Full Text
Introduction
Functional endoscopic sinus surgery (FESS) is a minimally invasive procedure to restore sinus ventilation and normal function. These surgeries have drastically improved over time and are usually done under general anaesthesia. Laryngoscopy and tracheal intubation are an essential part of general anaesthesia to maintain airway and prevent aspiration. Intense sympathetic hemodynamic response to airway devices called the ‘pressor response’ is a dangerous condition in general anaesthesia [1].
It is associated with tachycardia and hypertension causing an imbalance in myocardial oxygen demand and supply which may lead to myocardial infarction and heart failure in few patients having other comorbidities [2]. Healthy adults can normally tolerate this sympathetic response but in patients having comorbidities it can be hazardous [3].
Hence pre-medications to attenuate the pressor response to intubation is very much necessary during general anaesthesia. The search for an ideal premedication drug has been going on since few decades but no single drug has been proven to be the drug of choice. Medications such as midazolam, barbiturates, alpha 2 agonists, opioids have been used by few authors to attenuate the hemodynamic response [4, 5].
Gamma-amino butyric acid (GABA) analogs pregabalin and gabapentin used as premedication drugs in various clinical studies have shown to be effective in alleviating perioperative pain and also in attenuating pressor response to intubation and in producing perioperative sedation and anxiolysis [6-13]. Oral pregabalin or oral gabapentin can been used to attenuate hemodynamic response associated with direct laryngoscopy and intubation [14].
The present study was designed to compare the premedication effects of oral gabapentin and oral pregabalin in patients undergoing FESS under general anaesthesia.
To compare the effects of oral gabapentin and oral pregabalin as a premedication for alleviating anxiety, to produce sedation and attenuate hemodynamic response to laryngoscopy and endotracheal intubation.
Materials and methods
This prospective, randomized study was undertaken in ENT operation theatre in Hassan Institute of Medical Sciences, Hassan, Karnataka between July 2020 and June 2021. Institutional Ethical Committee approval was taken. Written informed consent was obtained from 60 adult patients posted for elective FESS under general anaesthesia.
Inclusion criteria
Male and female patients who are posted for elective FESS, patients who are weighing between 40 and 70kg and aged between 20 to 60 years, patients with airway Mallampatti Grade I and Grade II only, patients with American Society of Anaesthesiologists (ASA) grade I and II only, patients undergoing orotracheal intubation only.
Exclusion criteria
Patients posted for other surgeries other than elective FESS, ASA Grade III or higher, anticipated difficult intubation, intubation other than orotracheal, cardiac, pulmonary or renal disease, patients on sedatives, hypnotics and analgesics for chronic pain, second attempt for intubation, duration of laryngoscopy exceeding 20 sec, pregnancy/ lactation.
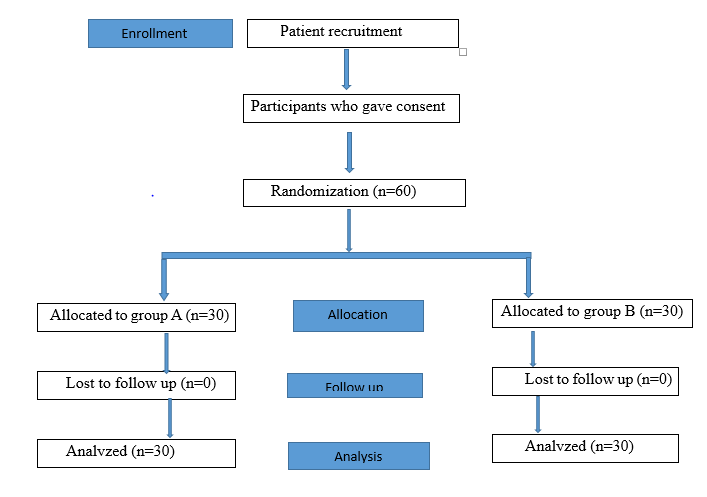
Figure 1: Consort diagram.
During the preoperative visit, based on inclusion and exclusion criteria, patients posted for elective FESS were selected for the present study. Patients were examined and appropriate investigations were done. Informed written consent was taken. 60 patients were randomly allocated into two groups of 30 each by computer generated random numbers.
In the pre-anaesthetic room, Group A received gabapentin 600 mg and Group B received pregabalin 150 mg orally with sips of water as premedication one hour prior to induction of general anaesthesia. Both group A and group B patients were not pre-medicated with any other sedative drugs before surgery. The observer Anaesthesiologist was unaware of the study drugs. In the pre anaesthetic room baseline heart rate, systolic, diastolic, mean arterial pressure, oxygen saturation and respiratory rate were recorded. Exactly one hour after taking the premedication drug, all patients were assessed for sedation using appropriate scoring systems and the scores were recorded. The pre-operative level of sedation was assessed by the Ramsay sedation scale [15] (Table 1).
Table 1: Ramsay sedation scale.
|
Scores
|
Sedation levels
|
|
1
|
Anxious, agitated or restless
|
|
2
|
Co-operative, oriented or restless
|
|
3
|
Responds to command
|
|
4
|
Asleep with brisk response to stimulus
|
|
5
|
Asleep with sluggish response to stimulus
|
|
6
|
Asleep with no response
|
Patients were then shifted to operating room by stretcher. In the operating room patient was connected to three lead ECG, non-invasive blood pressure cuff and arterial oxygen saturation probes.
An 18-gauge intravenous cannula was secured and intravenous fluids were started in all patients. In both A and B groups anaesthetic technique followed was same. They were premedicated intravenously with Inj. Ondansetron 0.1mg/kg, inj. glycopyrolate 10 µgm/kg, Inj. Fentanyl 2µgm/kg prior to induction followed by preoxygenation with 100% oxygen for 3min. Then the patients were induced with Inj. Propofol 2mg/kg. Intravenous inj. vecuronium 0.1mg/kg was used to paralyse the patients after which laryngoscopy and tracheal intubation was done by an anaesthesiologist who was blinded to the study protocol. Anaesthesia was maintained with 40% Oxygen, 60% nitrous oxide and Isoflurane 0.5 to 0.6% along with inj. vecuronium 0.02mg/kg. Following parameters were recorded-baseline heart rate (HR) and mean arterial pressure (MAP) before premedication, HR and MAP after premedication and after induction, HR and MAP at 0 min (during laryngoscopy), HR and MAP at 1 min, 3min, 5min and 10min after intubation.
Intravenous inj. neostigmine 0.05mg/kg and inj. glycopyrolate 0.01mg/kg was given at the end of the procedure and the patient was extubated. There was no respiratory depression in both the groups. No delay in recovery was noted in both the groups. All patients were extubated when fully awake and alert.
Statistical analysis
All the parameters recorded were entered in excel sheet. Statistical package for social sciences for windows (SPSS) version 19.0 was used for the analysis of the data. Microsoft word and Excel have been used to generate graphs, tables, etc. Data were represented as mean and standard deviation. Paired and unpaired student t-test was used to calculate the p value. P < 0.05 was considered statistically significant.
Results
Totally, 60 patients were included in the study. All the patients completed the study successfully. Both Groups A and B were comparable with respect to age, sex, weight and ASA (I and II). There were no significant differences in demographic profile among the two groups (>0.05) (Table 2).
Table 2: Demographic parameters.
|
Demographic parameters
|
Group A (n=30)
Mean ± SD
|
Group B (n=30)
Mean ± SD
|
p value
|
|
Age (Years)
|
34.5±7.5
|
35.5±7.20
|
0.6003
|
|
Sex (M:F)
|
20:10
|
19:11
|
>0.05
|
|
Weight (Kg)
|
56.5±5.2
|
58.2±5.5
|
0.22
|
|
ASA (I:II)
|
18:12
|
17:13
|
>0.05
|
Sedation was assessed using Ramsay sedation scale [15]. Sedation levels were recorded in both group A and group B patients. In group A, of total 30 patients, 16 patients had sedation score 2 and 14 patients had score 1. One hour after premedication with oral gabapentin 600mg, 15 patients had sedation score 3 and 15 patients had score 2. In group B, of total 30 patients, 13 patients had score 1, 17 patients had score 2. One hour after premedication with oral pregabalin 150 mg, 14 patients had score 2, 13 patients had score 3 and 3 patients had score 4 (Table 3).
In both group A and group B, sedation scores were on lower levels before premedication but one hour after premedication both the groups showed higher sedation scores. Higher levels of sedation were achieved in group B (p <0.0001) compared to group A (p 0.0052) (Table 3.1).
Table 3: Sedation score before induction.
|
Group A (n=30)
|
Group B (n=30)
|
|
Sedation score
|
Before premedication
|
1 hour after premedication
|
Sedation score
|
Before premedication
|
1 hour after premedication
|
|
1
|
14
|
0
|
1
|
13
|
0
|
|
2
|
16
|
15
|
2
|
17
|
14
|
|
3
|
0
|
15
|
3
|
0
|
13
|
|
4
|
0
|
0
|
4
|
0
|
03
|
|
5
|
0
|
0
|
5
|
0
|
0
|
|
6
|
0
|
0
|
6
|
0
|
0
|
Table 3.1: Comparison of sedation scores between Group A and Group B.
|
Groups
|
Sedation score (Mean ± SD)
|
P value
|
|
Before premedication
|
After premedication
|
|
Group A (n=30)
|
1.5±0.5
|
2±0.812
|
0.0052
|
|
Group B (n=30)
|
1.5±0.5
|
2.5±1.11
|
<0.0001
|
Both group A and group B did not show significant difference in baseline heart rate (HR) and mean arterial pressure (MAP) (p value >0.05). Both the groups did not show any significant difference in the HR and MAP, one hour after premedication and after induction. But during laryngoscopy (0 min) and at 1, 3 and 5 min after laryngoscopy and intubation, the HR and MAP increased in both the groups. But the attenuation of HR and MAP was significantly higher in group B compared to group A (p <0.01). After 5 min, the HR and MAP decreased in both the groups. And at 10 min, HR and MAP values almost reached the baseline values and no significant difference was noted in both the groups (p = 1.000) (Tables 4 and 5).
Table 4: Comparison of heart rate.
|
Heart rate
|
Group A
Mean ± SD
|
Group B
Mean ± SD
|
p value
|
|
Baseline
|
78.50±5.20
|
77.20±4.20
|
0.2912
|
|
After premedication
|
76.20±4.50
|
75.50±4.50
|
0.5492
|
|
After induction
|
80.20±5.0
|
78.20±5.20
|
0.1343
|
|
During laryngoscopy (0 min)
|
88.40±5.50
|
85.50±3.50
|
0.0179*
|
|
1 min
|
90.20±4.50
|
87.20±3.20
|
<0.01**
|
|
3 min
|
86.80±5.20
|
83.20±3.50
|
<0.01**
|
|
5 min
|
85.50±3.20
|
83.50±2.50
|
<0.01**
|
|
10 min
|
80.20±3.50
|
80.50±2.20
|
<0.69
|
Table 5: Comparison of mean arterial pressure (MAP).
|
MAP
|
Group A
Mean ± SD
|
Group B
Mean ± SD
|
p value
|
|
Baseline
|
90.30±3.70
|
90.20±3.50
|
0.9147
|
|
After premedication
|
88.80±2.74
|
88.50±2.70
|
0.6708
|
|
After induction
|
86.50±3.50
|
85.50±2.84
|
0.2
|
|
During laryngoscopy (0 min)
|
98.80±2.58
|
95.28±1.72
|
<0.01**
|
|
1 min
|
99.86±2.28
|
96.9±2.8
|
<0.01**
|
|
3 min
|
94.20±3.74
|
91.20±3.20
|
<0.01**
|
|
5 min
|
92.50±3.40
|
90.20±2.80
|
<0.01**
|
|
10 min
|
90.20±2.70
|
89.80±2.80
|
0.5754
|
Side effects such as nausea/vomiting, headache and dizziness occurred in few cases of both the groups. Incidence of nausea/vomiting was high in group A (6.6%) compared to group B (3.33%). Headache was also noted more in group A (10%) when compared to Group B (6.6%). The incidence of dizziness was same in both the groups (6.6%). All these side effects subsided without any treatment. No other side effects such as somnolence and blurred vision were reported in this study (Table 6).
Table 6: Comparison of side effects.
|
Side effects
|
Group A (n=30)
|
Group B (n=30)
|
|
Nausea/ Vomiting
|
2 (6.6%)
|
1 (3.33%)
|
|
Headache
|
3 (10%)
|
2 (6.6%)
|
|
Dizziness
|
2 (6.6%)
|
2 (6.6%)
|
|
Somnolence
|
-
|
-
|
|
Blurred vision
|
-
|
-
|
Discussion
Laryngoscopy and endotracheal intubation elicits reflex hemodynamic response due to stimulation of mechanoreceptors which are present over the pharyngeal wall, epiglottis, and vocal cord leading to sympathoadrenal activity [16, 17].
Intense sympathetic hemodynamic response to airway devices is a dangerous condition in general anaesthesia. Many different techniques were proposed to attenuate this hemodynamic responses such as deepening the plane of anaesthesia [18], premedication with drugs such as IV lignocaine [19], nitroglycerine [18], β blockers [20], calcium channel blockers [21] and opioids [22]. But no single technique was satisfactory.
GABA analogs such as pregabalin and gabapentin have shown effects like anxiolysis, sedation, attenuation of hemodynamic responses to laryngoscopy and intubation in various clinical studies [23, 24]. Gabapentin is a structural analogue of neurotransmitter GABA. It acts by selective activation of GABA-B receptors and enhancement of NMDA receptors thus producing the desired pharmacological actions [25].
Pregabalin is also structurally related to GABA but inactivates GABA receptors. It acts by decreasing the synthesis of neurotransmitter glutamate. It acts as an analgesic, anxiolytic, anticonvulsant, and maintains hemodynamic stability throughout perioperative period [26]. Oral bioavailability of pregabalin (90%) is more than that of gabapentin (60%) [27].
The present study is undertaken to compare the effects of oral gabapentin and oral pregabalin as a premedication for alleviating anxiety, to produce sedation and attenuate hemodynamic response to laryngoscopy and endotracheal intubation in patients receiving general anaesthesia. To make the study population more similar we included the patients undergoing only elective FESS in the study. 60 patients were chosen based on the inclusion and exclusion criteria. Patients were divided into two groups, Group A received oral gabapentin 600mg and Group B received oral pregabalin 150 mg as premedication. Sedation, attenuation of HR and MAP produced by both the groups were compared.
Pre-operative level of sedation was assessed using Ramsay sedation scale [15] in which there are a total of 6 scores based on the sedation level of patients. Score 1 is the minimum, given to patients who are anxious, agitated or restless and score 6 is the maximum in which patients will be asleep with no response (Table 1).
Sedation levels were recorded in both group A and group B patients. In group A, of total 30 patients, 16 patients had sedation score 2 and 14 patients had score 1. One hour after premedication with oral gabapentin 600mg, 15 patients had sedation score 3 and 15 patients had score 2. In group B, of total 30 patients, 13 patients had score 1, 17 patients had score 2. 1 hour after premedication with oral pregabalin 150 mg, 14 patients had score 2, 13 patients had score 3 and 3 patients had score 4 (Table 3).
In both group A and group B, sedation scores were on lower levels before premedication but one hour after premedication both the groups showed higher sedation scores. On comparing, higher levels of sedation were achieved in group B compared to group A (Table 3 and 3.1).
Anju et al. [28] used higher dose of pregabalin 300mg and gabapentin 900 mg and compared them for producing preoperative sedation. They concluded that pregabalin significantly produce more sedation which is similar to our study.
Baseline heart rate (HR) and mean arterial pressure (MAP) were recorded in both groups and then HR and MAP were again recorded one hour after premedication, after induction, during laryngoscopy (0 min) and at 1min, 3min and 5 min after laryngoscopy and intubation.
Both group A and group B did not show significant difference in baseline HR and MAP (p value >0.05). There was no significant difference in the HR and MAP, 1 hour after premedication and after induction in both the groups. But during Laryngoscopy (0 min) and at 1, 3 and 5 min after laryngoscopy and intubation, the HR and MAP increased in both the groups. But the attenuation of HR and MAP was significantly higher in group B compared to group A (p <0.01). After 5 min, the HR and MAP decreased in both the groups. And at 10 min, HR and MAP values almost reached the baseline values and no significant difference was noted in both the groups (p value >0.05) (Table 4 and 5).
Though the attenuation of HR and MAP were noted in both groups, group B showed higher level of attenuation compared to group A (p <0.01) (Table 4 and 5) (Graph 1 and 2). Similarly, Namratha et al. [13] compared gabapentin (800mg) and pregabalin (150mg) as premedication for attenuation of pressure response, in which pregabalin proved to be more effective than gabapentin both for heart rate and mean arterial pressure response, which is similar to the result obtained in the present study.
Rastogi et al. [6] also stated in their study that oral 150 mg of pregabalin significantly attenuate hemodynamic response to orotracheal intubation. Salman et al. [29] compared oral placebo and oral pregabalin 150 mg and found oral pregabalin to significantly lower HR and MAP compared to placebo group.
The effect of pregabalin on hemodynamic response to laryngoscopy and intubation may be explained by its inhibitory effects on membrane voltage gated calcium channels. Pregabalin binds potently and selectively to alpha 2 delta subunit of hyperexcited voltage gated calcium channels and inhibits the release of several neurotransmitters such as glutamate, noradrenaline, and substance P [29]. It does not interact with GABA receptors.
Studies done in the past have compared the effects of oral gabapentin and oral pregabalin as a premedication in the attenuation of hemodynamic response, but these studies were not narrowed to a specific surgical procedure [6, 13, 28, 29]. In the present study we have included only the patients undergoing FESS and compared the premedication effects of oral gabapentin and pregabalin. As head and neck surgeries have high risk of bleeding choosing a better premedication drug becomes very crucial.
Limitations of the study
Anxiety was not assessed in the present study, sample size studied was less, though the laryngoscopy duration was restricted to less than 20s, the exact duration of laryngoscopy was not measured.
Conclusion
Premedication with both oral pregabalin 150mg and oral gabapentin 600mg, given one hour before general anaesthesia in patients undergoing FESS produce sedation and attenuate hemodynamic response to laryngoscopy and intubation. But premedication with oral pregabalin 150 mg is more effective than oral gabapentin 600 mg in producing sedation and attenuating the hemodynamic responses to laryngoscopy and intubation.
Conflicts of interest
Author declares no conflicts of interest.
References
[1] Roberts P, Green C, Meloche LT, Foes R. Studies of Anaesthesia in relation to hypertension II, Hemodynamic consequences of induction and endotracheal intubation. Br J Anaesth. 1971; 43(6):531–547.
[2] Reid LC, Brace DE. Irritation of the respiratory tract and its reflex effect upon heart. Surg Gynaec & Obst. 1940; 70:157–162.
[3] Kovac AL. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. J Clin Anesth. 1996; 8(1):63–79.
[4] Korpien R, Sarnivaara L, Siren K, Sarna S. Modification of the haemodyamic responses to induction of anaesthesia and tracheal intubation with alfentanil, esmolol and their combination. Can J Anaesth. 1995; 42(4):298–304.
[5] Helfman SM, Gold MI, DeLisser EA, Herrington CA. Which drug prevents tachycardia and hypertension associated with tracheal intubation: lidocaine, fentanyl, or esmolol? Anesth Analg. 1991; 72(4):482–486.
[6] Rastogi B, Gupta K, Gupta PK, Agarwal S, Jain M, et al. Oral pregabalin premedication for attenuation of haemodynamic pressor response of airway instrumentation during general anaesthesia: A dose response study. Indian J Anaesth. 2012; 56(1):49–54.
[7] Paul W, Tufanogullari F, Taylor J, Klein K. The effect of pregabalin on preoperative anxiety and sedation levels: A dose ranging study. Anesth Analg. 2009; 108(4):1140–1145.
[8] Sundar AS, Kodali RK, Sulaiman S. The effect of preemptive Pregabalin on attenuation of stress response to endotracheal intubation and opioid sparing effect in patient undergiong off pump coronary artery bypass grafting. Annals of Cardiac Anaesthesia. 2012; 15(1):18–25.
[9] Gupta K, Bansal P, Gupta PK, Singh YP. Pregabalin premedication - A new treatment option for hemodynamic stability during general anaesthesia. Anesthesia Essays and researches. 2011; 5(1):57–62.
[10] Salman E, Celik C, Candan S. Premedication with single dose pregabalin 150mg Attenuates Hemodynamic Response to laryngoscopy and intubation. Research Article, June 07, 2012.
[11] Eren, Kozanhan B, Hergunsel O. Pregabalin blunts cardiovascular response to laryngoscopy and tracheal intubation. Turkiye Klinikleri J Anest Reanim. 2009; 7(2):82–87.
[12] Raichurkar A, Dinesh K, Ravi M, Anand T, Somasekharam P. A comparative study of oral pregabalin and clonidine for attenuation of hemodynamic responses to laryngoscopy and tracheal intubation. J Clin Biomed Sci. 2015; 5(1):25–29.
[13] Namratha S, Shobha D. Comparative evaluation of oral gabapentin and pregabalin premedication for attenuation of pressor response to endotracheal intubation under general anaesthesia IJSR. General Anaesthesia IJSR. 2014; 3(11):654–658.
[14] Singhal SK, Kaur K, Arora P. Oral clonidine versus gabapentin as premedicant for obtunding hemodynamic response to laryngoscopy and tracheal intubation. Saudi J Anaesth [Internet]. 2014; 8(2):172–177.
[15] Stawicki SP. Mechanical ventilation: Weaning and extubation. OPUS 12 Scientist. 2007 1(2):13–16.
[16] Thomson IR. The haemodynamic response to intubation: a perspective. Can J Anaesth. 1989; 36(4):367–369.
[17] Fox EJ, Sklar GS, Hill CH, Villanueva R, King BD. Complications related to the pressure response to endotracheal intubation. Anaesthesiology. 1977; 47(6):524–525.
[18] Fassoulaki A, Kaniaris P. Intranasal administration of nitroglycerine attenuates the pressor response to laryngoscopy and intubation of the trachea. Br J Anaesth. 1983; 55(1):49–52.
[19] Vucevic M, Purdy GM, Ellis FR. Esmolol hydrochloride for management of the cardiovascular stress responses to laryngoscopy and tracheal intubation. Br J Anaesth. 1992; 68(5):529–530.
[20] Mikawa K, Ikegaki J, Maekawa N, Goto R, Kaetsu H, et al. The effect of diltiazem on the cardiovascular response to tracheal intubation. Obstet Anesth Dig. 1990; 10(3):139.
[21] Miller DR, Martineau RJ, O’Brien H, Hull KA, Oliveras L, et al. Effects of alfentanil on the hemodynamic and catecholamine response to tracheal intubation. Anesth Analg. 1993; 76(5):1040–1046.
[22] Abou-Madi MN, Keszler H, Yacoub JM. Cardiovascular reactions to laryngoscopy and tracheal intubation following small and large intravenous doses of lidocaine. Can Anaesth Soc J. 1977; 24(1):12–19.
[23] Lauria-Horner BA, Pohl RB. Pregabalin: a new anxiolytic. Expert Opin Investig Drugs. 2003; 12(4):663–672.
[24] Ménigaux C, Adam F, Guignard B, Sessler DI, Chauvin M. Preoperative gabapentin decreases anxiety and improves early functional recovery from knee surgery. Anesth Analg. 2005; 100(5):1394–1399.
[25] Rose MA, Kam PCA. Gabapentin: pharmacology and its use in pain management: Gabapentin. Anaesthesia. 2002; 57(5):451–462.
[26] Kavoussi RC. Pregabalin: From molecule to medicine. Eur Neuropsychopharmacol. 2004; 14:S413.
[27] Nutt D, Mandel F, Baldinetti F. Early onset anxiolytic efficacy after a single dose of pregabalin: double-blind, placebo- and active-comparator controlled evaluation using a dental anxiety model. J Psychopharmacol. 2009; 23(8):867–873.
[28] Anju G, Gupta M, Rana N, Wadhera R. The effect of pregabalin and gabapentin on preoperative anxiety and sedation: A double blind study. Anaesth Pain Intensive Care. 2012; 16(3):257–261.
[29] Salman E, Celik C, Candan S. Premedication with single dose pregabalin 150 mg attenuates hemodynamic response to laryngoscopy and endotracheal intubation. Open Access Scientific Reports; 2012; 47:34–41.