involved earlier as they are vascular (2ab). However, when a large part of the body is involved in myeloma, pedicles also may be destroyed (Figure 3abc).
CT and MRI demonstrate lytic areas with struts of bone interspersed. In MRI, plasmacytoma shows a classical minibrain appearance (Figure 4abc). At times, it is difficult to differentiate hemangioma from plasmacytoma (Figure 5ab). It may remain localized for many years but more than 30% progress quite rapidly to generalized myelomatosis with a latent interval of 5-10 years. Radiological features are listed in table 1.
Table 1: Radiological features of plasmacytomas.
|
· It is typically lytic and destructive. Sclerosis is rare.
· Bone expansion, which may be considerable with thinning of the overlying cortex, is common.
· The margins are usually well defined and sharply demarcated and an associated soft tissue mass is frequently seen.
· Large lesions in flat bones may assume a soap –bubble appearance.
· “Solitary osteolytic lesion in a vertebral body in a patient in late middle age should always be considered as a Plasmacytoma”.
· Following the diagnosis of plasmacytoma, MRI of the spine and pelvis is indicated to identify additional lesions, to rule out multiple myeloma, which may be seen in up to 80% of cases.
· Occult lesions may also be demonstrated by [F-18] FDG-PET.
|
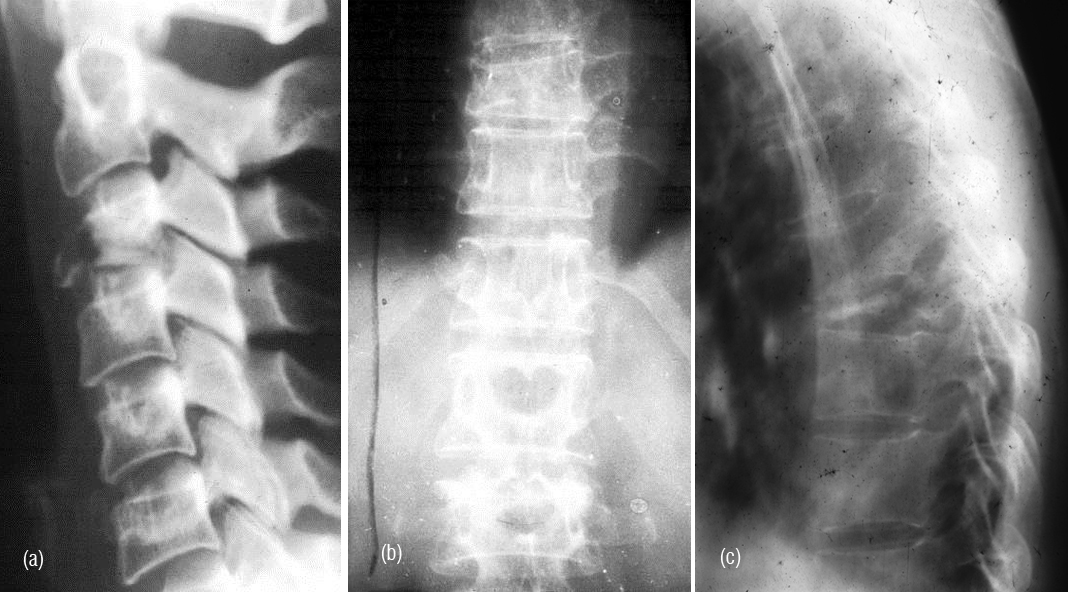
Figure 1a,b: Plasmacytoma with collapse of C3, T10. (c) Plasmacytoma – vertebra plana T8.
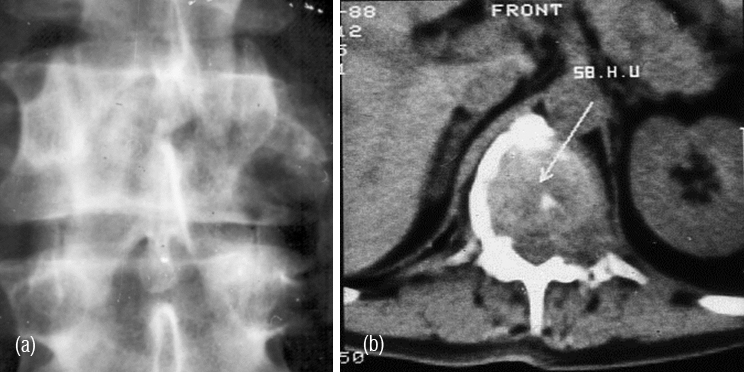
Figure 2: (a) Plasmacytoma of L2, (b) CT guided biopsy.
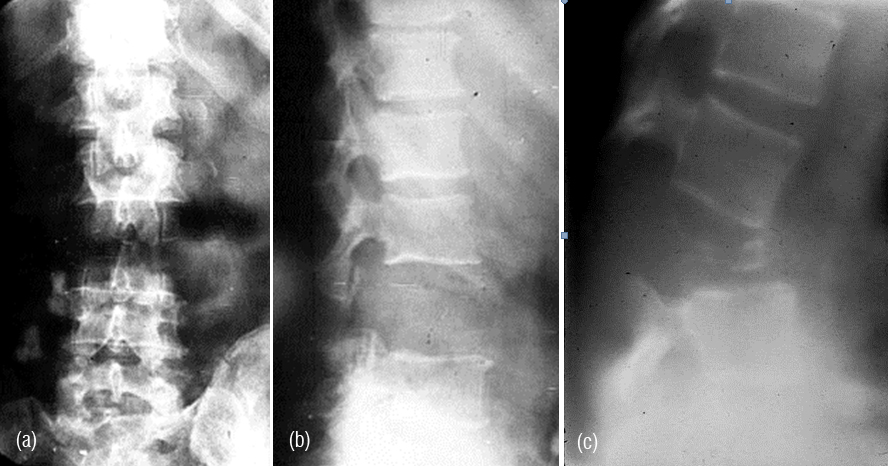
Figure 3abc: Plasmacytoma - Complete destruction of body of L3 including the posterior elements.
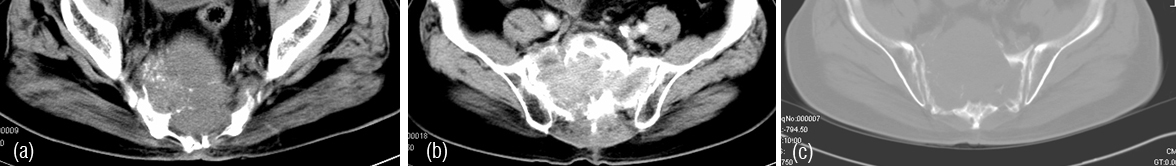
Figure 4a,b,c: CT - Plasmacytoma of sacrum, an expanding lytic lesion.
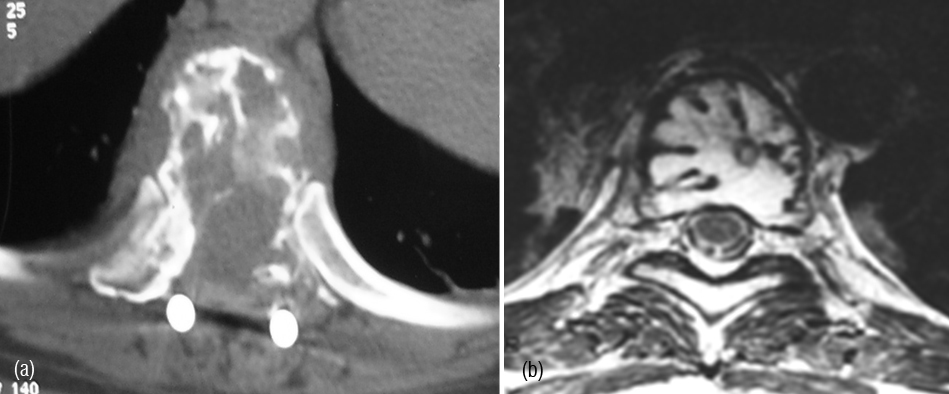
Figure 5: (a) CT (post op.), (b) MRI – Minibrain appearance
Multiple myeloma (MM)
MM is a clonal B-lymphocyte neoplasm of terminally differentiated plasma cells and it is most common primary malignant tumor of bone. The median age at diagnosis is 55 years. Higher incidence is noted in men. Clinical symptoms include fatigue, generalized bone pains with or without associated fracture. The types of multiple myeloma are listed in table 2.
Table 2: Four distinct forms of involvement have been described.
|
· Diffuse skeletal involvement (myelomatosis),
· Diffuse skeletal osteopenia
· Sclerosing myeloma
· Plasmacytoma, distribution of malignant plasma cells in MM includes sites that show normal areas of active hematopoiesis in adults, lesions are osteolytic with discrete margins and uniform size, common sites are vertebrae, pelvis, skull, ribs, sternum and proximal appendages.
|
It radiologically shows a spectrum of manifestations. The bones particularly, in axial skeleton may present with multiple compression fractures. In 10-15% of cases, classical punched out lesions of the skull may be noted. In long tubular bones, pathological fractures are common with associated soft tissue swelling. In early skeletal lesions, moth eaten type of appearance is observed without any periosteal reaction (Figure 6ab). MRI is more sensitive to depict bone marrow lesions, whereas radionuclide scintigraphy with technetium 99 compounds is not that sensitive (Figure 7abcdef). The radiological appearances are listed in Table 3.
Table 3: Multiple Myeloma Radiological Spectrum
|
· Normal
· Osteopenia
· Compression #s of spine
· Moth eaten
· Punched out lesions
· Geographic areas of lysis
· Sclerotic lesions (Poems)
· Soft tissue masses
· Plasmacytoma
|
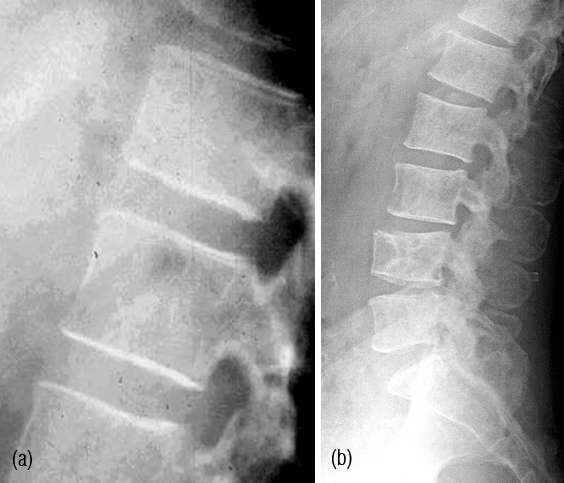
Figure 6: Multiple Myeloma – (a) Diffuse osteopenia with loss of trabeculae, (b) lytic lesions in the bodies.
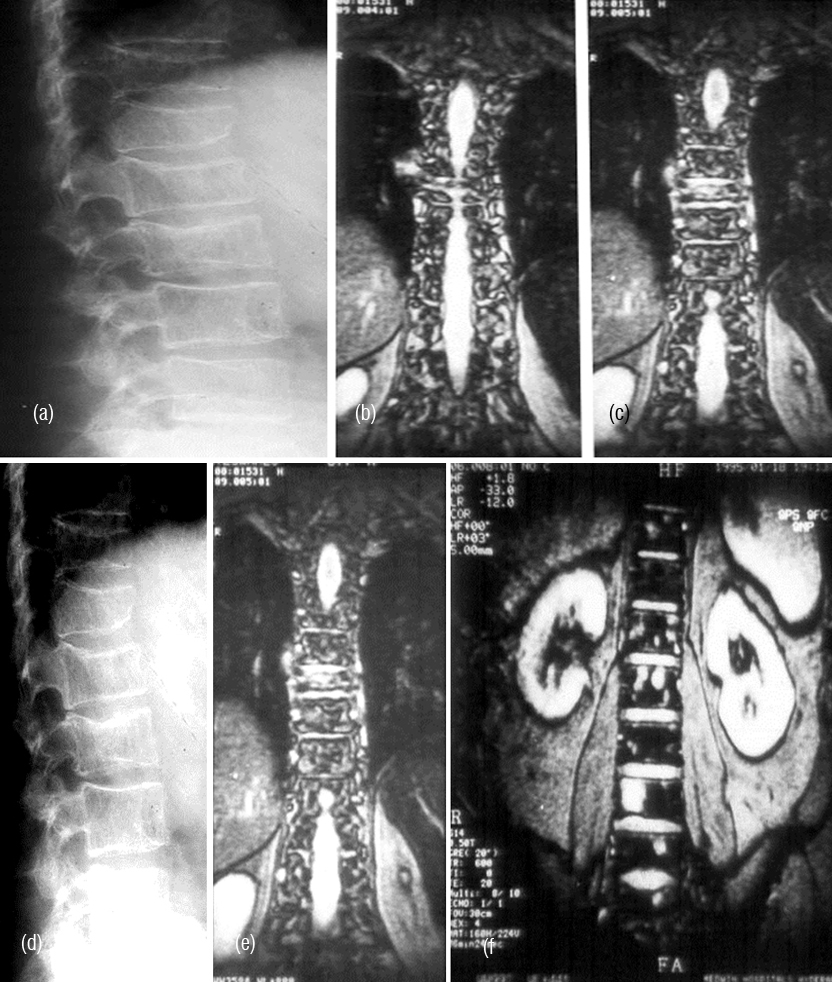
Figure 7: (a,b,c) Multiple myeloma with osteopenia and early collapse of vertebral bodies BC MRI of the same patient. (d) plain films, (e, f) MRI.
Poems syndrome
P stands for polyneuropathy, O stands for organomegaly, E stands for endcrinal changes, M stands for M protein and S stands for sclerotic changes in the bone. All of these may not be present all the time.
Radiologically, Sclerotic changes in the bone may be unifocal or multifocal. At times, lytic lesions may be also noted (Figure 8ab).
In the differential diagnosis particularly in older people metastasis must be considered. Table 4 shows the radiological differentiation between myeloma and metastases. Differential diagnostic features are listed in table 4.
Table 4: Myeloma Vs Metastases.
|
|
Myeloma
|
Metastasis
|
|
Vertebral pedicle involvement
|
Late
|
Early
|
|
Soft tissue
|
Masses ++
|
Mass only with fracture
|
|
Mandible involvement
|
Involved
|
Late
|
|
Mixed lesions
|
Unusual
|
Not unusual
|
|
IV disc involvement
|
Involved
|
Rare
|
|
Facial bones involvement
|
Involved
|
Rare
|

Figure 8: (a) Sclerotic myeloma – diffuse sclerosis of all the lumbar vertebrae. (b) Sclerotic lesion in the femur in Poems syndrome.
Chondrosarcoma
This is also a rare tumor and may involve the vertebral column. Radiological findings include lytic lesion with sclerosis and cartilaginous calcifications (Figure 9abcd). CT helps in identification of early calcifications. CT allows optimal detection and characterization of matrix mineralization, endosteal scalloping. MR imaging depicts the extent of marrow involvement and demonstration of soft tissue extension with mass formation. MRI shows the cartilaginous nature of the lesion by bright signals in T2 (Figure 10abcd).
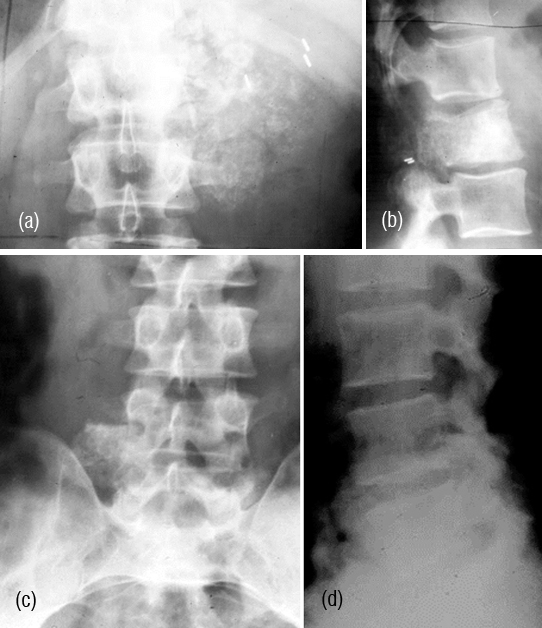
Figure 9a,b: Chondrosarcoma of L1. Note the paravertebral ring like calcifications.
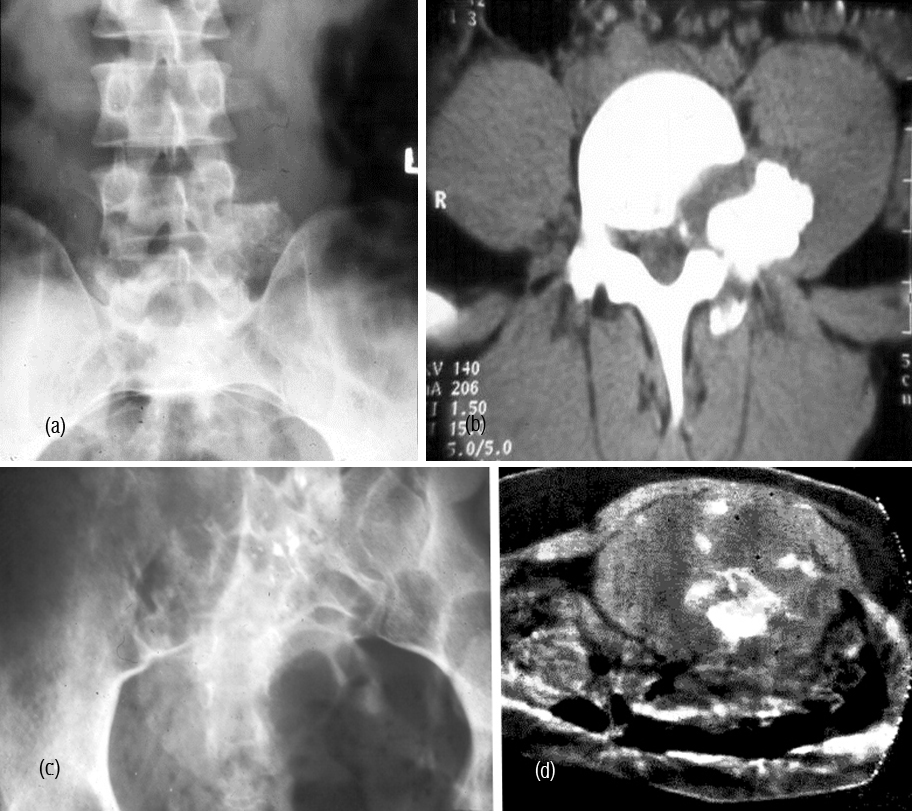
Figure 9: Chondrosarcoma of L5- (c) AP view, (d) Lateral view.
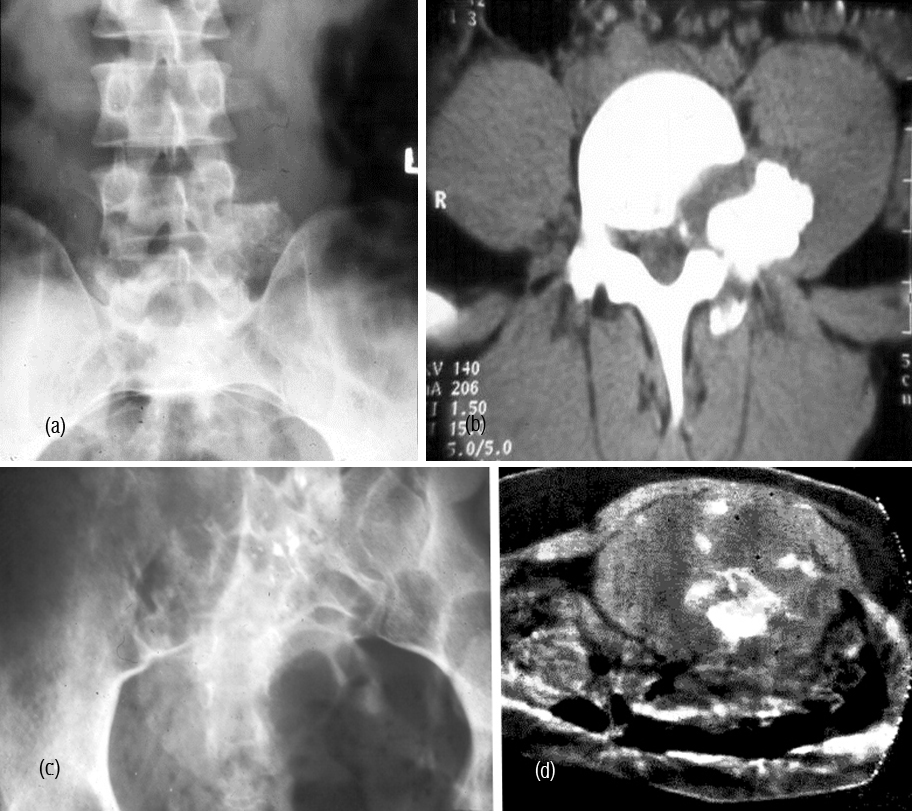
Figure 10: Chondrosarcoma L5 – (a) plain films, (b) CT helps in identification of small calcifications. (c) plain, (d) MRI.
Ewing’s sarcoma
It constitutes 10% of all primaries. The incidence of M:F :: 2:1. It is not common in the vertebral column. 75% of the lesions occur in pelvic girdle and long bones. Chromosomal abnormality is translocation of (t11;22). Biopsy is the final confirmation for diagnosis.
Radiological findings include permiative lytic lesion with a large soft tissue mass, on occasion diffuse sclerosis is noted simulating an ivory vertebra (Figure 11ab)
“The gross anatomy (as revealed in radiographs) is often a safer guide to a correct clinical conception of the disease than the variable and uncertain structure of a small piece of tissue”- Ewing - 1922
The differential diagnosis of Ivory vertebra seen on plain films is listed in table 5.
Table 5: Differential diagnosis of ivory vertebra
|
· Ewing’s sarcoma
· Metastasis - Solitary
· Lymphoma
· Paget’s disease
· Osteosarcoma
· Chronic osteomyelitis
· Melorheostosis
· Chordoma (rare)
· Myeloma (rare)
· Osteoblastoma
|
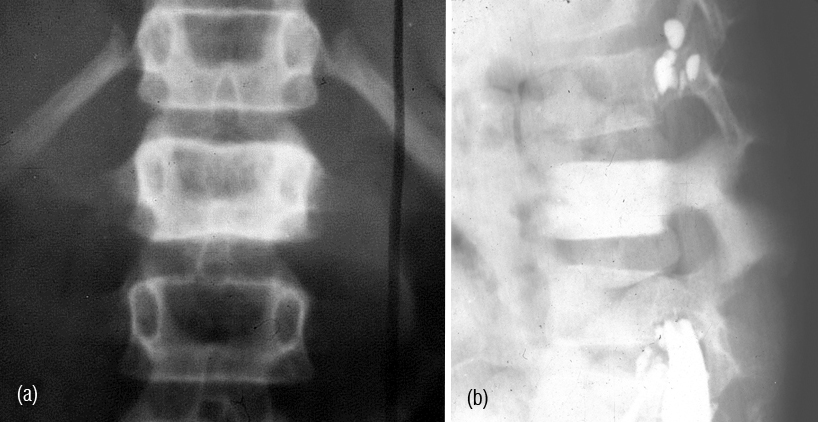
Figure 11a,b: Ewing’s sarcoma – Ivory vertebra of L1.
Primary osteosarcoma
This is another rare tumor that involves the vertebral column. Several instances have been reported involving single vertebral body of spine more commonly sacrum. Radiologically, both lytic and sclerotic changes are noted with new tumor bone formation. When it occurs in the sacrum it may simulate an ivory body (Figure 12). When sclerotic metastasis occur in a solitary vertebra it is difficult to differentiate from primary osteosarcoma.

Figure 12: Primary osteosarcoma involving the sacrum.
Primary lymphoma
Primary lyphoma of bone is uncommon. However, when the bone is involved, radiological findings include both lytic and sclerotic changes with soft tissue swelling. In Hodgkin’s type of lymphoma sclerotic lesions predominate. Occasionally, only pedicles of the spine may be involved (Figure13abc).
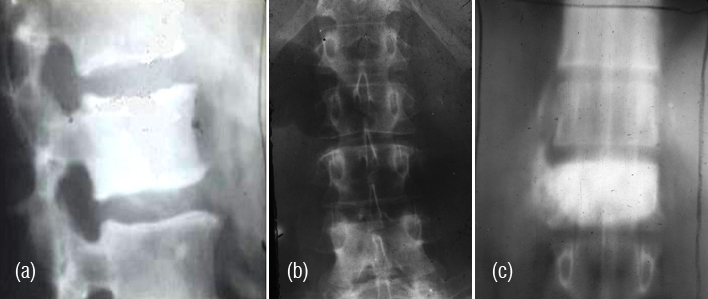
Figure 13: (a) Lymphoma (Ivory vertebra) involving the body of L1. (b) Hodgkin’s lymphoma. Note the ivory pedicles. (c) Hodgkin’s lymphoma – conventional tomogram.
Primary osseous malignant fibrous histiocytoma (MFH). Formerly used to be called fibrosarcoma which does not form osteoid or chondroid matrix, it is rare in the vertebral column.
Radiologically, most primary osseous MFHs are purely osteolytic and range in aggressiveness from geographic, with a variable width in the zone of transition, to permeative patterns. Internal calcification, bone formation, periosteal reaction and sequestra within osseous lesions are uncommon findings (Figure 14ab). Histiologically, storiform type of spindle cells are noted.
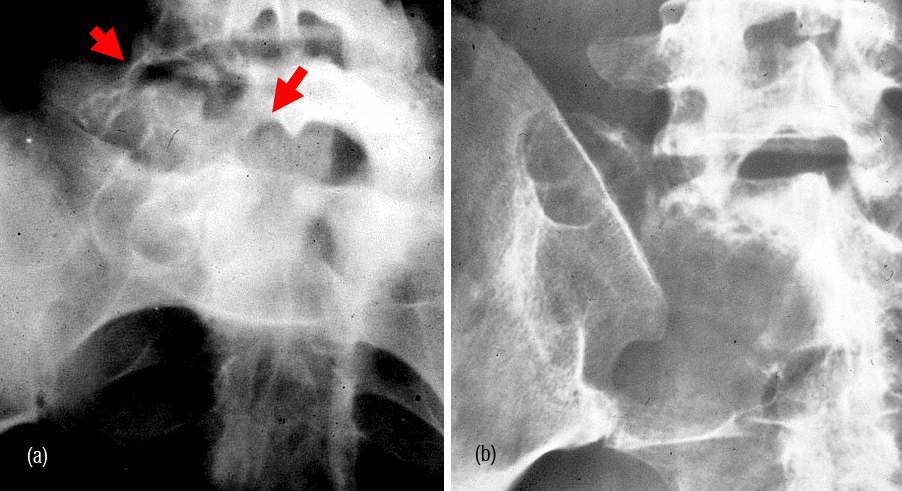
Figure 14: (a) Malignant Fibrous Histiocytoma involving L5 and sacrum on right side. (b) Malignant Fibrous Histiocytoma of the sacrum involving right iliac bone.
Chordoma
This locally malignant lesion occurs in the vertebral column in 90% of the cases, 55% in sacrum and 25% in clivus and rest of the spine 20%. It is common in the cervical spine as compared to the rest of the spine. The age group is between 45 & 70, but no age is exempt.
Radiologically, majority of the cases show extensive osteolysis of the sacrum with few areas of osteoblastic reaction. A large soft tissue mass is noted with few calcifications. The calcifications of chondroid nature are common in chondroid type of chordoma and are extensive (Figure 15abcde). In the differential diagnosis, plasmacytoma, metastasis and chondrosarcoma may be considered. Aggressive benign lesions such as aneurysmal bone cyst, myxopapillary ependymoma and aggressive giant cell tumor may also be under consideration particularly when it occurs in the sacrum. In the cervical spine TB of the spine comes under differential diagnosis. Histiologically, the physalipherus cell is characteristic (Figure 15f).
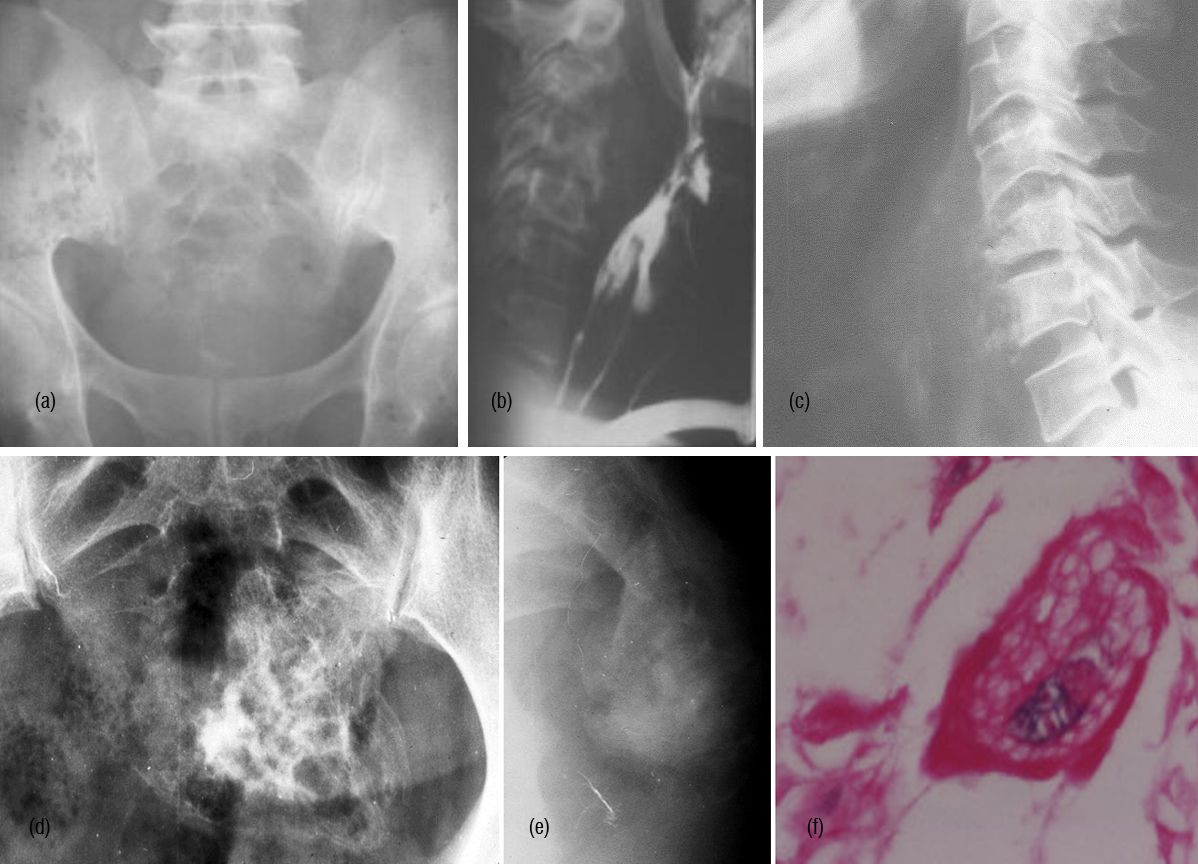
Figure 15: (a) Chordoma of sacrum, (b) Chordoma C. Spine with soft tissue swelling compressing the pharynx , (c) Chordoma C. Spine (d) Chondroid chordoma – AP, (e) lateral of sacrum. (f) Chordoma – Physalipherus cell.
Myxopapillary ependymoma
It is a rare tumor involving the sacrum. Radiologically, it is a lytic lesion which is lobulated and is difficult to make a diagnosis (Figure 16). CT and MRI may help in tissue differentiation. Histology is the only way to make a diagnosis (Figure 17abcd). An admixture of fibrillated & epitheloid cells with myxoid connective tissue stroma and fusiform cells in palisading arrangement mixed with mucin deposition are noted. Glial fibrillary acidic protein (GFAP), S-100 protein is positive.

Figure 16: Myxopapillary ependymoma of the sacrum – Note lytic and sclerotic changes of non – specific nature.
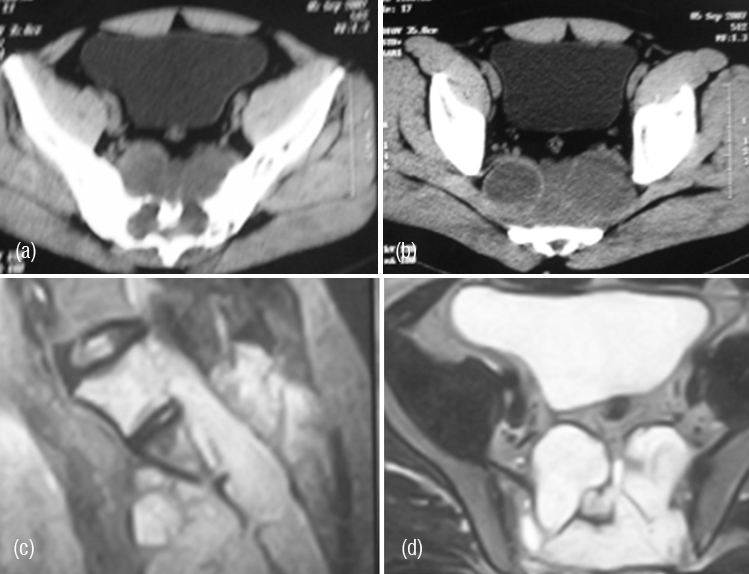
Figure 17: (a,b) CT – Myxopapillary ependymoma of sacrum. Lytic and sclerotic changes with cyst like soft tissue masses. (c,d) MRI – Myxopapillary ependymoma of sacrum. Cyst like soft tissue masses in a lytic sacrum.
Conclusion
Primary malignant tumours of the vertebral column are rare. Whenever, an isolated vertebral lesion is noted radiographically a systemic examination for other lesions should be done, preferably radionuclide scintigraphy. Most of the time, plain films would help. However, small lesions may be missed. Hence, CT scan and MRI should be used to identify the small lesions and early calcifications. Radionuclide scintigraphy would help in identifying multiple lesions, but this may not be helpful in multiple myeloma and other bone marrow lesions. Finally biopsy should be done under the imaging guidance for confirmation of the diagnosis.
Conflict of interest
The author wish to express that he has no conflict of interest.
References
1. Beltran J, Noto AM, Chakeres DW, Christoforidis AJ. Tumors of the osseous spine: staging with MR imaging versus CT. Radiology 1987;162(2):565-569.
2. Boyko OB, Cory DA, Cohen MD, Provisor A, Mirkin D. MR imaging of osteogenic and Ewing's sarcoma. AJR Am J Roentgenol. 1987; 148(2):317-322.
3. de Bruïne FT, Kroon HM. Spinal chordoma: radiologic features in 14 cases. AJR Am J Roentgenol. 1988; 150(4):861-873.
4. Edeiken-Monroe B, Edeiken J, Kim EE. Radiologic con¬cepts of lymphoma of bone. Radiol Clin North Am. 1990; 28:841-864.
5. Firooznia H, Golimbu C, Rafii M, Reede DL, Kricheff II, et al. Computed to¬mography of spinal chordomas. J Comput Tomogr. 1986; 10:45-50.
6. Fruehwald FX1, Tscholakoff D, Schwaighofer B, Wicke L, Neuhold A, et al. Magnetic resonance imaging of the lower vertebral column in patients with multiple myeloma. Invest Radiol. 1988; 23(3):193-199.
7. Kornberg M. Primary Ewing's sarcoma of the spine: a review and case report. Spine 1986;11(1):54-57.
8. Mayes CB, Wallace S, Bernardino ME. Computed to¬mography of chondrosarcoma. Journal of Computed Tomography 1981; 5:345-348.
9. Mulligan ME, McRae GA, Murphey MD. Imaging features of primary lymphoma of bone. AJR Am j Roentgenol. 1999; 173 (6): 1691-1697
10. Oot RF, Melville GE, New PF, Austin-Seymour M, Munzenrider J, et al. The role of MR and CT in evaluating clival chordomas and chondrosarcomas. AJR Am J Roentgenol. 1988; 151(3):567-575.
11. Resnick D, Greenway GD, Bardwick PA, Zvaifler NJ, Gill GN, et al. Plasma-cell dyscrasia with polyneuropathy, organomegaly, endocrinopathy, M-protein, and skin changes: the POEMS syndrome. Distinctive radiographic abnormalities. Radiology 1981:140:17-22.
12. Schreiman JS, McLeod RA, Kyle RA, Beabout JW. Mul¬tiple myeloma: evaluation by CT. Radiology 1985:154:483-486.
13. Shives TC, Dahlin DC, Sim FH, Pritchard DJ, Earle JD. Osteosarcoma of the spine. J Bone Joint Surg Am. 1986; 68(5):660-668.
14. Smith J, Ludwig RL, Marcove RC. Sacrococcygeal chor¬doma: a clinicoradiological study of 60 patients. Skel¬etal RadioI. 1987; 16:37-44.
15. Solomon A, Rahamani R, Seligsohn U, Ben-Artzi F. Multiple myeloma: early vertebral involvement assessed by computerised tomography. Skeletal Radiol. 1984; 11(4):258-261.
16. Sze G, Uichanco LS, Brant-Zawadzki MN, Davis RL, Gutin PH, et al. Chor¬domas: MR imaging. Radiology 1988; 166:187-191.
17. Vanel D, Contesso G, Couanet D, Piekarski JD, Sarrazin D, et al. Computed tomography in the evaluation of 41 cases of Ewing's sarcoma. Skeletal Radiol. 1982; 9(1):8-13.