Full Text
Introduction
Chronic otitis media (COM) is defined as a chronic inflammation of the middle ear and mastoid cavity with recurrent ear discharge with a period ranging from 6 weeks to 3 months, though the World Health Organization (WHO) definition requires only 2 weeks of otorrhoea [1]. COM is classified into mucosal and squamosal disease [2], each with subtypes of “active” and “inactive” disease.
Chronic otitis media (COM) of mucosal type is characterized by a perforation of the pars tensa also called as central perforation [2]. The location of central perforations is denoted by their relationship to the handle of malleus as anterior, posterior and inferior [2]. Tympanic membrane (TM) protects the round window by shielding it from direct conduction of sound waves referred to as round window baffle [3]. A normally vibrating TM with its effective surface area plays a major role in the middle ear transformer mechanism and a perforation causes hearing impairment, the magnitude of which depends on the site of perforation with posterior quadrant perforations having more severe hearing loss than with other sites [4]. Hearing loss is the most common sequelae of COM and this may affect a child’s development in language skill and scholastic performance [5].
The aim of study was to find out the effect of site and size of TM perforations on hearing loss in inactive mucosal type of chronic otitis media. (i) To study the association of the site and size of tympanic membrane perforation with the degree of conductive hearing loss assessed by Pure Tone Audiometry (PTA) in patients with inactive chronic otitis media of mucosal type. (ii) To stress the importance of undergoing reconstructive surgery of the tympanic membrane and thereby improving the hearing in patients with inactive chronic otitis media.
Methodology
This was a hospital based descriptive cross-sectional study with the setting of the study at Government Medical College, Alappuzha during the period from November 2017 to March 2019 among patients with COM visiting the outpatient department (OPD) of ENT. Written informed consent was taken with the confidentiality of information maintained. Ethical clearance and approval of the protocol from the institutional review committee of Government Medical College, Alappuzha.
Convenience sampling method was done. Sample size (4pq/d2) was calculated using nMaster 2.0 software with linear relationship measured using regression co-efficient between tympanic membrane perforation size and hearing loss (air bone gap) expected to be 0.35, standard deviation of tympanic membrane perforation size 0.8 and standard deviation of air bone gap 1.8.
Patients with inactive COM of mucosal type of at least 6 months duration aged between 10 and 75 years, were included in the study with their consent. Patients with active ear discharge, granulation, cholesteatoma, hearing impairment of more than 60 decibels, meatal stenosis, exostosis and congenital hearing loss were excluded. Informed consent was obtained from all the patients. For data collection, a thorough history was taken in each case, followed by detailed examination and relevant investigations and the findings were collected in the proforma. The study variables were age, sex, laterality of the diseased ear, size of the TM perforation, location of the TM perforation and degree of hearing loss.
TM images were obtained by otoendoscopy using 2.7mm 0° Hopkins rod telescope. Images captured were analyzed by measuring the percentage area of tympanic membrane perforation in relation to total area using adobe acrobat area tool, to avoid errors from angle of view and proximity of the endoscope.
Percentage area of tympanic perforation was calculated as follows: Percentage area of perforation = {area of perforation / total area of tympanic membrane} *100
The patients were grouped as those with small, moderate, large, and subtotal perforations with the size categorized according to the percentage area of perforation as small (<25%), moderate (26-50%), large (51-75%) and subtotal (>75%).
Patients were also grouped based on the site of TM perforations as ‘anterior’, ‘posterior’ and ‘those involving both anterior and posterior’ in relation to an imaginary line running vertically down along the handle of malleus for convenience.
Pure tone audiometry test was done for all patients in a sound proof room and pure tone signals were delivered to the ear via air conduction and bone conduction at frequencies ranging from 125Hz to 8000Hz. The patient responded to the sound by signaling the examiner with a button.
Degree of hearing loss was calculated for the frequencies of 250Hz, 500Hz, 1000Hz, 2000Hz and 4000Hz using the clinical audiometer ‘GSI AUDIOSTAR PRO’. Data obtained were correlated with average hearing threshold levels of each ear.
Analyses are done using PASW 18 software.
Results
A total of 174 cases were enrolled for the study. The results were tabulated as follows. Table 1 show the age distribution of the study population with maximum cases of 53 in the age range of 31 to 40 years with a mean age of 41.78 years.
Table 1: Age distribution of the study population.
|
Age in years
|
Number of cases (N=174)
|
|
11-20
|
6
|
|
21-30
|
26
|
|
31-40
|
53
|
|
41-50
|
41
|
|
51-60
|
31
|
|
61-70
|
16
|
|
>70
|
1
|
The gender wise distribution of patients were 107 males and 67 females. The male to female ratio was 1.59:1. On considering the laterality of ear disease, there was slight left ear preponderance in 88 cases (50.57%) and 86 cases (49.43%) had right ear involvement.
Large size perforations were noted in 64 (36.8%) patients, moderate size in 57(32.8%) patients and 37 patients (21.3%) had small size perforations in the study group (Table 2).
Table 2: Distribution of different sizes of perforation among the group.
|
Size
|
Number of cases
|
Percentage (%)
|
|
Large
|
64
|
36.8
|
|
Moderate
|
57
|
32.8
|
|
Small
|
37
|
21.3
|
|
Subtotal
|
16
|
9.2
|
|
Total
|
174
|
100
|
By drawing an imaginary line through the handle of the malleus upto the inferior annulus, the perforations were also classified as “anterior” (group A), “posterior” (group B) and as those involving both anterior and posterior parts of the tympanic membrane (group C). Table 3 shows the number of patients with the distribution of perforations in relation to the handle of malleus. Posterior perforations were seen in 42 (24.1%) patients, 41 (23.6%) had anterior perforations, and 91 (52.3%) had perforations involving both anterior and posterior parts of the TM.
Table 3: Distribution according to the site of perforations.
|
Location
|
Number of cases
|
Percentage (%)
|
|
Anterior
|
41
|
23.6
|
|
Posterior
|
42
|
24.1
|
|
Both anterior and posterior
|
91
|
52.3
|
|
Total
|
174
|
100
|
Figure 1 shows the correlation of area of perforation versus the degree of hearing loss. Correlation was significant at 0.01level by the 2-tailed test. The degree of hearing loss showed a positive linear relationship with the area of perforation which was statistically significant.
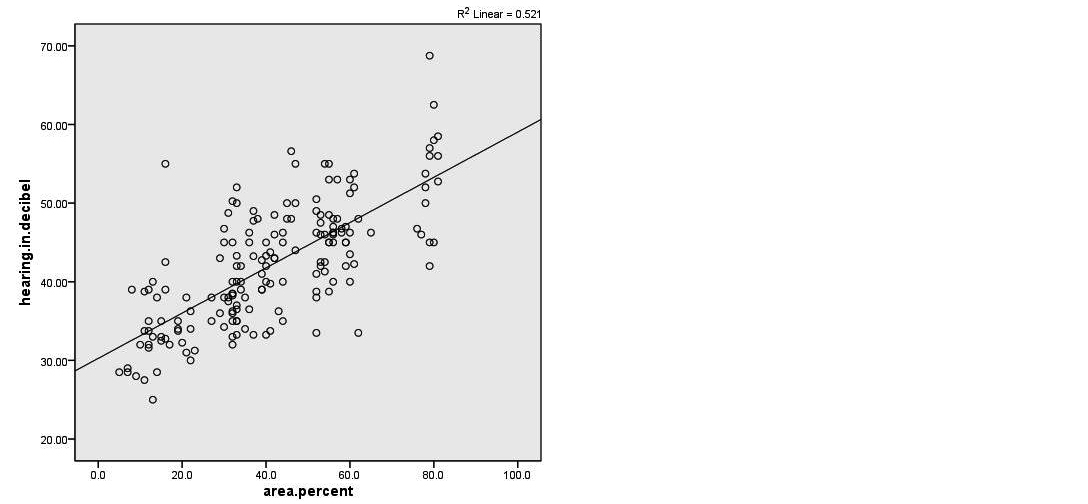
Figure 1: Correlations of area of perforation vs. degree of hearing.
The mean hearing in different groups according to the site of perforation were estimated and compared with the one way Anova test. The results are shown in Table 4. The mean hearing threshold level for group C was 46.3676, 39.5369 for group B and 35.3439 for group A. Standard deviation and standard error were calculated for the respective groups. The difference among the groups (by post hoc test) is found to be significant (p value <0.01).
Table 4: Mean hearing in different sites of perforation.
|
Group
|
Number
|
Mean hearing
|
Std. Deviation
|
Std. Error
|
|
Anterior (A)
|
41
|
35.3439
|
5.11789
|
0.79928
|
|
Posterior (B)
|
42
|
39.5369
|
6.29158
|
0.97081
|
|
Both anterior & posterior ©
|
91
|
46.3676
|
6.58640
|
0.69044
|
The mean hearing threshold in different groups according to the size of perforation was estimated and compared with the one way Anova test. The posterior group of tympanic perforations had a significantly higher degree of hearing impairment with a mean hearing of 39.54 decibels (dB) when compared with those with anterior tympanic perforations (mean hearing of 35.34 dB), the mean difference giving a p value of <0.01 (Table 5) which was significant.
Table 5: Multiple comparison for different quadrants of perforation (Hearing threshold level in decibel Bonferroni).
|
(I) site
|
(J) site
|
Mean difference (I-J) in hearing threshold level
|
Std. Error
|
Significance level.
|
95% Confidence interval
|
|
Lower bound
|
Upper bound
|
|
Posterior
|
Anterior
|
4.19300*
|
1.36135
|
0.007
|
0.9016
|
7.4844
|
|
Both anterior & posterior
|
Anterior
|
11.02368*
|
1.16633
|
0.000
|
8.2038
|
13.8436
|
|
Posterior
|
6.83068*
|
1.15672
|
0.000
|
4.0340
|
9.6273
|
Small perforations had a mean hearing of 34.00 +/_ 5.33 dB. Moderate sized perforations had a mean hearing of 39.93 +/_ 5.08 dB. Large perforations had a mean hearing of 46.01+/_ 4.91dB while the subtotal perforations had a mean hearing of 53.12+/_ 7.18 dB.
The results are shown in table 6. The difference among the groups (by post hoc test) is found to be statistically significant (p value <0.01).
Table 6: Mean hearing according to size of perforation.
| |
Number
|
Mean hearing
|
Std. Deviation
|
Std. Error
|
|
Subtotal
|
16
|
53.1250
|
7.18795
|
1.79699
|
|
Large
|
64
|
46.0148
|
4.90794
|
0.61349
|
|
Moderate
|
57
|
39.9307
|
5.08135
|
0.67304
|
|
Small
|
37
|
34.0027
|
5.32619
|
0.87562
|
|
Total
|
174
|
42.1213
|
7.74578
|
0.58721
|
Among the 4 groups each group was individually compared with the remaining 3 using post hoc analysis (Bonferroni test). The results were as follows (Table 7).
Table 7: Multiple comparison for different sizes of perforation.
|
Groups according to the perforation size
|
Mean Difference in size of perforation
|
Std. Error
|
P value
|
|
Subtotal
|
Large
|
7.11016*
|
1.47898
|
0.000
|
|
Moderate
|
13.19430*
|
1.49703
|
0.000
|
|
Small
|
19.12230*
|
1.58323
|
0.000
|
|
Large
|
Subtotal
|
-7.11016*
|
1.47898
|
0.000
|
|
Moderate
|
6.08414*
|
0.96368
|
0.000
|
|
Small
|
12.01214*
|
1.09279
|
0.000
|
|
Moderate
|
Subtotal
|
-13.19430*
|
1.49703
|
0.000
|
|
Large
|
-6.08414*
|
0.96368
|
0.000
|
|
Small
|
5.92800*
|
1.11710
|
0.000
|
|
Small
|
Subtotal
|
-19.12230*
|
1.58323
|
0.000
|
|
Large
|
-12.01214*
|
1.09279
|
0.000
|
|
Moderate
|
-5.92800*
|
1.11710
|
0.000
|
The comparison between the groups according to the size revealed a statistically significant difference of hearing impairment among each group.
The hearing threshold was lower in small sized perforations (<25% area involvement), which steadily rose as the area of tympanic membrane loss increased and had a maximum hearing loss in patients with perforations involving >75% area (subtotal).
Discussion
Prevalence of chronic otitis media among the rural population of India is estimated to be 46 per 1000 and in urban population 16 per 1000 [1]. Long term Eustachian tube dysfunction, poor aeration of the middle ear space, frequent episodes of otitis media and persistent middle ear infection are considered to be the causative factors of COM [6].
The degree of conductive hearing loss noted in COM patients depends on many factors like the size, site of perforation, middle ear volume, ossicular integrity etc. An intact TM is protective to the middle ear cleft and acts as a round window baffle by creating a phase differential so that sound waves do not impact on both the oval window and round window at the same time. Also, the ratio of the surface area of the TM to the surface area of the oval window increases the sound pressure by around 27 decibels, while the ossicular lever action contributes only by 3 decibels. A perforated tympanic membrane with its reduced surface area allows the sound to travel directly into the middle ear and a total loss of the TM will lead to a loss of the middle ear transformer mechanism and loss of surface area causes hearing impairment [3, 4].
Choffor-Nchinda et al. in a cross sectional study noted that the size of the tympanic membrane perforation was a predictor of the severity of hearing loss whereas site, duration and etiology did not seem to have any impact on hearing [7]. But the location of the perforation is also believed to have a significant effect on the magnitude of the hearing loss [7]. In the analytical study by Nahata et al in 2019, a linear relationship was found to exist between the size and degree of hearing loss and posterior perforations had a higher degree of hearing loss [8].
In this study population of 174 patients, the age distribution was from 14 years to 72 years with mean age of 41.78 +/- 13.1 years. Maximum cases (N=53) were in the age group of 31 to 40 years (30%) with a male: female ratio of 1.59:1. In a similar study by Singh in 2016 of 100 cases with COM, the maximum number of patients were in the age group of 41 to 50 years with a male to female ratio of 1.38:1 [9], while Pannu et al in their study of 100 patients noted the mean age of patients as 28.27 +/- 11.59 years with a male to female ratio 1.1:1 [10] whereas Maharajan et al. noted a female preponderance in his study [11].
In our study, 88 patients (50.57%) had left ear and 86 patients (49.43%) had right ear involvement. Left ear predominance also was noted by Pannu et al [10] and Maharjan et al [11].
In this study 91 patients (52.3%) had perforations involving both anterior and posterior quadrants followed by 42 patients (24.1%) with posterior and 41 (23.6%) with anterior perforations. Similar distribution of perforations was found in the study by Singh et al [9] and Maharjan et al [11] while, the study group of Pannu et al [10] had maximum number of patients with anterior perforations (38%) followed by perforations with multiple quadrant involvement (33%).
The effect of loss of the “round window baffle” on hearing threshold is displayed in this study. Perforations posterior to the handle of malleus were found to have maximum hearing loss with a mean hearing of 39.54 dB when compared to those perforations anterior to handle of malleus (35.34 dB) as shown in Table 4. The mean hearing loss of those with perforation involving both anterior and posterior quadrants was 46.37 decibel, which was significantly higher (p value <0.001) than the loss in the other two groups. This may be due to the additional effect of loss of more vibratory area of the tympanic membrane. The difference in hearing threshold between the anterior and posterior perforations was statistically significant with a p value = 0.007 (Table 5). Similar findings were noted in the study of Maharjan et al [11] where they demonstrated a significant correlation between posterior based perforation and hearing loss with a p-value=0.000. On the other hand, the relation between anterior perforations with the degree of hearing loss was not significant (p value: 0.422).
Similar observations were made by Ahmed et al [4] Voss et al [12] and Ibekwe et al [3] unlike the studies conducted by Mehta et al [13] and Oluwole et al [14] where there was no significant difference in the hearing loss in anterior versus posterior perforations.
In the present study the patients were grouped as small, moderate, large and subtotal based on the percentage area involved by the perforation in the TM (Table 7). Highest numbers of patients were with large sized perforations involving 51 to 75% of area of TM. The mean hearing threshold in small sized perforations was 34 dB whereas that of moderate sized perforations was 39.9 dB. Large perforations had a mean hearing threshold of 46 dB while the subtotal perforations had 53.1 dB of mean hearing. These figures highlight a steadily rising tendency of degree of hearing loss with respect to the increase in the size of tympanic membrane perforations. The comparison between each group showed a statistically significant association (p value of 0.000).
Similar observations were made by Singh et al [9] where they grouped perforations into 3 types (size of 1- 16mm2, 17 – 32 mm2 and >32 mm2) based on the actual area of perforation. Hearing loss was greater in larger perforations compared to the small perforations. The hearing loss threshold ranged from 43.7 to 59.8 dB.
Similar observation was made in the study by Pannu [10] where the patients were grouped into 3 sizes of 0-9mm2, 9-30mm2 and >30mm2. They observed a mean hearing threshold level of 23.9 dB, 32.09 dB and 45.5 dB respectively. The difference in their study was also statistically significant (p- value <0.001).
Maharjan et al [10] found in his study of 72 cases, noted that patients with larger perforation involving all the four quadrants of the TM showed greater hearing loss with large air bone gap. They found a significant relationship between hearing loss and size of perforation (p value <0.05) with a strong trend for the hearing loss to be more with increase in the perforation size.
Voss et al [12] Ahmed et al [4] Ibekwe et al [3] Oluwole et al [14] and Mehta et al [13] also found that larger the perforation on the tympanic membrane, greater was the decibel loss in sound perception.
Study by Mehta et al emphasizes the importance of determining other factors of hearing loss in a perforated TM and noted that the hearing loss was frequency dependent with more loss at lower frequencies and increased with the size of the perforation, but not with its location and inversely proportional to the volume of the middle ear and mastoid air space [13]. In our study these factors were not taken into account for as they were beyond the scope of this study.
The results of this study emphasise the chances of hearing improvement in patients with inactive mucosal COM by doing tympanic membrane reconstruction (myringoplasty or type 1 tympanoplasty). According to our findings, benefits of the reconstruction will be more for the patients with large perforations as well as for those with loss of the posterior part of tympanic membrane, which will significantly improve their quality of life and performance. The relevance of this study lies in the fact that it was conducted in the district of Alappuzha in Kerala among a population with a low socioeconomic background and that the prevalence of COM is high in a developing country like India [1].
Also, it is the most important cause of preventable hearing loss [15]. Unless intervened early enough, hearing impairment and associated morbidities can severely affect these patients which would have once been a treatable condition and of immense benefit especially to the younger generation of patients.
Limitation
Relationship of hearing impairment with changing frequency, volume of middle ear space, and with changes in eustachian tube functions were not considered in this study.
Conclusion
Chronic otitis media is a highly prevalent condition and an important cause of preventable hearing loss. This study was done to assess the relationship between the size and site of the tympanic membrane perforation and the degree of hearing impairment and it was concluded that hearing impairment increases with the size of the perforation. Also, location wise, the hearing impairment was more in posteriorly situated perforation than anteriorly locatedwhich was found to be significant statistically.
Acknowledgement
The authors acknowledge the help of all health-care workers, the Audiology department of ENT.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] World Health Organization. Chronic suppurative otitis media - Burden of Illness and Management Options, WHO Libr. Cat Data. 2004: 84. Available from: https://apps.who.int/iris/bitstream/handle/10665/42941/9241591587.pdf
[2] Browning GG, Merchant SN, Kelly G, Swan IR, Canter R, et al. Chronic otitis media Chapter 237c: In Kerr AG, editor. Scott-Brown’s Otolaryngology 7th ed. Vol 3. London: Arnold; 2008:3395–445.
[3] Ibekwe TS, Nwaorgu OG, Ijaduola, TG. Correlating the site of tympanic membrane perforation with Hearing loss. BMC Ear Nose Throat Disord. 2009; 9:1.
[4] Ahmad SW, Ramani GV. Hearing loss in perforations of the tympanic membrane. J Laryngol Otol. 1979; 93(11):1091–1098.
[5] Mittal R, Lisi CV, Gerring R, Mittal J, Mathee K, et al. Current concepts in the pathogenesis and treatment of chronic suppurative otitis media. J Med Microbiol. 2015; 64(10):1103–1116.
[6] Alam M, Sultan A, Chandra K. Microbiological assessment of chronic otitis media: Aerobic culture isolates and their antimicrobial susceptibility patterns. Indian J Otolaryngol Head Neck Surg. 2021; pp.1–7.
[7] Choffor-Nchinda E, Djomou F, Meva'a Biouele RC, Mindja D, Bola A, et al. Determinants of hearing loss severity in tympanic membrane perforations in a sub-Saharan African setting. J Laryngol Otol. 2018;132(11):1013–1017.
[8] Nahata V, Patil CY, Patil RK, Gattani G, Disawal A, et al. Tympanic membrane perforation: its correlation with hearing loss and frequency affected—an analytical study. Indian J Otol. 2014; 20(1):10–15.
[9] Singh R, Srivastava A, Mohan C. Comparative evaluation of hearing in different tympanic membrane perforations. Indian J Otol. 2016; 22(4):258–261.
[10] Pannu KK, Chadha S, Kumar D, Preeti. Evaluation of hearing loss in tympanic membrane perforation. Indian J Otolaryngol Head Neck Surg. 2011; 63(3):208–213.
[11] Maharjan M, Kafle P, Bista M, Shrestha S, Toran KC. Observation of hearing loss in patients with chronic suppurative otitis media tubotympanic type. Kathmandu Univ Med J. 2009; 7(28):397–401.
[12] Voss SE, Rosowski JJ, Merchant SN, Peake WT. Middle-ear function with tympanic-membrane perforations. I. Measurements and mechanisms. J Acoust Soc Am. 2001; 110(3 Pt 1):1432–1444.
[13] Mehta RP, Rosowski JJ, Voss SE, O'Neil E, Merchant SN. Determinants of hearing loss in perforations of the tympanic membrane. Otol Neurotol. 2006; 27(2):136–143.
[14] Oluwole M, Mills RP. Tympanic membrane perforations in children. Int J Pediatr Otorhinolaryngol. 1996; 36(2):117–123.
[15] Bellad SA, Kavi A, Mudhol RS. Prevalence of chronic suppurative otitis media among school children residing in rural area of Belagavi, South India. Indian J Otolaryngol Head Neck Surg. 2019; 71(Suppl 2):1549–1552.