Full Text
Introduction
In India the standard of care for gynecological cancers is laparotomy. Laparoscopy has its own advantages of minimal invasive route but the intuitive technique of robotics is advantageous in pelvic surgeries. Robotic surgery is a newer approach in medical science. Therefore comparison of open and robotic surgery will provide evidence of advantages in robotic surgery in current practice. The radical hysterectomy for early stage endometrial cancer done by both route and comparison of the surgical technique as well as peri/ post-operative outcome in the present study has shown promising results in robotic route.
To compare the safety, morbidity, perioperative outcome between robotic and open radical hysterectomy in the treatment of endometrial cancer.
Material and methods
The prospective data collection started for all women diagnosed with endometrial cancer who were planned for type 1 radical hysterectomy with bilateral pelvic lymph node dissection (RH) at tertiary care center of Hyderabad, India from May 2012 to April 2014. The diagnosed cases were offered both open and minimal invasive route for the management of the diseases and decision of selection of route of surgery was done by the patient. Minimal invasive route included both laparoscopic and robotic both the techniques and once laparoscopic technique was opted by the patients they were excluded from the study.
During the defined period the cases were operated by the same surgical team trained in both the routes.
The age, body mass index (BMI), and co-morbid medical conditions for each patient were recorded. Peri and postoperative data was collected including intro-operative period (defined as veress needle insertion/skin incision to skin closure), estimated blood loss, pre- and post-operative hemoglobin values, need for transfusion, length of hospital stay, and re-operation or re-admission. Intraoperative complications identified which included vascular injuries, bladder or urologic injuries, soft tissue injury and conversion to laparotomy. Pathologic data collected were the volume of uterus, total number of lymph nodes retrieved, International federation of gynecology and obstetrics (FIGO) stage of tumor, and the histology and grade of the tumor. Incomplete charts were excluded from the study.
Surgical procedure
The procedure in both open and robotic assisted route was same. The cases were preoperatively diagnosed as stage 1 or occult stage II disease by routine ultrasonography/ magnetic resonance imaging (MRI) scan and endometrial biopsy. They were planned for surgical management by radical hysterectomy Type 1 with bilateral pelvic lymphadenectomy.
All patients received preoperative antibiotics to reduce the rate of wound infections. A clear liquid diet on the day before surgery followed by bowel preparation by Peglec (polyethelene glycol) preparation was given. After peglec patient was kept nil orally and intravenous fluids were given for the rest of the day. Regular breathing exercises were taught on the same day to continue after surgery. In both types of surgery, general anesthesia was given. Before surgery, vascular compression stockings above the knee were applied.
In open technique the duration of surgery was taken from skin incision to skin closure. The midline vertical incision to explore the abdomen followed by total hysterectomy and bilateral pelvic lymphadenectomy.
In robotic technique the patient was kept in extreme Trendelenburg position. The assessment of actual surgical time is little different from the previous one. The skin to skin duration was defined as total duration and again the docking time (the duration of attachment of instrument to trocar and insertion into the abdomen) was deducted from total duration of surgery and this duration was taken as actual duration of surgery.
The umbilical or supraumbilical port for camera and 10 cm lateral to central port on the either side just below the midclavicular line, two subsequent ports for instruments were used. Right side for first arm and left side for second arm of robot. The third arm port was 8-10 cm from second port at the line joining the Anterior Superior Iliac Spine (ASIS). On right side one assistant port was made midway to camera port and first arm port 8-10 cm.
The camera is inserted and operability is assessed. The first arm holds monopolar scissors, second arm holds bipolar forceps and third arm holds Maryland forceps. The assistant port used to hold suction cannula and Maryland grasper for use during the steps of surgery.
Steps of surgery
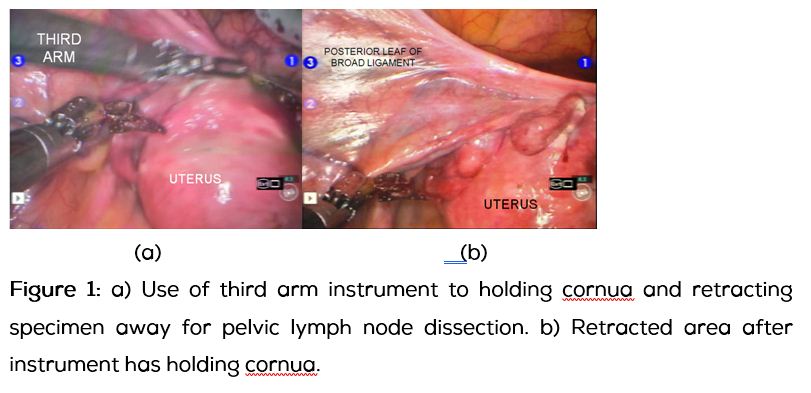
First the round ligament at lateral attachment and both fallopian tubes are coagulated at near the cornua to avoid any spillage from endometrial cavity. Now under vision uterine manipulator is inserted if uterus is found bulky and obstructing the surgical field for lymph node dissection. Most of the time we avoid use of manipulator and use the assistant port instrument and robotic third arm instrument to hold the uterus if required (Figures1a and 1b).
The round ligament is dissected and retroperitoneal space for lymph node dissection is mobilized. The lymphadenectomy is done prior to hysterectomy. This technique is surgeons preferred step for better achievement of surgical view during lymphadenectomy as well as it does not need any accessory retraction force throughout for dissection. The dissected lymph nodes of each side kept in colour coded separate pouch to retrieve later through vagina along with main specimen (Figure 2).

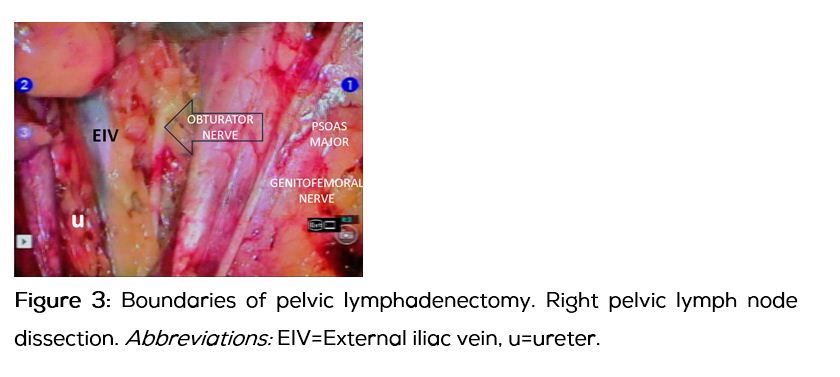
The lymphadenectomy started from visualization of lateral limit, genitofemoral nerve on psoas major followed by removal of lymph nodes from external iliac artery and vein till visualization of medial limit internal iliac artery. The extent of dissection is as follows. The dissection should go deep till the visualization of the obturator nerve and distal limit should be till the visualization of the iliac vein (Figure 3).
After lymphadenectomy both the uterine arteries are dissected and the bladder is mobilized down. The vault is open at the cervico-vaginal junction. Posteriorly the utero-sacrals are dissected. At the end both the infundibulo-pelvic ligaments are cut and the entire specimen is removed vaginally in robotic and abdominally in open technique. Vault is closed by interlocking sutures. Port sites are closed by vicryl 3-0 and stapler. In open technique abdomen closed in layers by vicryl 3-0 and skin by stapler.
Results
From May 2012 to April 2014 total sixty one cases underwent hysterectomy for endometrial cancer in the institute where the study is undertaken. Out of sixty one (100%) cases, 17(27.86%) were operated by open arm cohort (OA) and 25 (40.98%) by Robotic Arm cohort (RA) 13(21.31%) laparoscopically and 6(9.83%) cases with incomplete data.
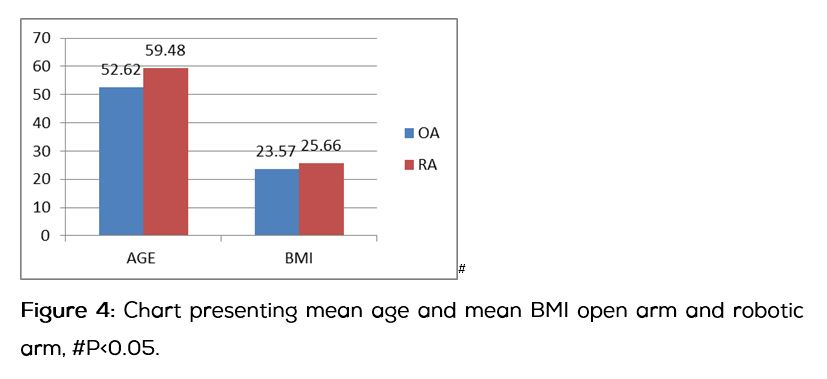
The baseline characters, which were included in the study as an important factor and taken into stastistical consideration were age and body mass index (BMI). We have found a significant difference in these two in RA. The mean age (52.62 yr ± 12.83Vs 59.48±8.62 yr, p<0.05) and BMI (23.57±3.39 Vs 25.66±3.21, p<0.05) respectively in OA Vs RA. The difference was statistically significant (Figure 4).
Comorbidities like diabetes, hypertension, asthma and thyroid disease are seen more in RA. Similarly the history of previous surgery was also significantly high in RA (Table 1).
Table 1: The associated co-morbid medical and surgical history in study group.
|
Comorbidities**
|
OA
n=17
|
RA
n=25
|
|
Htn
|
3
|
4
|
|
Diabetes
|
2
|
3
|
|
Htn+diabetes
|
1
|
7
|
|
Thyroid disease
|
0
|
1
|
|
Asthma
|
0
|
1
|
|
Surgical history*
|
2
|
10
|
Abbreviations: HTN=Hypertension, DM=Diabetes, *abdominal surgeries includes ceasarian section, tubectomy, appendicectomy. ** p>0.05 not statistically significant.
The mean duration of surgery was significantly less in OA as compare to RA (98.54 min±89.15 Vs 215.36min±32.18, p<0.05) but there was not a single case in RA required conversion to laparotomy. The estimated mean blood loss was found high in OA as compare to RA (227.05 ml±113.79 Vs 92.6ml±64.34, P<0.05). The need of blood transfusion intraoperatively or post operatively was high in OA though not statistically significant (Figure 5).

Robotic surgery did not compromise the disease as compare to open and it clearly reflected in the histopathology. Histopathological features included volume of uterus, tumor size, type of carcinoma and lymph node yield. The resected volume of uterus in OA and RA was almost similar (159.63 cm3±162.59 Vs147.19 cm3±137.45 p>0.05). The resected tumor diameter in the specimen was also similar in both arms (OA vs RA, 2.42 cm ± 1.79 Vs 3.50cm ±2.03, p>0.05). The types of carcinoma operated by either arm were endometroid carcinoma (82.36% vs 92%), serous carcinoma (5.88 vs 4%), mucinous variety (5.88 vs 0) and mixed mullerian tumor (5.58% vs 4%). The mean number of lymph nodes retrieved by RA was significantly high as compare to OA (15.84 Vs 11.82, P<0.05 ) (Table 2).
Table 2: Histopathological data of study population, p value >0.05. There was no statistical difference in tumor size and resected specimen by both routes.
|
|
Histopathological features
|
OA (n=17)
|
RA (n=25)
|
|
|
mean volume of uterus (in cm3)
|
159.63±162.59a
|
147.19±137.45a
|
|
|
mean diameter of tumor(in cm)
|
2.42 cm ± 1.79a
|
3.50cm ±2.03a
|
| |
|
OA % (n=17)
|
RA % (n=25)
|
|
Type of cancer
|
Endometroid
|
14(82.36)
|
23(92)
|
|
|
serous adenocarcinoma
|
1(5.88)
|
1(4)
|
|
|
Adenocarcinoma with mucin component
|
1(5.88)
|
1(4)
|
|
|
MMT
|
1(5.88)
|
0(0)
|
|
Grade of tumor
|
Grade 1
|
13(76.47)
|
16(64)
|
|
|
Grade 2
|
1(5.88)
|
4(16)
|
|
|
Grade 3
|
3(17.65)
|
5(20)
|
Abbreviations: MMT=Mixed mullerian tumor.
The peri and post-operative complications like paralytic ileus, lymphedema, pulmonary and cardiovascular event noted but there was no statistically significant difference in both the groups (Table 3).
Table 3: The perioperative and post-operative complication in study population.
|
Complications#
|
OA (N=17)
|
RA (N=25)
|
|
Bladder injury
|
1
|
0
|
|
Soft tissue injury
|
1
|
1
|
|
Vascular injury
|
2
|
1
|
|
Paralytic ileus
|
1
|
1
|
|
Post OP wound infection
|
2
|
1
|
|
Cardiac complication
|
1
|
1
|
|
Pulmonary complication
|
0
|
1
|
Abbreviations: # p value >0.05 not significant.
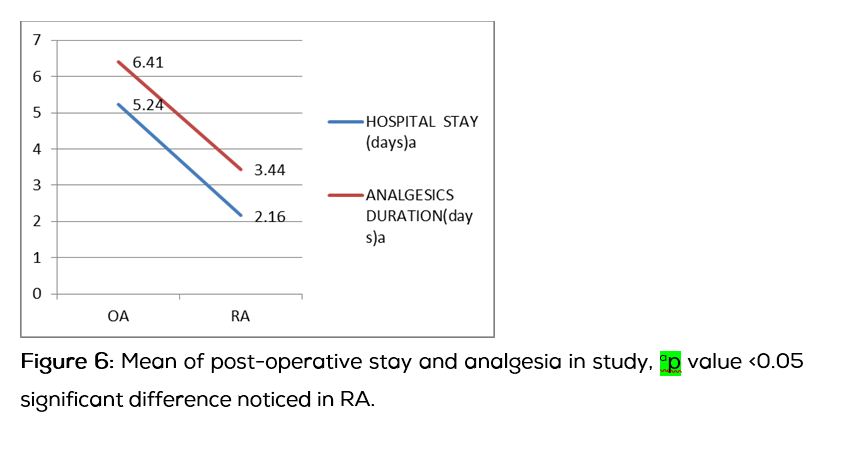
On the other hand the mean duration of analgesia (2.16 days±0.81 Vs 5.23 days ±0.97) hospital stay (3.4 days ±0.97 Vs 6.4 days ±1.41, p<0.05) and wound complication rate was low in RA (1/25) as compare to OA (2/17) (Table 3). The need of reoperation and readmission was not found in both the group (Figure 6).
The minimal follow up after 90 days of surgery done in the study. Three patients lost in follow up, one of RA and two of OA. Rests of the patients are doing well and alive till their last follow up and no recurrence or further morbidity noted. Eight cases underwent radiation (5vs 3 RA Vs OA) and one case required chemo radiation for cervical invasion in final histopathology (RA).
Discussion
Robotic surgery has got its pathway, now the era has come to direct the benefits of this medical intuitive technique in the current practice to achieve its better use in human hands. Previous author Seamon et al. has already compared the two minimal invasive techniques beautifully [1]. But the present study respected conventional technique and dared to compare it with newer modality. The current study is a boon for such upcoming challenges and may lead to a better support for medical plans.
In the present study robotic route has found statistically better in few aspects of surgery in comparison to traditional open technique. Despite of heterologous distribution in age, BMI, comorbidities, the elderly obese women with multiple comorbidities were operated by this newer technique. We compare duration of surgery, histopathology, post-operative morbidities also and they were quite satisfactory in RA.
Endometrial cancer is one of the disease diagnose in early stage and can be cured up to an extent by timed surgical management. The literature has conflicting and very limited evidences in the support of this medical intuitive, because of limited studies. In our study we have operated youngest 38 year to oldest 78 year with mean age in both the groups OA Vs RA (52.6 Vs 59.8 year) respectively. The results are absolutely contradictory from Maria et al. study who found the high age group in OA as compare to RA (72.3 year Vs 63.0 year) [2]. This study was a comparison of open, laparoscopy and robotic radical hysterectomy for endometrial cancer and included 40 cases in OA and RA. This interesting study has also reported difference in BMI in both the routes (OA Vs RA, 31.8 Vs 33.0) though not statistically significant [1]. In our study the range of BMI was 18-32 kg/m2 and the elderly obese patients were operated by RA (OA Vs RA 23.57 Vs 25.66, p<0.05). This was comparable to DeNardis SA et al. study, though they have operated BMI >40 kg/m2 too [3].
These elderly obese including the rest study population carried multiple comorbidities. High BMI, diabetes, hypertension are factors which increases the risk of development of endometrial cancer [4, 5]. Hypertension, diabetes, hypothyroidism alone or together seen more in RA. The further correlation of the factors to development of the disease was beyond the study objective.
In the present study we have found that duration of surgery was prolong in robotic route as compare to open (215.36 min Vs 98.54 min, p<0.05). The duration of surgery is in the range of previous studies of Veljovich et al. (302 min) [6], Gehrig et al. (189 min) [7], Maria et al. (184 min) [2], Joel CG et al. (237± 57 min) [8], Lowe MP et al. (170.5 min) [9]. The definition of duration of surgery in these studies is very much heterologus. The results are comparable and showed lesser duration of surgery as compare to Seamon et al. study (242 min±50). But it is tough to say because these studies have included para-aortic node dissection in some of the cases, which we have excluded [1, 10].
An interesting study by Mok ZW et al. reported that in the study the duration of surgery in robotic route was significantly high in the initial cases but later the difference was negligible [11]. When we compared our data in similar way the results were almost same though not statistically significant. In our analysis the first 12 cases were taking more time (219.3±32.4 min) than rest 13 cases (211.6±32.7 min) but did not show statistically significant difference (p>0.05). The interesting thing in our study is that there was significant difference in the study population for BMI and comorbidities, which was not seen in Mok Zw study [10]. Therefore the comment on duration difference cannot be done strongly in comparison to this study.
The conversion to open in the present study was zero. It may be by chance or may be due to loss of large number of cases opted laparoscopy. The study group included 25 cases only while previous studies showing conversion has done on large groups and the operating team included fellow surgeons learning the intuitive technique [7]. The volume of uterus is also a factor which has been considered most of the time for selection of route of surgery. We did not select the cases on this basis of size of uterus but after surgery the excised volume of uterus did not show any significant difference in both arms and comparable to study by Joel et al. [7] (Table 1).
The advantage of the minimal invasive technique is better visualization and magnified field along with special endowrist movement which provides feasibility of surgery [12]. The 3 D vision with magnified field at surgeons console gives quality approach on pelvic vessels situated in narrow space which is almost impossible in naked eye. The endowrist movement with 7 degree rotation gives more mobilsation even better than human hand. Therefore the lymph node dissection becomes far easier by robotic route as compare to open. In open the visibility is restricted and surgeons comfort is compromised. The advantages one can certainly calculate by seeing the lymph node retrieval rate which is significantly high in RA as compare to OA (15.84 Vs 11.82, p<0.05). The range of lymph node retrieval in the study was 11-23. Wide range of lymph node retrieval mentioned in previous studies and we are well enough comparable to them [1, 7, 9, 13]. In endometrial cancer the pelvic lymphadenectomy is only an indicator or prognostic marker [14]. The previous studies including our study clearly state that lymph node retrieval is far better in robotics as compared to open [1, 7, 9, 14]. A randomized trial on 514 subjects with early endometrial cancer reported by Benedetti Panici P et al. concluded that systematic pelvic lymphadenectomy statistically significantly improved the surgical staging but it did not improve disease-free or overall survival [15]. Looking into the evidences we too do not recommend Para aortic lymphadenectomy and limit our surgery up to bilateral pelvic lymphadenectomy though in that as well the results are questionable due to flaws in further management [16].
Fabien et al. have clearly mentioned in their study that LN metastasis is a real indicator of poor prognosis and requires an adapted adjuvant therapy. To date, lymphadenectomy is still the standard technique to assess the lymphatic spread of EC. However, its morbidity prompts us to define objective criteria to select patients who will benefit from such extensive staging [17].
The morbidity after surgery was assessed by blood loss, infection rate, hospital stay, need of analgesia and reoperation. In the present study the loss of blood and need of transfusions were significantly low in RA as compared to OA (227.05±113) and the minimal blood loss in RA (92.6±64 ml) is comparable to Leigh et al. study [5].
The length of hospital stay was less in RA as compare to OA (3.4 Vs 6.4 day). Even the requirement post-operative parenteral analgesia was for a shorter duration in RA as compared to OA (2.1 vs 5.2 day) which helped in early mobilization. The results were similar to other previous studies and it is agreed that robotic route provides early mobilization and pain is less in post-operative period, as compared to conventional technique [10, 18].
One of the post-operative complications in lymph node dissection is lymphoedema and prolonged duration of follow up in this regard. The precise lymph node dissection in robotic route provides minimal injury to lymphatics and nerves. In a study by Vidal Fabien et al. it was recommended that less invasive procedure may result in minimal chances of development of lymphedema. After reviewing the follow up in other studies, the chance of development of lymphedema is variable [17]. In the 3 to 27 months follow up observations from first to last patient included in the study, this complications is not observed in among.
In this present study the high risk cases that are found suitable for robotic route were selected because better visualization and precise tissue dissection will lesser the post operative complication.
Conclusion
The robotic route has given significantly better surgical outcomes, despite prolonged duration of surgery as compared to conventional open route. Robotic surgery is costlier for single sitting but in the long run is beneficial as compare to open technique. Robotic surgery has proven itself as a better option for Indian obese women along with other advantages like minimal blood loss, shorter hospital stay and minimal post-operative complications. It has equivalent outcomes in cure rate.
Acknowledgement
We appreciate the work of Dr. Satish & Dr. Sailaja (Pathologist) in providing us detailed histopathological study of the specimens provided. We thank Dr. V. Sudhindra Gupta for data assessment and giving his valuable time in appropriate statistics.
Conflict of interest
The authors declare no conflict of interest.
References
1. Seamon LG, Cohn DE, Henretta MS, Kim KH, Carlson MJ, et al. Minimally invasive comprehensive surgical staging for endometrial cancer: Robotics or laparoscopy? Gynecol Oncol. 2009; 113(1):36–41.
2. Bell MC, Torgerson J, Seshadri-Kreaden U, Suttle AW, Hunt S. Comparison of outcomes and cost for endometrial cancer staging via traditional laparotomy, standard laparoscopy and robotic techniques. Gynecol Oncol. 2008; 111(3):407–411.
3. DeNardis SA, Holloway RW, Bigsby GE, Pikaart DP, Ahmad S, et al. Robotically assisted laparoscopic hysterectomy versus total abdominal hysterectomy and lymphadenectomy for endometrial cancer. Gynecol Oncol. 2008; 111(3):412–417.
4. Szablewski L. Diabetes mellitus: influences on cancer risk. Diabetes Metab Res Rev. 2014; 30(7):543–553.
5. Park SL, Goodman MT, Zhang ZF, Kolonel LN, Henderson BE, et al. Body size, adult BMI gain and endometrial cancer risk: the multiethnic cohort. Int J Cancer. 2010; 126(2):490–499.
6. Field JB, Benoit MF, Dinh TA, Diaz-Arrastia C. Computer-enhanced robotic surgery in gynecologic oncology. Surg Endosc. 2007; 21(2):244–246.
7. Gehrig PA, Cantrell LA, Shafer A, Abaid LN, Mendivil A, et al. What is the optimal minimally invasive surgical procedure for endometrial cancer staging in the obese and morbidly obese woman? Gynecol Oncol 2008; 111(1):41–45.
8. Cardenas-Goicoechea J, Adams S, Bhat SB, Randall TC. Surgical outcomes of robotic-assisted surgical staging for endometrial cancer are equivalent to traditional laparoscopic staging at a minimally invasive surgical center. Gynecol Oncol. 2010; 117(2):224–228.
9. Lowe MP, Johnson PR, Kamelle SA, Kumar S, Chamberlain DH, et al. A multiinstitutional experience with robotic-assisted hysterectomy with staging for endometrial cancer. Obstet Gynecol. 2009; 114(2 Pt 1):236–243.
10. Seamon LG, Cohn DE, Richardson DL, Valmadre S, Carlson MJ, et al. Robotic hysterectomy and pelvic-aortic lymphadenectomy for endometrial cancer. Obstet Gynecol. 2008; 112(6):1207–1213.
11. Mok ZW, Yong EL, Low JJ, Ng JS. Clinical outcomes in endometrial cancer care when the standard of care shifts from open surgery to robotics. Int J Gynecol Cancer. 2012; 22(5):819–825.
12. Shafer A, Boggess JF. Robotic assisted endometrial cancer staging and Radical hysterectomy with Da Vinci surgical system. Gynecol Oncol. 2008; 111(2 suppl):s18–s23.
13. Hoekstra AV, Jairam-Thodla A, Rademaker A, Singh DK, Buttin BM, et al. The impact of robotics on practice management of endometrial cancer: transitioning from traditional surgery. Int J Med Robot. 2009; 5(4):392–397.
14. Tong SY, Lee JM, Choi YJ, Lee JK, Kim MK, et al. Efficacy of systematic pelvic lymphadenectomy in patients with non-endometrioid endometrial cancers: a retrospective, multicenter study in Korea. J Obstet Gynaecol Res. 2012; 38(11):1321–1327.
15. Benedetti Panici P, Basile S, Maneschi F, Alberto Lissoni A, SignorelliM, et al. Systematic pelvic lymphadenectomy vs. no lymphadenectomy in early-stage endome-trial carcinoma: randomized clinical trial. J Natl Cancer Inst. 2008; 100(23):1707–1716.
16. Naumann RW. The role of lymphadenectomy in endometrial cancer: was the ASTEC trial doomed by design and are we destined to repeat that mistake? Gynecol Oncol. 2012; 126(1):5–11.
17. Vidal F, Rafii A. Lymph Node Assessment in Endometrial Cancer: Towards Personalized Medicine. Obstet Gynecol Int. 2013; 2013:892465.
18. Lavoue V, Zeng X, Lau S, Press JZ, Abitbol J, et al. Impact of Robotics on the outcome of elderly patients with endometrial cancer. Gynecol Oncol. 2014; 133(3):556–562.