Full Text
Introduction
Vitamin D is a group of fat-soluble steroids responsible for intestinal absorption of calcium and phosphate. In humans, the most important related compounds of vitamin D are vitamin D2 and vitamin D3. Vitamin D is not strictly a vitamin since it can be synthesized in the skin, and under most conditions that is its major source. Only when sunlight is inadequate is a dietary source required. The main function of vitamin D is in the regulation of calcium absorption and homeostasis; most of its actions are mediated by way of nuclear receptors that regulate gene expression. Deficiency leads to rickets in children and osteomalacia in adults continues to be a problem in northern latitudes, where sunlight exposure is poor.
Prevalence
In a world it has been estimated that 1 billion people have vitamin D deficiency or insufficiency. According to several studies, 40 to 100% of U.S. and European elderly men and women still living in the community (not in nursing homes) are deficient in vitamin D. More than 50% of postmenopausal women taking medication for osteoporosis had suboptimal levels of 25-hydroxyvitamin D below 30 ng per milliliter (75 nmol). In India the prevalence is between 70 -98 percent. There is difference in prevalence from North and south of India. Interestingly seasonal variation in vitamin D levels observed. In winter vitamin D levels are as low as 4 to 5 ng/ml. In Andhra Pradesh, studies has shown –mean 25 hydroxyl vitamin d—17 ng /ml in urban &18 ng/ml in rural areas in children. In Pregnant and lactating women –84-93%. Vitamin D deficiency (VDD, serum 25(oH) D levels < 20 ng/ml) was present in 1228 (91.2%) and vitamin D insufficiency [VDI serum 25(oH) D levels 20-<30 ng/ml) in 92(6.8%). There was no significant difference in prevalence of either VDD or VDI between two age groups and sexes. Serum 25(oH) D levels were negatively correlated with PTH levels (r -0.027, p <0.00001) and bmI (r -0.128, p 0.05). Prevalence of secondary hyperparathyroidism increased from 14.1% to 43.1% from VDI to severe VDD. PTH levels started rising at vitamin D level <30 ng/ml. However, more than 50% of subjects with severe VDD had PTH levels within normal range. Sensible sun exposure can provide an adequate amount of vitamin D3, which is stored in body fat and released during the winter, when vitamin D3 cannot be produced. Exposure of arms and legs for 5 to 30 minutes (depending on time of day, season, latitude, and skin pigmentation) between the hours of 10 am and 3 pm twice a week is often adequate.
Seasonal variation and vitamin D
Vitamin D status may fluctuate throughout the year, with the highest serum 25 (OH) D levels occurring after the summer and the lowest serum 25(OH) D concentrations after winter. A study by Shoben at el [1] demonstrated that mean serum 25(OH) D concentrations can vary as much as 9.5 ng/mL.
Vitamin D and absorption in dark skin
Darker skin interferes with the cutaneous synthesis of vitamin D, because of increased melanin content, competing with vitamin D. A study by Holick et al [2] demonstrated that non-Hispanic black subjects require 6 times the amount of UV radiation necessary to produce a serum vitamin D concentration similar to that found in non-Hispanic white subjects. Dawson-Hughes et al. [3] demonstrated that in Boston, 73% of elderly black subjects were vitamin D insufficient, compared with 35% of elderly non-Hispanic whites.
Common in Indians
Poor sun exposure, worried about skin texture, sun screen lotions usage. Clothing habits, cultural, Skin pigmentation, melanin, Food habits and lack of fortification. Negligible vitamin D available in diet of Indians.
Vitamin D metabolism
Vitamin D has a potent effect to increase calcium absorption from the intestinal tract; it also has important effects on both bone deposition and bone absorption. However, vitamin D itself is not the active substance that actually causes these effects. Instead, vitamin D must first be converted through a succession of reactions in the liver and the kidneys to the final active product, 1, 25-dihydroxycholecalciferol, also called 1, 25(OH) 2D3.
Skin: Cholecalciferol (Vitamin D3) is formed in the skin. Several compounds derived from sterols belong to the vitamin D family, and they all perform more or less the same functions. Vitamin D3 (also called cholecalciferol/ calcitriol) is the most important of these and is formed in the skin as a result of irradiation of 7-dehydrocholesterol, a substance normally in the skin, by ultraviolet rays from the sun. Consequently, appropriate exposure to the sun prevents vitamin D deficiency. The additional vitamin D compounds that we ingest in food are identical to the cholecalciferol formed in the skin, except for the substitution of one or more atoms that do not affect their function.
Liver: Cholecalciferol is converted to 25-Hydroxycholecalciferol in the liver. The first step in the activation of cholecalciferol is to convert it to 25-hydroxycholecalciferol; this occurs in the liver. The process is a limited one, because the 25-hydroxycholecalciferol has a feedback inhibitory effect on the conversion reactions. This feedback effect is extremely important for two reasons. First, the feedback mechanism precisely regulates the concentration of 25-hydroxycholecalciferol in the plasma, an effect that is shown in Figure 1. Note that the intake of vitamin D3 can increase many times and yet the concentration of 25-hydroxycholecalciferol remains nearly normal. This high degree of feedback control prevents excessive action of vitamin D when intake of vitamin D3 is altered over a wide range. Second, this controlled conversion of vitamin D3 to 25-hydroxycholecalciferol conserves the vitamin D stored in the liver for future use. Once it is converted, it persists in the body for only a few weeks, whereas in the vitamin D form, it can be stored in the liver for many months.
Kidney: Formation of 1, 25-Dihydroxycholecalciferol in the kidneys and its control by Parathyroid Hormone. Figure 1 also shows the conversion in the proximal tubules of the kidneys of 25-hydroxycholecalciferol to 1, 25- dihydroxycholecalciferol. Therefore, in the absence of the kidneys, vitamin D loses almost all its effectiveness. Note that the conversion of 25- hydroxycholecalciferol to 1, 25-dihydroxycholecalciferol requires PTH. In the absence of PTH, almost none of the 1, 25-dihydroxycholecalciferol is formed. Therefore, PTH exerts a potent influence in determining the functional effects of vitamin D in the body.
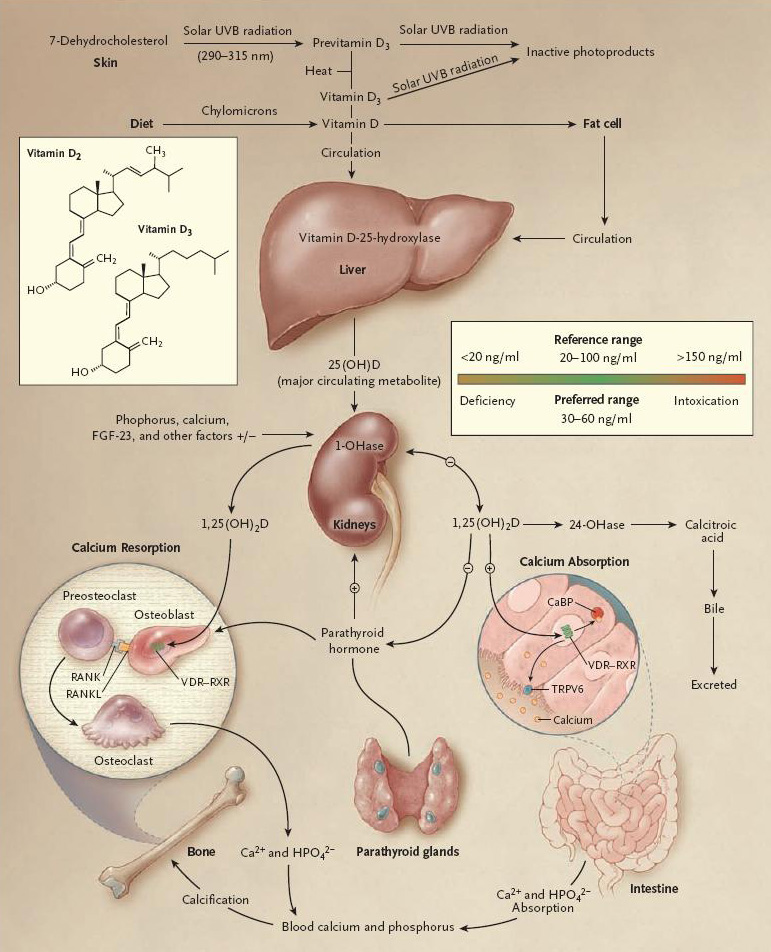
Figure 1: Vitamin D metabolism.
Vitamin deficiency
Without vitamin D, only 10 to 15% of dietary calcium and about 60% of phosphorus is absorbed. The interaction of 1,25-dihydroxyvitamin D with the vitamin D receptor increases the efficiency of intestinal calcium absorption to 30 to 40% and phosphorus absorption to approximately 80%. Risk of chronic disorders, infections, cancer are more in patients without vitamin D. Vitamin D is found in only a few foods (Figure 2), with fatty fish and fish oils, liver, meat and eggs being the main natural sources.
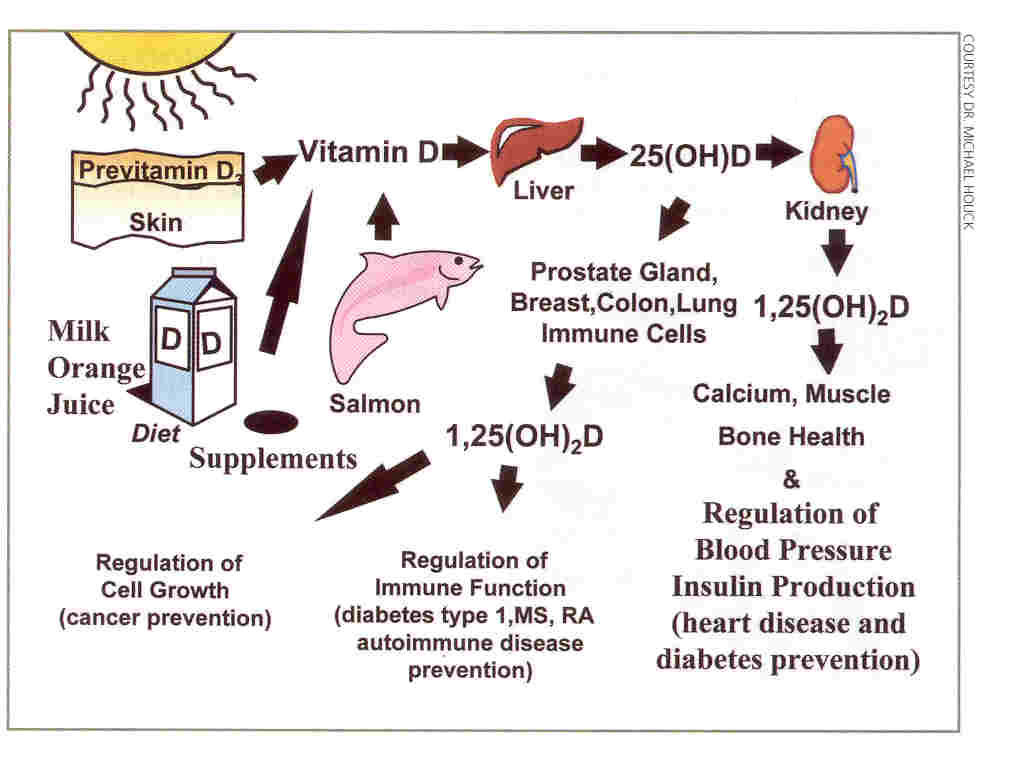
Figure 2: Source of vitamin D.
Vitamin D levels in blood
- Vitamin D adequacy— 30ng/ml above
- Vitamin D inefficiency— 21 – to 29 ng/ml
- Vitamin D deficiency— < 20ng/ml
- Severe vitamin D Deficiency— <5 ng/ml
- Vitamin D Excess— above 150ng/ml
- 25 hydroxyl vitamin D-barometer of vitamin D in the body
- The 1, 25- dihydroxy vitamin D assay should never be used for detecting vitamin D deficiency because levels will be normal or even elevated as a result of secondary Hyperparathyroidism.
Evidence for different disorders
Vitamin D and cancers
People living at higher latitudes are at increased risk for Hodgkin’s lymphoma as well as colon, pancreatic, prostate, ovarian, breast, and other Cancers and are more likely to die from these cancers, as compared with people living at lower latitudes. Both prospective and retrospective epidemiologic studies indicate that levels of 25-hydroxyvitamin D below 20 ng per millilitre are associated with a 30 to 50% increased risk of incident colon, prostate, and breast cancer, along with higher mortality. An analysis from the Nurses’ Health Study cohort (32,826 subjects) showed that the odds ratios for colorectal cancer were inversely associated with median serum levels of 25-hydroxyvitamin D. (The odds ratio at 16.2 ng per millilitre [40.4 nmol per liter] was 1.0, and the odds ratio at 39.9 ng per millilitre [99.6 nmol per liter] was 0.53; P≤0.01). A prospective study of vitamin D intake and the risk of colorectal cancer in 1954 men showed a direct relationship (with a relative risk of 1.0 when vitamin D intake was 6 to 94IU per day and a relative risk of 0.53 when the intake was 233 to 652 IU per day, P<0.05) [4].
Children and young adults who are exposed to the most sunlight have a 40% reduced risk of non-Hodgkin’s lymphoma [5, 6] and a reduced risk of death from malignant melanoma once it develops, as compared with those who have the least exposure to sunlight. The maximum beneficial effect was observed for gastrointestinal cancer. Skinner et al. [7] reported 41 per cent lower risk of pancreatic cancer among subjects consuming >600 IU vitamin D daily in comparison to those with <150 IU per day. Similar inverse relation with vitamin D nutritional status was also reported for colorectal adenomas, endometrial and breast carcinoma. Besides, Hartman et al [8] reported 18 per cent lower recurrence of adenomatous polyps in ‘Polyp Prevention Trial’ among subjects on vitamin D supplementation.
Vitamin D and type 1 diabetes
Several studies suggest that vitamin D supplementation in children reduces the risk of type 1 diabetes. Increasing vitamin D intake during pregnancy reduces the development of islet auto antibodies in Offspring. For 10,366 children in Finland who were given 2000 IU of vitamin D3 per day during their first year of life and were followed for 31 years, the risk of type 1 diabetes was reduced by approximately 80% (relative risk, 0.22; 95% CI, 0.05 to 0.89).
Vitamin D and type 2 diabetes
Pittas et al. [9] also examined association between combined vitamin D and calcium intake and incidence of type 2 DM among 83,806 women in Nurses’ Health Study. Association between vitamin D intake and incidence of type 2 DM was examined in Women’s Health Subjects with daily vitamin D intake >511 IU had lower risk of incidence of DM when compared to a cohort with daily vitamin D intake of <159 IU per day (2.7% vs. 5.6%). In another study, vitamin D deficiency increased insulin resistance, decreased insulin production, and was associated with the metabolic syndrome.
Another study showed that a combined daily intake of 1200 mg of calcium and 800 IU of vitamin D lowered the risk of type 2 Diabetes by 33% (relative risk, 0.67; 95% CI, 0.49 to 0.90) as compared with a daily intake of less than 600 mg of calcium and less than 400 IU of vitamin D. improved b-cell function via direct effect of vitamin D or by increase in the intracellular ionized calcium which therefore would result in enhanced insulin release, increased insulin sensitivity related to expression of insulin receptor or via calcium dependent pathways in target cells leading to increase in the glucose utilization, and inhibition of b-cells apoptosis due to VDR transcription factor mediated inhibition of cytotoxic cytogene gene expression. While there is a possibility that widespread prevalence of type 2 DM observed in Asian Indians could be partially related to VDD, there are no data available among Indian subjects on VDD and its effect on beta cell function or insulin sensitivity.
Vitamin D and risk of hypertension, cardiovascular disease
In a study of patients with hypertension who were exposed to ultraviolet B radiation three times a week for 3 months, 25-hydroxyvitamin D levels increased by approximately 180%, and blood pressure became normal (both systolic and diastolic blood pressure reduced by 6 mm Hg). Vitamin D deficiency is associated with congestive heart failure and blood levels of inflammatory factors, including C-reactive protein and interleukin. The incidence of hypertension also followed an inverse relation with serum 25(OH) D and increased intake of vitamin D was associated with 9.3 per cent decrease in systolic blood pressure. Interventional studies had also shown up to 40 per cent fall in C-reactive protein (CRP) and interleukin-6 (inflammatory markers of CAD) at the end of one year in patients with CAD put on three monthly injections of 1250 µg cholecalciferol. Study by Watson et al. [10] reported inverse correlation of serum 1,25(OH)2D3 and presence of coronary artery calcification in subjects with hypercholesterolemia who are at high risk for CAD (Framingham cohort) and also in asymptomatic individuals from South way with moderate risk of CAD when followed up for four years. Circumstantial evidences also indicated an increase in the risk of CAD with increasing geographic latitude and associated fall in serum 25(OH) D. On the contrary, there was a decline in mortality from CAD for males in the New Mexico with higher altitudes. On an average, an increase of 1000 meter in the altitude of residence was associated with a 28 per cent decrease in mortality rates associated with CAD.
In addition, several studies also demonstrated increase in the coronary events and associated mortality (up to 40%) in winter season when compared to other seasons. Studies are shown that the seasonal variation of serum 25(OH) D levels with almost undetectable 25(OH) D levels in winter in Indians despite its sunny climate. Zitterman et al. [11] also suggested high prevalence of CAD in urban population when compared to the rural population could be due to VDD secondary to environmental pollution linked block in UV rays. Agarwal et al. [12] also reported environmental pollution and haze related fall in serum 25(OH) D in urban Delhi.
Lung Function and Wheezing Illnesses
Men and women with a 25-hydroxyvitamin D level above 35 ng per millilitre (87 nmol per litre) had better improvement. Recently, Nursyam et al. [13] carried out a placebo-controlled randomized trial of vitamin D supplementation (0.25 mg/day for initial 6 wk) in 67 patients with pulmonary tuberculosis. All the subjects in the vitamin D supplemented group and only 76.7 per cent in the placebo group had sputum conversion. In another randomized control trial, addition of vitamin D to standard anti tubercular therapy resulted in higher rate of clinical and radiological improvement. Davies [14] reported significantly lower levels of serum 25(OH) D in patients with untreated tuberculosis in comparison to healthy controls. In a similar study, Grange et al showed that patients with higher 25(OH) D levels had less extensive radiographic disease.
Conclusions
Vitamin D is not just a vitamin. Vitamin D deficiency is a preventable chronic disorder, in all age groups. It is very common in Indians when compared to west, even though enough exposure to the sun. VDD affects all age groups. 25 hydroxyl vitamin D is the barometer of vitamin D status in the body. There is enough evidence to show it reduces risk of cancer, TB, autoimmune disorders, diabetes etc. Vitamin D Fortification should be a national policy. Vitamin D is one of the life style markers, as of exercise.
Conflicts of interest
Author declares no conflicts of interest.
References
1. Shoben AB, Kestenbaum B, Levin G, Hoofnagle AN, Psaty BM. Seasonal variation in 25-hydroxyvitamin D concentrations in the cardiovascular health study. Am J Epidemiol. 2011, 174:1363-1372.
2. Holick MF, Chen TC, Lu Z, Sauter E. Vitamin D and skin physiology: a D-lightful story. J Bone Miner Res 2007, 2:V28-33.
3. Dawson-Hughes B, Harris SS, Palermo NJ, Ceglia L, Rasmussen H. Meal conditions affect the absorption of supplemental vitamin D(3) but not the plasma 25-hydroxyvitamin D response to supplementation. J Bone Miner Res 2013 doi: 10.1002/jbmr.1896.
4. Gorham ED, Garland CF, Garland FC, et al. Vitamin D and prevention of colorectal cancer. J Steroid Biochem Mol Biol 2005, 97:179-194.
5. Chang ET, Smedby KE, Hjalgrim H, et al. Family history of hematopoietic malignancy and risk of lymphoma. J Natl Cancer Inst 2005,97:1466-1474.
6. Garland CF, Garland FC, Gorham ED, et al. The role of vitamin D in cancer prevention. Am J Public Health 2006, 96:252-261.
7. Skinner HG, Michaud DS, Giovannucci E, Willett WC, Colditz GA, et al. Intake and the risk for pancreatic cancer in two cohort studies. Cancer Epidemiol Biomarkers Prev 2006, 15: 1688-1695.
8. Hartman TJ, Albert PS, Snyder K, Slattery ML, Caan B, et al. Polyp Prevention Study Group The association of calcium and vitamin D with risk of colorectal adenomas. J Nutr 2005, 135: 252-259.
9. Pittas AG, Dawson-Hughes B, Li T, Van Dam RM, Willett WC, et al. Vitamin D and calcium intake in relation to type 2 diabetes in women. Diabetes Care 2006, 29: 650-656.
10. Watson KE, Abroiat ML, Malone LL, Hoed JM, Doheerty T, et al. Active vitamin D levels are inversely correlated with coronary calcification. Circulation 1997, 96: 1755-1760.
11. Zittermann A, Schleithoff SS, Koefer R. Putting cardiovascular disease and vitamin D insufficiency into perspective. Br J Nutr 2005, 94: 483-492.
12. Agarwal KS, Mughal MZ, Upadhyay P, Berry JL, Mawer EB, et al. The impact of atmospheric pollution on vitamin D status of infants and toddlers in Delhi, India. Arch Dis Child 2002, 87: 111-123.
13. Nursyam EW, Amin Z, Rumende CM. The effect of vitamin D as supplementary treatment in patients with moderately advanced pulmonary tuberculous lesion. Acta Med Indones 2006, 38: 3-5.
14. Davies PD. The role of vitamin D in tuberculosis. Am Rev Respir Dis 1989, 139: 1571.