Case Report
2022
September
Volume : 10
Issue : 3
Pyogenic granuloma of eyelid: A literature review and case report
Dasari G, Rao VVLN, Satyanarayana KVV, Vedula B
Pdf Page Numbers :- 169-171
Gayatri Dasari1,*, Narasimha Rao VVL1, Satyanarayana KVV1 and Bharadwaj Vedula2
1Department of Ophthalmology, Gitam Institute of Medical Sciences and Research, Rushikonda, Visakhapatnam, Andhra Pradesh 530045, India
2Department of Pathology, Gitam Institute of Medical Sciences and Research, Rushikonda, Visakhapatnam, Andhra Pradesh 530045, India
*Corresponding author: Dr. Dasari Gayatri, Senior Resident, Department of Ophthalmology, Gitam Institute of Medical Sciences and Research, Rushikonda, Visakhapatnam, Andhra Pradesh 530045, India. Email: perigayatri@gmail.com
Received 30 March 2022; Revised 24 May 2022; Accepted 1 June 2022; Published 10 June 2022
Citation: Dasari G, Rao VVLN, Satyanarayana KVV, Vedula B. Pyogenic granuloma of eyelid: A literature review and case report. J Med Sci Res. 2022; 10(3):169-171. DOI: http://dx.doi.org/10.17727/JMSR.2022/10-31
Copyright: © 2022 Dasari G et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Pyogenic granuloma is an acquired vascular proliferative lesion with associated inflammation, affecting the skin and mucous membranes more frequently. Ocular pyogenic granulomas are rare, involving adnexa, conjunctiva, and cornea. Eyelid pyogenic granuloma is uncommon, associated with chalazion, lid surgeries, lacrimal sac procedures, trauma, predisposing cutaneous lesions, congenital capillary malformations, and idiopathic. We report a case of a 40-year-old male patient who attended our outpatient department with right eye upper lid painless growth, gradually increasing in size in the last two months. The differential diagnosis was burst chalazion, capillary haemangioma, molluscum contagiosum, pilomatricoma, basal cell carcinoma, squamous cell carcinoma, and Kaposi's sarcoma. The lesion was surgically excised, and histopathological examination confirmed the diagnosis. There was no recurrence. This present case illustrates the importance of considering benign inflammatory causes in the differential diagnosis of eyelid mass lesions to avoid unnecessarily aggressive intervention.
Keywords: eyelid; pyogenic granuloma; pathology; haemangioma; vascular proliferation
Full Text
Introduction
Pyogenic granuloma (lobular capillary haemangioma) [1] is an acquired ulcerative vascular proliferation, commonly involving skin and mucous membranes [2]. The male: female ratio is 1.5:13. Ocular pyogenic granulomas are rare. Usually, eyelids, conjunctiva, and cornea are involved. Pathogenesis is unclear, assumed to be due to vasoproliferative inflammatory response with granulation tissue. Some researchers proposed an imbalance in angiogenesis regulation [3].
Causes of adnexal pyogenic granuloma are trauma, previous surgeries (entropion repair, dacryocystorhinostomy with stent tube or jones tube, tarsorrhaphy), chalazion, punctal plug insertion, and idiopathic [4-7]. Causes of conjunctival pyogenic granuloma are trauma, infection, surgeries (pterygium excision, strabismus surgery, scleral buckle), post-Ahmed valve implantation, and scleral prosthesis [8-13]. Causes of pyogenic corneal granuloma are previous corneal surgeries [6], trauma, and infectious keratitis [14-16].
Case report
A 42-year-old male patient visited our Outpatient Department of Ophthalmology in Gitam Institute of Medical Sciences and Research on the 14th of July 2021 with right eye upper lid painless growth, gradually increasing in size for the last two months. No history of trauma or any predisposing dermatologic lesion or surgery. On examination, a purple-red well circumscribed polypoid lobular lesion with ulcerated skin, 15mm × 9mm in size, present on the right upper lid, 2 mm above the lid margin, and 10 mm from the medial canthus, non-tender and firm in consistency on palpation, was present (Figure 1). There was no regional lymph node involvement. The fellow eye was normal. Both eyes' uncorrected distance visual acuity was 20/20, and near vision was N6 with the addition of a +1.00 dioptre lens. Differential diagnoses were capillary haemangioma, molluscum contagiosum, ruptured chalazion granuloma, pilomatricoma, basal cell carcinoma, and squamous cell carcinoma. Informed consent was taken.

Figure 1: Pre-operative picture.
A complete excision biopsy of the mass performed with a margin of 4mm, and the skin defect was closed with interrupted sutures (Figure 2). A histopathological examination conducted on the excised mass.
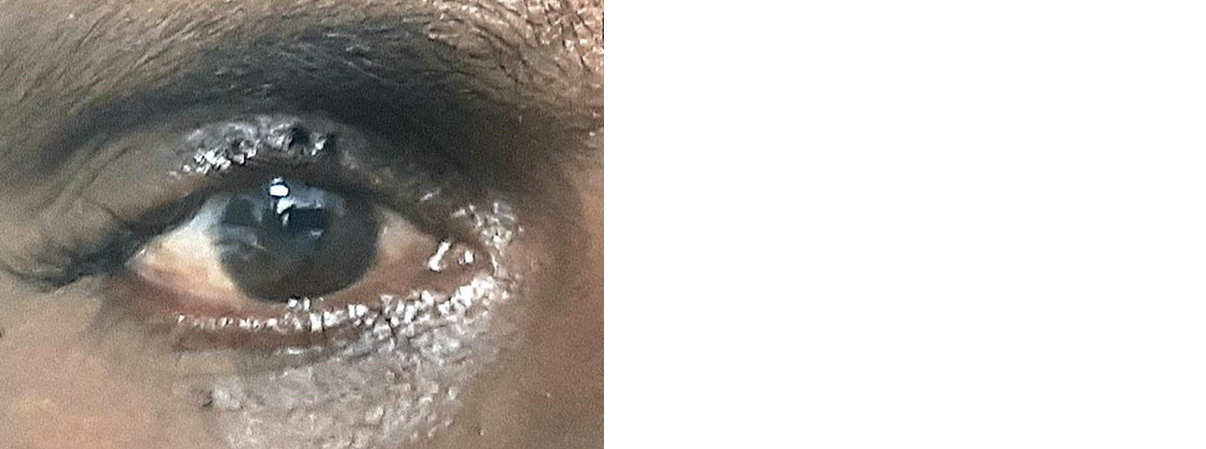
Figure 2: Post-operative picture.
Histopathology report revealed ulcerated epithelium with bacterial colonies, lobules containing multiple endothelial lined vascular channels (proliferating capillary buds) in fibromyxoid matrix along with acute and chronic inflammatory cells, characteristic of pyogenic granuloma (Figure 3). As the lesion was benign, immunohistochemistry was not required. The patient was given oral antibiotics and analgesics for one week and advised to follow up after one week. Sutures removed after one week. The wound appeared healed. Follow-up after three months showed no recurrence.
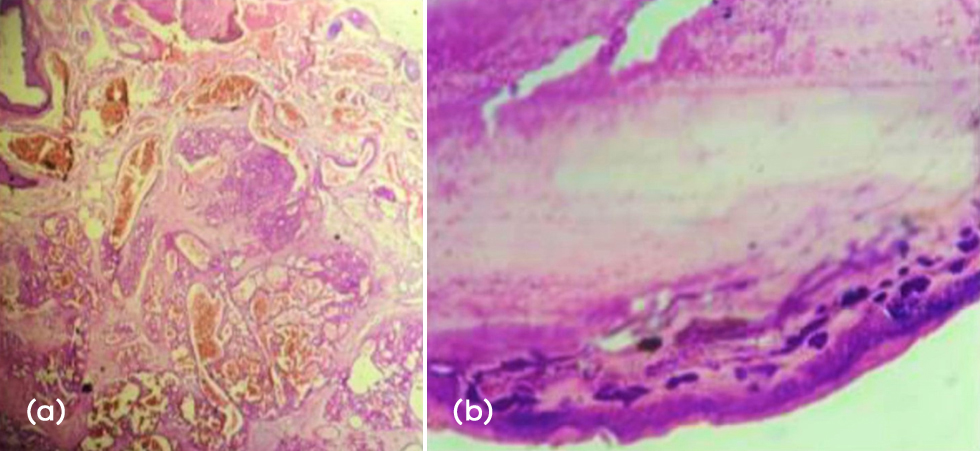
Figure 3: (a) Histopathological specimen showing lobules containing multiple endothelial lined vascular channels in fibromyxoid matrix along with acute and chronic inflammatory cells. (b) Histopathological slide showing ulcerated epithelium with secondary bacterial infection.
A complete excision biopsy of the mass performed with a margin of 4mm [17], and the skin defect was closed with interrupted sutures. A histopathological examination conducted on the excised mass.
Histopathology report revealed ulcerated epithelium with bacterial colonies, lobules containing multiple endothelial lined vascular channels (proliferating capillary buds) in fibromyxoid matrix along with acute and chronic inflammatory cells, characteristic of pyogenic granuloma (Figure 3). As the lesion was benign, immunohistochemistry was not required. The patient was given oral antibiotics and analgesics for one week and advised to follow up after one week. Sutures removed after one week. The wound appeared healed. Follow-up after three months showed no recurrence.
Discussion
Pyogenic granuloma commonly occurs on the skin and mucous membranes, trunk, head and neck, extremities, oral cavity, and nasal mucous membranes. The treatment modalities are the treatment modalities for cryosurgery, curettage, electrodesiccation, chemical cauterization, and laser surgery. A recent addition in managing oral lesions is sclerotherapy with monoethanolamine oleate [18]. Diode laser used for recurrent cases [19]. Ocular lesions are rare if involved in conjunctiva, cornea, and adnexa secondary to surgery, infection, or trauma. Pyogenic granuloma of the upper lid is a rare occurrence [20]. The differential diagnosis is burst chalazion, capillary hemangioma, molluscum contagiosum, pilomatricoma, basal cell carcinoma, squamous cell carcinoma, Kaposi’s sarcoma, periocular metastasis. The etiology of ocular pyogenic granuloma is previously discussed.
This is a rare case of upper eyelid pyogenic granuloma in a 40-year-old male patient, idiopathic in origin, which was surgically excised with surrounding normal tissue rim and sent to the histopathological examination, which confirmed the diagnosis.
Conclusion
Pyogenic granuloma should be considered as a differential diagnosis for eyelid swellings. Benign inflammatory lesions to be ruled out before considering malignant conditions. Surgical excision is the treatment of choice. Histopathological examination is the definitive tool to confirm the diagnosis. Follow-up is necessary to exclude recurrence.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Mills SE, Cooper PH, Fechner RE. Lobular capillary hemangioma: the underlying lesion of pyogenic granuloma. A study of 73 cases from the oral and nasal mucous membranes. Am J Surg Pathol. 1980; 4(5):470–479.
[2] Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): A clinicopathologic study of 178 cases. Pediatr Dermatol. 1991; 8(4):267–276.
[3] Jordan DR, Brownstein S, Lee-Wing M, Ashenhurst M. Pyogenic granuloma following oculoplastic procedures: An imbalance in angiogenesis regulation? Can J Ophthalmol. 2001; 36(5):260–268.
[4] Al-Towerki AA. Pyogenic granuloma. Int Ophthalmol. 1995; 19(5):287–291.
[5] Cosar CB, Cohen EJ, Rapuano CJ, Maus M, Penne RP, et al. Tarsorrhaphy: Clinical experience from a cornea practice. Cornea. 2001; 20(8):787–791.
[6] Papadopoulos M, Snibson GR, McKelvie PA. Pyogenic granuloma of the cornea. Aust N Z J Ophthalmol. 1998; 26(2):185–188.
[7] Chou TY, Perry HD, Donnenfeld ED, Solomon R. Pyogenic granuloma formation following placement of the Medennium SmartPLUG punctum plug. Cornea. 2006; 25(4):493–495.
[8] Ferry AP. Pyogenic granulomas of the eye and ocular adnexa: a study of 100 cases. Trans Am Ophthalmol Soc. 1989; 87:327-347.
[9] Clearfield E, Muthappan V, Wang X, Kuo IC. Conjunctival autograft for pterygium. Cochrane Libr. 2016; 2(2):CD011349.
[10] AlHarkan DH, AlOdan HA. Infected conjunctival pyogenic granuloma at strabismus surgery site mimicking conjunctival abscess. Saudi J Ophthalmol. 2019; 33(1):109–111.
[11] Damasceno EF, Pereira C, Damasceno NAP, Horowitz SAP, Amaral Filho OMB. Pyogenic granuloma after retinal detachment surgery with scleral buckle: Case report. Arq Bras Oftalmol. 2009; 72(4):543–544.
[12] Chendran P, Seng Fai T, Halim WHA, Din NM. Pyogenic granuloma formation following Ahmed valve glaucoma implant. J Glaucoma. 2019; 28(10):e162–e164.
[13] Bettich Z, El Moize Z, Benchekroune S, Ouafae Cherkaoui L. Granulome pyogénique de la conjonctive palpébrale chez un porteur de prothèse sclérale. J Fr Ophtalmol. 2018; 41(10):991–992.
[14] Srinivasan S, Prajna NV, Srinivasan M. Pyogenic granuloma of cornea: a case report. Indian J Ophthalmol. 1996; 44(1):39–40.
[15] Mietz H, Arnold G, Kirchhof B, Krieglstein GK. Pyogenic granuloma of the cornea: report of a case and review of the literature. Arbeitsphysiologie. 1996; 234(2):131–136.
[16] Abateneh A, Bekele S. Case report: Corneal pyogenic granuloma: Rare complication of infectious keratitis. Ethiop J Health Sci. 2014; 24(1):85.
[17] Mouriaux F, Stefan A, Coffin-Pichonnet S, Verneuil L, Rousselot P. Quelles marges d’exérèse pour les carcinomes de paupières ? J Fr Ophtalmol. 2015; 38(2):154–158.
[18] Matsumoto K, Nakanishi H, Seike T, Koizumi Y, Mihara K, et al. Treatment of pyogenic granuloma with a sclerosing agent. Dermatol Surg. 2001; 27(6):521–523.
[19] Rai S, Kaur M, Bhatnagar P. Laser: a powerful tool for treatment of pyogenic granuloma. J Cutan Aesthet Surg. 2011; 4(2):144–147.
[20] Ergün SS, Kocabora MS, Su Ö, Demirkesen C. Surgical treatment of giant pyogenic granuloma of the upper eyelid. Ann Ophthalmol (Skokie). 2007; 39(3):264–266.