Full Text
Introduction
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis complex [1]. It usually affects the lungs but can affect any organ in the body [2]. Until 2019, before the emergence of corona virus pandemic, TB was the leading cause of death from a single infectious agent, ranking above HIV (human immunodeficiency virus) / AIDS (Acquired immunodeficiency syndrome) [3].
With advent of drug resistant tuberculosis, treatment of tuberculosis is even more challenging. All TB infected people do not necessarily get the disease with an estimated life time risk of 10-15%. This risk increases to 10% per year if the person is co-infected with HIV. There was an estimated TB deaths of 214000 (187000-242000) among HIV positive people in 2020 globally. In India the mortality was 11000 (9800-12000) among HIV positive TB patients [4].
Tuberculosis has existed for many years and it was in 1944, streptomycin, the first drug for treatment became available. Merely 12 years after its introduction in 1956, TB strains resistant to streptomycin, para-amino salicylic acid and isoniazid was discovered in great Britain. In subsequent years, strains with resistance to more drugs were reported and with discovery of extensively drug-resistant tuberculosis (XDR-TB) strains [5]. Globally 3 in every 1000 people carry multidrug-resistant tuberculosis (MDR-TB) infection [6].
Since the beginning of AIDS epidemic, tuberculosis was known to be a major cause of suffering and death [7]. Association of HIV infection, drug resistant TB and associated mortality together with lack of second line drugs in resource limited settings were called as the “perfect storm” [8].
Despite the evolution of well organised programmes for the diagnosis and management of drug resistant TB and HIV, the mortality is still high [9]. There is also insufficient data regarding the treatment outcome of MDR-TB in HIV patients despite the high incidence and prevalence. This study is intended to find out the treatment outcome in these patients and factors affecting the same.
The study was to assess the treatment outcome of multidrug resistant tuberculosis co-infected with HIV treated under programmatic management of drug resistant tuberculosis.
Material and methods
The study was conducted by Department of Respiratory Medicine in Princess Krishnajammanni Tuberculosis and Chest Diseases (PK TB & CD) Hospital, Mysore Medical College and Research Institute (MMCRI), Mysore, India from January 2013 to December 2019 after institutional ethical committee clearance. It is a retrospective study done on patients who were admitted in drug resistant tuberculosis center of PK TB & CD hospital, Mysore.
Inclusion criteria: All the cases of MDR tuberculosis co-infected with HIV who were admitted in PKTB& CD hospital for initiation of treatment.
Exclusion criteria: MDR tuberculosis with HIV co-infected patients who were started treatment in some other DRTB center and admitted in PKTB hospital for management of complication or adverse effects.
Methods and protocol
In patient records of all MDR-TB cases co-infected with HIV were collected and details about patients anti-tubercular treatment history, anti-retroviral treatment history, blood investigations, radiological picture shall be recorded. Treatment outcome was assessed and ascertained as per PMDT guidelines.
Statistical analysis
Descriptive and inferential statistical analysis has been carried out in the study. Data was entered in Microsoft Excel sheet. Chi square test for proportion and other related statistical tests along with suitable graphs used to study the treatment outcome in MDR-TB-HIV patients and data analysis was done using SPSS 21.0.
Results
This retrospective study was conducted among 63 MDR-TB patients co-infected with HIV admitted at PKTB and CD Hospital for initiation of treatment from 2013. The demographic details, clinical features, radiological assessment and treatment outcome were studied and the data was compiled, after statistical analysis using SPSS 21.0
Demographic details
Out of 63 patients studied 48(76.2%) were males and 15(23.8%) were females. Male to female sex ratio was 3.2 (Figure 1). The mean age of the study population was 39 years (38.58 + 1.23). 65%(41) of the patients belonged to the age group of 21-40 years (Figure 2). Out of the 63 patients, 58(92.1%) were married and 5(7.9%) were unmarried.
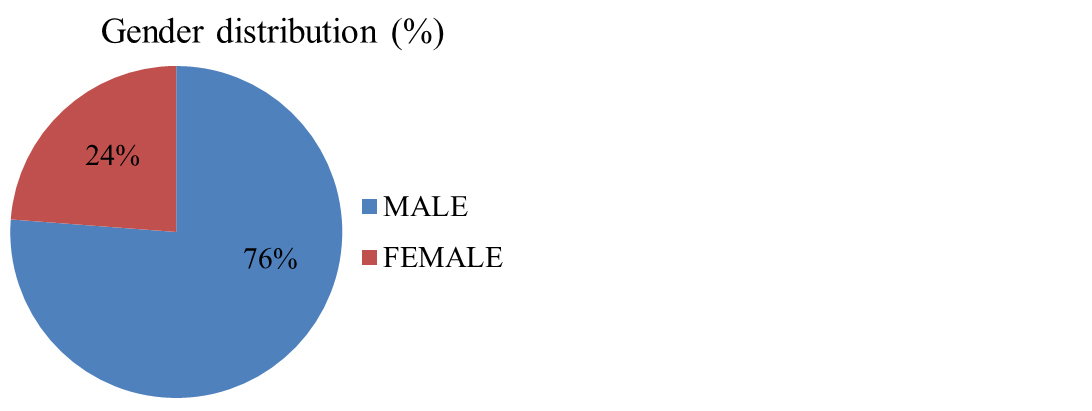
Figure 1: Gender distribution among the study population.
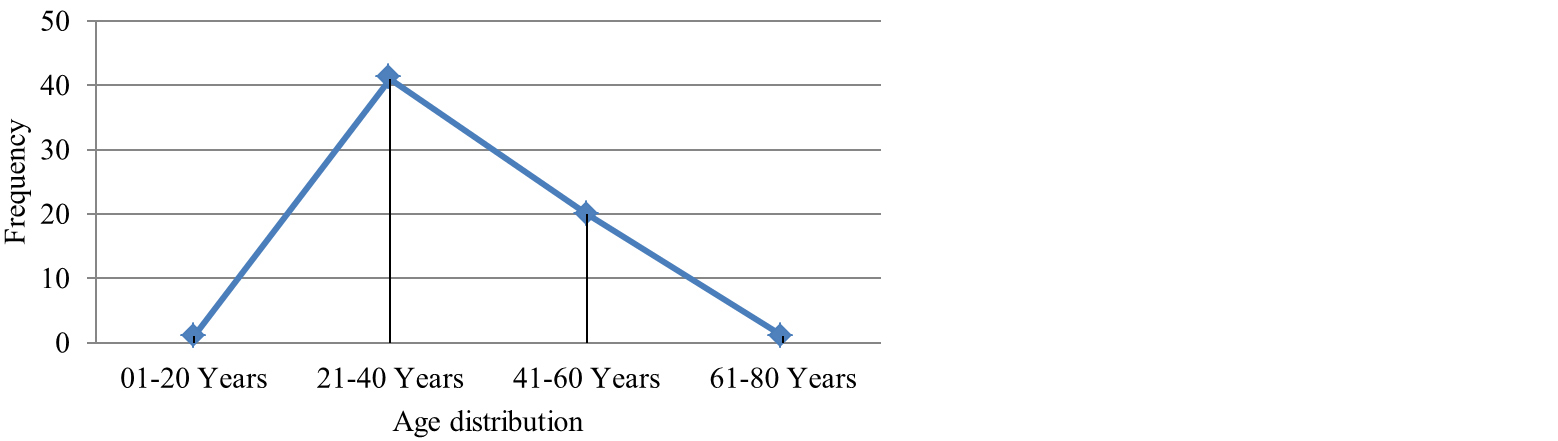
Figure 2: Age distribution among the study population.
Previous history of ATT: All the 63 patients had past history of TB. 43 patients (68.3%) had taken Category I treatment previously, 13 patients (20.6%) Category II, 4 patients (6.3%) had MDR-TB, 2 (3.2%) had XDR-TB in the past.
Table 1: Past history of anti-tubercular treatment.
|
Past ATT history
|
Number of patients
|
Percentage (%)
|
|
Category I
|
43
|
68.3
|
|
Category II
|
13
|
20.6
|
|
MDR
|
4
|
6.3
|
|
XDR
|
2
|
3.2
|
|
LFU
|
1
|
1.6
|
Clinical features: All the patients had fever as a common clinical feature. The next most common symptom was cough (98.4%), followed by loss of weight (96.8%), loss of appetite (96.8%), shortness of breath (63.5%), chest pain (55.6%). The less common presentations were hemoptysis (3.2%), seizure (3.2%), abdominal pain (1.2%), scrotal abscess (1.2%), LN swelling (1.2%) (Figure 3).
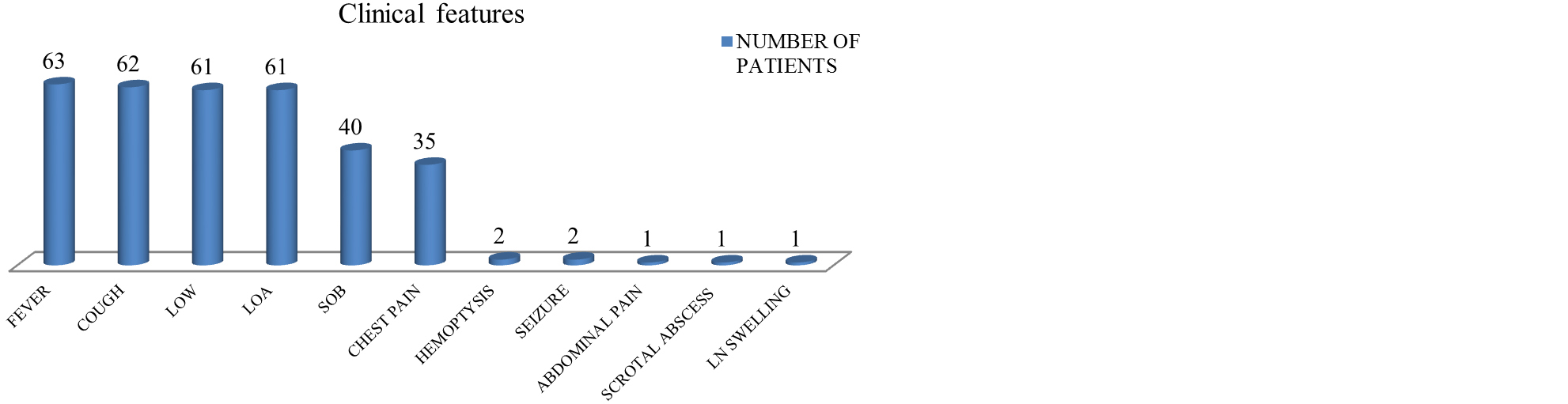
Figure 3: Symptomatology among the study population.
Radiological features: Among the study population, 29 (46%) patients had moderately advanced lesions in chest x-ray, 8 (12.7%) showed mild, 23 (36.5%) far advanced and 1 (1.6%) showed military pattern on chest radiograph. X-ray was normal in 2 patients (3.2%) (Table 2). The most common pattern on x-ray was infiltrates in 60 patients (95%), followed by cavity (51%). Other patterns were hilar lymphadenopathy and military pattern (Table 3).
Table 2: Radiological distribution among the study population.
|
Chest x-ray findings
|
Number
|
Percentage (%)
|
|
Normal
|
2
|
3.2
|
|
Mild
|
8
|
12.7
|
|
Moderately advanced
|
29
|
46
|
|
Far advanced
|
23
|
36.5
|
|
Miliary TB
|
1
|
1.6
|
Table 3: Pattern of chest lesions.
| |
Pattern on chest x-ray
|
Frequency
|
Percentage (%)
|
|
| |
|
1
|
Cavity
|
32
|
51
|
|
|
2
|
Infiltration
|
60
|
95
|
|
|
3
|
Miliary
|
1
|
0.01
|
|
|
4
|
Hilar lymphadenopathy
|
8
|
0.12
|
|
Site of tuberculosis: Majority of the patients had pulmonary tuberculosis (95.2%). Lymph node TB was seen in 2 patients (3.2%) and abdominal TB in 1 patient (1.6%) (Table 4).
Table 4: Site of tuberculosis.
|
Site
|
Number of patients
|
Percentage (%)
|
|
Pulmonary
|
60
|
95.2
|
|
Lymph node tuberculosis
|
2
|
3.2
|
|
Abdominal tuberculosis
|
1
|
1.6
|
ART treatment: Among the 63 patients diagnosed with MDR-TB and HIV, 4 patients (6%) were not taking ART and 59 (94%) were on ART (Figure 4).
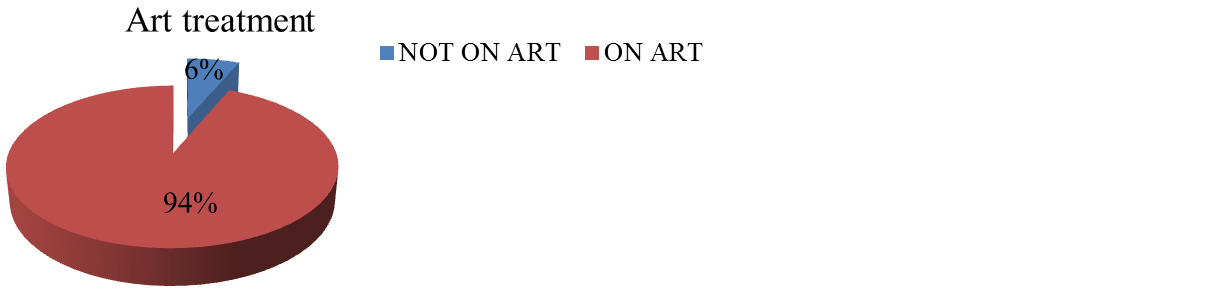
Figure 4: Patients on treatment for HIV.
Treatment outcome: Among the study population, 39.7% (25 patients) had an unfavorable outcome with death. 28.6% (18 patients) was declared cured and 12.7% (8 patients) declared treatment completed. 14.3% (9 patients) of the patients defaulted, 3.2% (2 patients) had treatment failure. 1.6% (1 patient) was transferred out from the DRTB centre.
Outcome among male and females were comparable and was not statistically significant (p value = 0.325). Past history of TB treatment was found not to affect the treatment outcome in the study population (p value = 0.316). It was also seen that the initial chest x-ray findings was not significantly affecting the outcome of treatment in these patients (p value = 0.458).
Clinical stage of HIV had a significant impact on treatment outcome. Out of the 22 patients (34.9%) in Stage II, 12 patients (54.5%) had a favourable outcome with cure and treatment completed. Among 14 patients (22.2%) in stage III HIV, 6 patients (42.9%) had favourable outcome, 3 patients (21.4%) died and 2 patients (14.3%) defaulted treatment. 27 patients (42.9%) patients were having Stage IV HIV, with death in 18 patients (66.7%), cure and treatment completed 4 patients (14.8%) each (Table 5).
HIV patients who were on ART had a better outcome compared to those who were not on treatment (p value = 0.004).
Table 5: Treatment outcome in MDR-TB patients co-infected with HIV.
|
Treatment outcome
|
Number of patients
|
Percentage (%)
|
|
Died
|
25
|
39.7
|
|
Cured
|
18
|
28.6
|
|
Defaulted
|
9
|
14.3
|
|
Treatment completed
|
8
|
12.7
|
|
Failed
|
2
|
3.2
|
|
Transfer out
|
1
|
1.6
|
Discussion
As indicated by the WHO global TB report 2019, in India, the burden of tuberculosis was found to be around 26.9 lakh in the year 2019 [10]. In the same year, deaths caused by TB were 4.40 lakhs. This is one of the significant concerns in India. In addition, the increase in the incidence of HIV creates a pavement for the further rise in TB incidence. Around 92,000 patients who are HIV positive in India are co-infected with TB, which further raises the disease burden.
We have evaluated 63 patients diagnosed with MDR-TB co-infected with HIV who were admitted at DRTB centre, Mysore from the year 2013 to 2019. In our study around 76.2% of study population was male and 23.8% of population was female. Also 92.1% were married and 7.9% were unmarried.
All the patients had fever as a common clinical feature. The next most common was cough (98.4%), followed by loss of weight (96.8%). According to a study published by Cain et al., cough, fever, night sweats and weight loss can be employed for active screening with a sensitivity of 85–93 percent and specificity of 30–40 percent [11].
Among the study population, 29 (46%) patients had moderately advanced lesions in chest x-ray, 8 (12.7%) showed mild, 23 (36.5%) far advanced and 1 (1.6%) showed military pattern on chest radiograph. CXR was normal in 2 patients (3.2%). There was lower zone predominance in these patients as observed in other studies.
However the extent of the disease on chest x-ray was not found to be a significant factor affecting treatment outcome in our study with a p value of 0.458. The most common pattern on x-ray was infiltrates in 60 patients (95%), followed by cavity (51%). Other patterns were hilar lymphadenopathy and military pattern.
Our study was consistent with another study conducted by Padyana et al. The study concluded that patients with HIV TB had atypical radiologic picture with diffuse or mid and lower zone involvement rather than classical upper lobe involvement. And patients with lower CD4 count had predominantly consolidation and non cavitory infiltration. Hence high index of suspicion is necessary for early diagnosis of tuberculosis in HIV patients [12].
The radiological pattern of PTB in HIV depends on the degree of immunosuppression. When the immune system is relatively intact the appearance that of reactivation of disease manifested by upper zone disease, fibrocavitary disease and as the level of immunosuppression increase rapid progression from initial infection to active disease occur which is usually associated with atypical chest x-ray findings in the form of middle and lower zone infiltrate, hilar lymphadenopathy and pleural effusion [13]. San et al. found 16.2 % of opacities in upper zones, 45% of parenchymal opacities in the middle and lower zone and 7.5% presented with miliary TB [14].
Among the 63 patients diagnosed with MDR-TB and HIV, 4 patients (6%) were not taking ART and 59 (94%) were on ART. Patients on ART had a better outcome compared to those who did not. This was statistically significant with a p value of < 0.05 (0.004).
This is in contrast to the study conducted by Umanah et al. that concluded patients who started ART before starting MDR-TB treatment had a greater mortality rate (21.8 percent vs. 15.4%) than patients who started ART after starting MDR-TB treatment (p = 0.013) [15].
Clinical stage of HIV had a significant impact on treatment outcome. Among patients with stage II HIV, 55.6 % (10 patients) got cured, only 16% (4 patients) died. Patients with stage IV HIV, 72% (18] died. This was found to be statistically significant with a p value of 0.002. Treatment outcomes differ in different regions of the world. A systematic review and meta-analysis conducted by Isaakidis et al revealed a pooled treatment-success rate of 56.9% (95% CI 46.2%– 67.6%): 49.9% (95% CI 38.5%–61.2%) among adults and 83.4% (95% CI 74.7%–92%) among children [13, 16,]. This emphasizes the importance of early recognition and treatment of HIV patients by screening the high risk population. In several other studies published, in the treatment of drug resistant TB and HIV, HIV was not independently associated with death [17, 18]. Early diagnosis of HIV to allow for early ART initiation, early diagnosis of MDR-TB with improved access to resistance testing for HIV-TB co-infected patients, and access to second-line anti-tuberculosis drugs are all critical for improving treatment success and survival in HIV–MDR-TB co-infected populations.
Advanced age, profound immune-suppression (CD4 count 100 cells/cm3), unemployment, male sex, smoking, pregnancy, drug misuse, co-infection with hepatitis B or C, and a higher degree of treatment resistance, including to second-line medications, were associated with poor outcomes.
Limitations
Though the study was conducted over six years, small sample size was the biggest limitation. However this could also indicate timely initiation of ART in the District which results in better immunity and lesser probability of getting tuberculosis. A multicentric study could provide a larger picture about the factors associated with treatment outcome among MDR tuberculosis patients and help in reducing the mortality.
Conclusion
HIV clinical stage and treatment with HAART had significant impact on treatment outcome emphasizing early recognition and treatment of HIV in general population. Age, Gender, symptomatology and radiological involvement was not found to be significant parameters affecting outcome of treatment in the study population. Thus early diagnosis and timely initiation of ART is the need of hour for HIV – MDR co infection. Also steps to be taken to reduce lost to follow up rates by appropriate management of adverse events.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Addo K, Owusu-Darko K, Yeboah-Manu D, Caulley P, Minamikawa M, et al. Mycobacterial species causing pulmonary tuberculosis at the korlebu teaching hospital, Accra, Ghana. Ghana Med J. 2007; 41(2):52–57.
[2] Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis. 2015; 78(2):47–55.
[3] Chakaya J, Khan M, Ntoumi F, Aklillu E, Fatima R, et al. Global tuberculosis report 2020 – Reflections on the global TB burden, treatment and prevention efforts. Int J Infect Dis. 2021; 113:S7–12.
[4] Tuberculosis (TB). Available from: https://www.who.int/news-room/fact-sheets/detail/tuberculosis
[5] Tuberculosis therapy: past, present and future | European Respiratory Society. Eur Resp J. 2002; 20(36):87S–94s.
[6] Knight GM, McQuaid CF, Dodd PJ, Houben RMGJ. Global burden of latent multidrug-resistant tuberculosis: trends and estimates based on mathematical modelling. Lancet Infect Dis. 2019; 19(8):903–912.
[7] Chamie G, Luetkemeyer A, Charlebois E, Havlir DV. Tuberculosis as part of the natural history of HIV infection in developing countries. Clin Infect Dis. 2010; 50 Suppl 3(Suppl 3):S245–S254.
[8] Wells CD, Cegielski JP, Nelson LJ, Laserson KF, Holtz TH. HIV infection and multidrug-resistant tuberculosis: the perfect storm.J Infect Dis. 2007; 196(Suppl 1):S86–S107.
[9] Gandhi N, Andrews J, Brust J, Montreuil R, Weissman D, et al. Risk factors for mortality among MDR- and XDR-TB Patients in a High HIV-prevalence setting. Int J Tuberc Lung Dis. 2012; 16(1):90–97.
[10] World Health Organization. Global tuberculosis report 2019. Available from: https://www.who.int/publications-detail-redirect/9789241565714
[11] Cain KP, McCarthy KD, Heilig CM, Monkongdee P, Tasaneeyapan T, et al. An Algorithm for tuberculosis screening and diagnosis in people with HIV. N Engl J Med. 2010; 362:707–716.
[12] Padyana M, Bhat RV, Dinesha M, Nawaz A. HIV-Tuberculosis: A study of chest x-ray patterns in relation to CD4 count. North Am J Med Sci. 2012; 4(5):221–225.
[13] van’t Hoog AH, Meme HK, Laserson KF, Agaya JA, Muchiri BG, et al. Screening strategies for tuberculosis prevalence surveys: The value of chest radiography and symptoms. Plos One. 2012; 7(7):e38691.
[14] San KE, Muhamad M. Pulmonary tuberculosis in HIV Infection : The relationship of the radiographic appearance to CD4 T-lymphocytes count. Malays J Med Sci MJMS. 2001; 8(1):34–40.
[15] Umanah T, Ncayiyana J, Padanilam X, Nyasulu PS. Treatment outcomes in multidrug resistant tuberculosis-human immunodeficiency virus co-infected patients on anti-retroviral therapy at Sizwe Tropical Disease Hospital Johannesburg, South Africa. BMC Infect Dis. 2015; 15(1):478.
[16] Isaakidis P, Casas EC, Das M, Tseretopoulou X, Ntzani EE, et al. Treatment outcomes for HIV and MDR-TB co-infected adults and children: systematic review and meta-analysis. Int J Tuberc Lung Dis. 2015; 19(8):969–978.
[17] Dheda K, Shean K, Zumla A, Badri M, Streicher EM, et al. Early treatment outcomes and HIV status of patients with extensively drug-resistant tuberculosis in South Africa: a retrospective cohort study. Lancet Lond Engl. 2010; 375(9728):1798–807.
[18] O’Donnell MR, Padayatchi N, Master I, Osburn G, Horsburgh CR. Improved early results for patients with extensively drug resistant tuberculosis and HIV in South Africa. Int J Tuberc Lung Dis. 2009; 13(7):855–861.