Case Report
2019
December
Volume : 7
Issue : 4
Role of plasmapheresis in neuromyelitis optica spectrum disorders
Pranathi B, Nashrah Nooreen, Madhuri Gadde, Anitha Videkar
Pdf Page Numbers :- 115-119
Pranathi B1,*, Nashrah Nooreen1, Madhuri Gadde1 and Anitha Videkar1
1Department of Ophthalmology, Krishna Institute of Medical Sciences (KIMS), Secunderabad-500003, Telangana, India
*Correspondence: Dr. B. Pranathi, Senior consultant and Head of Department, Department of Ophthalmology, Krishna Institute of Medical Sciences (KIMS), Secunderabad-500003, Telangana, India. Tel.: 040-44885050; Email: bejugum.pranathi@gmail.com
Received 20 July 2019; Revised 30 August 2019; Accepted 11 September 2019; Published 19 September 2019
Citation: Pranathi B, Nooreen N, Gadde M, Videkar A. Role of plasmapheresis in neuromyelitis optica spectrum disorders. J Med Sci Res. 2019; 7(4):115-119. DOI: http://dx.doi.org/10.17727/JMSR.2019/7-20
Copyright: © 2019 Pranathi B et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: We report a case of Neuromyelitis optica spectrum disorder (NMOSD) which has failed to respond to the first line treatment i.e. IV methylprednisolone and had responded well to the plasmapheresis.
Method: A 23-year-old female presented with complaint of sudden painless diminution of vision in both eyes which is progressive in nature associated with severe headache, with no systemic symptoms, since 10 days. On examination patient denied perception to light in both eyes. On anterior segment examination both the pupil were 6mm dilated, ill sustained and sluggishly reacting to light, rest anterior segment was normal. Fundus examination of both eyes showed hyperemic pallid disc edema with blurring of margins all around associated with tortuous vessels with foveal reflux present. We started her on IV methyl prednisolone for 3 days but did not respond, then we switched to plasmapheresis.
Results: After 2nd cycles of plasmapheresis the vision improved to hand movement in both eyes and after 7thcycle the vision improved to counting fingers at 4meters. And the patient was maintained on tapering dose of steroids (50mg/day) and azathioprine 100mg/day (2-3 mg/kg/day) was started.
Conclusions: Plasmapheresis is an effective therapy in NMOSD patients and should be considered if the patient fails to respond to the initial therapy.
Keywords: Neuromyelitis optica; painless progressive diminision of vision; sluggishly reacting pupil; hyperemic pallid disc; methylprednisolone; plasmapheresis
Full Text
Introduction
Neuromyelitis optica is an autoimmune CNS demyelinating disease with a defined autoantibody to aquaporin 4 on the surface of astrocyte [1, 2]. Neuromyelitis optica (NMO) historically been considered a rare disease that selectively affects the optic nerve and spinal cord. The prevalence of NMO has increased yearly since the worldwide availability of AQP4 antibody testing [3]. Moreover NMO appears to be multiorgan disorder that is comorbid with other systemic autoimmune disease [4].
The diagnostic criteria were revised and published in the Integrated Public Number Database (IPND) 2015 [5]. The tests included in diagnostic criteria are visual evoked potential which classically shows prolonges latency, laboratory findings shows AQP4IgGs, APQ1-IgG and myelin oligodendrocyte glycoprotein and cerebrospinal fluid (CSF) examination reveals pleocytosis, protein loss, loss of oligoclonal IgG bands.
NMO relapses tend to be more severe than multiple sclerosis (MS. Disability care load is positively correlated with number of relapses. Relapses can be prevented with immunosuppressants such as azathioprine and mycophenolate. However acute phase and relapse treatment should be considered the foremost step in recovery.
The treatment tree for NMO, in acute attack (first episode or relapse) we start with IV methylprednisolone 1gm/day for 3-5 days and then tapering dose of oral steroids and in steroid non-responders we start with the plasmapheresis. Maintenance therapy for these patients would include immunosuppressive therapy including rituximab, mycophenolate mofetil, azathioprine, mitoxantrone, methotrexate, cyclophosphamide. Novel therapies includes human monoclonal anti bodies like tocilizumab, eculizumab, aquaporumab (Figure 1). To conclude acute neuromyelitis optica is treated with methyl prednisolone and resistant cases with plasmapheresis [6].

Figure 1: Treatment tree for neuromyelitis optica spectrum disorder patients.
Case report 23-year-old female presented with complaint of sudden painless diminution of vision in both eyes which is progressive in nature associated with severe headache, with no systemic symptoms, since 10 days.
At presentation patient denied perception to light in both eyes. On slit lamp biomicroscopy examination both eyes pupil was 6mm dilated, ill sustained and sluggishly reacting to light, rest anterior segment was normal. Fundus examination of both eyes showed hyperemic pallid disc edema with blurring of margins all around associated with tortuous vessels with foveal reflux present, which is shown below in fundus photo of right eye (Figure 2a) and the fundus photo of left eye (Figure 2b).
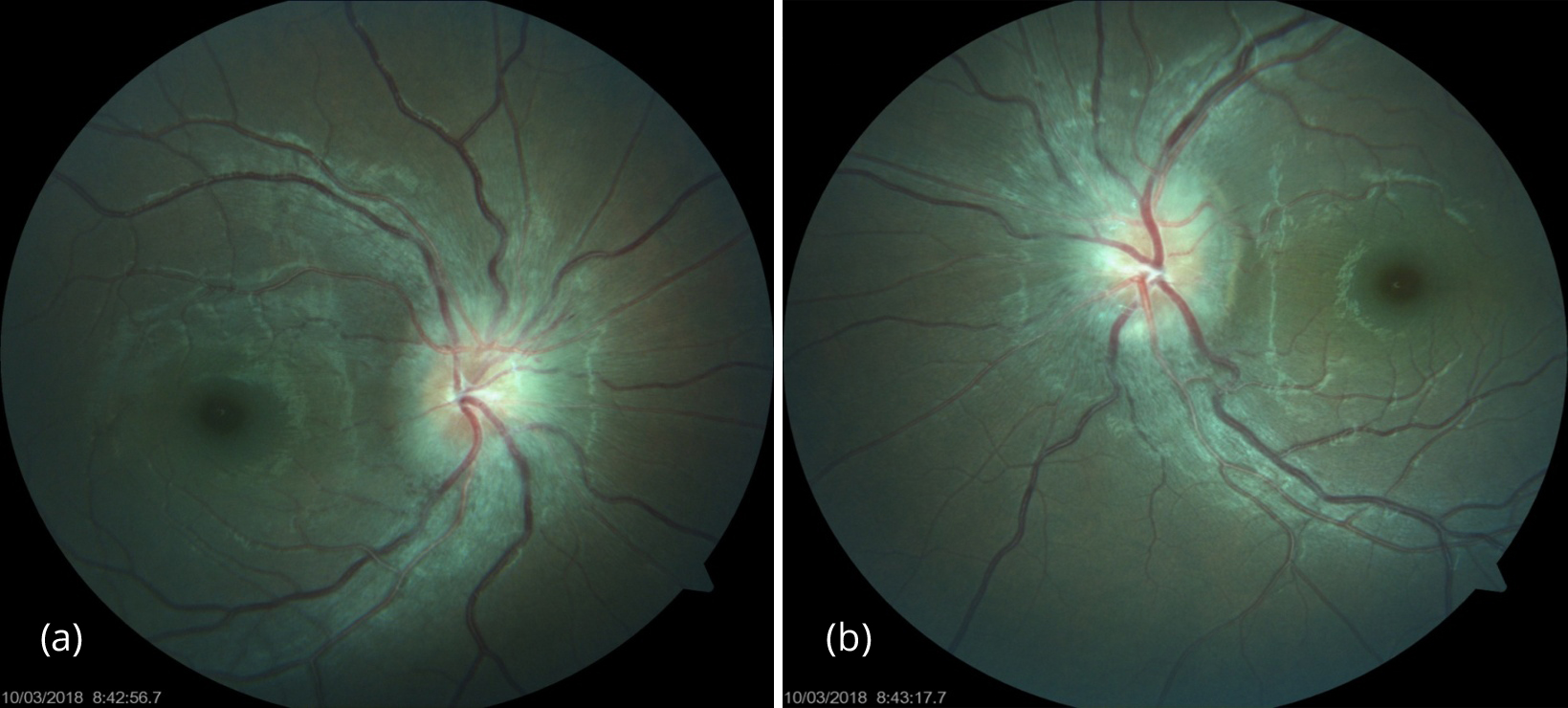
Figure 2: (a) Right eye fundus photo. (b) Left eye fundus photo.
Optical coherence tomography (OCT) also reveals the same, that is disc edema of about 766 microns in right eye (Figure 3a) and about 690microns in left eye (Figure 3b). Humphrey visual fields (HVF) reveals right visual field showing few depressed points superonasally and inferonasally and inferotemporally (Figure 4a) and left visual field showing depressed points inferonasally and inferotemporaly following the horizontal meridine (Figure 4b).

Figure 3: (a) Right eye optical coherence tomography. (b) Left eye optical coherence tomography.
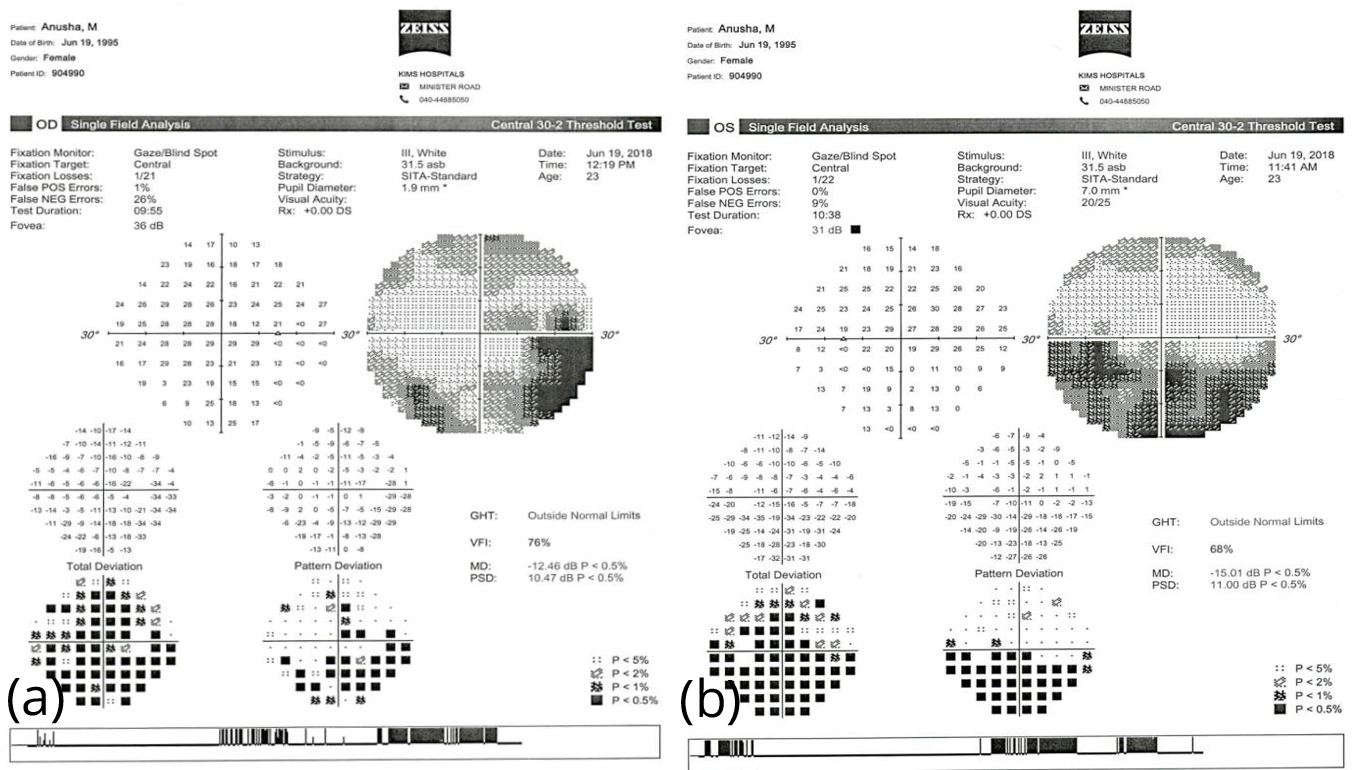
Figure 4: (a) Right eye Humphrey visual fields. (b) Left eye Humphrey visual fields.
Neurological evaluation was done with visual evoked potential showing extinguished responses bilaterally, magnetic resonance potential of brain was suggestive of bilateral optic neuritis but the cerebrospinal fluid analysis was normal and serum antibody titres of NMO IgG, AQP4IgG and MOG titres were negative.
Patient was started on intravenous methylprednisolone 1gm/day for 3 days but with no improvement so the plasmapheresis was initiated and by the end of 2nd cycle - vision improved to hand movement and by end of 7th cycle - vision improved to counting fingers 4m. Maintained on tapering doses of oral steroids (50mg/day) and azathioprine 100mg/day (2-3mg/kg/day) was started.
One month post treatment the BCVA (best corrected visual acuity) has improved to 6/9, N6 in both eyes, color vision has improved to 1/17 in both eyes, with pupil being 6mm and ill sustained. Fundus photo one month post treatment shows significantly decreased disc edema in right eye (Figure 5a) and in left eye (Figure 5b), OCT of the same also reveal resolving disc edema of about 300 microns in the right eye (Figure 6a) and the left eye (Figure 6b).

Figure 5: (a) Right eye Fundus photo one month post treatment. (b) Left eye Fundus photo one month post treatment.
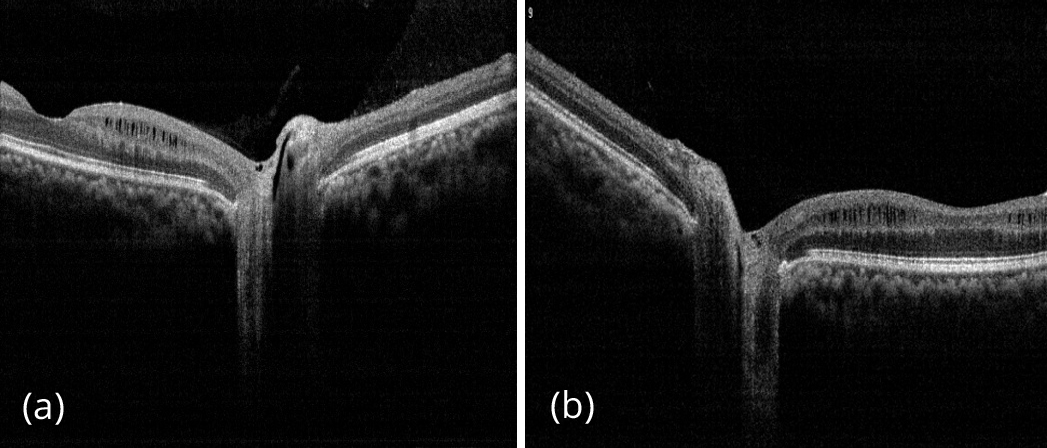
Figure 6: (a) Right eye OCT one month post treatment. (b) Left eye OCT one month post treatment.
Discussion
Plasmapheresis is an effective therapy for NMOSD attacks in patient who have not responded to initial intravenous corticosteroid/ intravenous immunoglobulin treatment, with an overall response rate of 50-100%. Patient who were nonresponsive to first line therapy the efficacy of plasmapheresis depended on the time of initial immunotherapy to plasmapheresis that is the sooner the plasmapheresis was implemented the greater the recovery. Therefore plasmapheresis should be considered as soon as possible in patients with NMOSD that are refractory to initially Intravenous corticosteroid/Intravenous immunoglobulin therapy and patients with severe NMOSD relapse. According to the previous literature expanded disability status scale (EDSS) score was slightly lower if plasmapheresis was administered within 15 days but not significantly higher than that when it was administered between 16-30 days. Patient later than 30 days was still beneficial to a few patients without an increased prevalence of adverse effects.
Kessler RA et al. [7] study has discussed the same that the disability in NMOSD results from accumulating damage in the CNS related to individual relapses over the course of the disease. Therefore, acute interventions designed to reduce damage may preserve long-term neurologic function. RA Kessler and Wingerchuk DM [8] in there study has concluded the same i.e. The treatment for NMOSD should begin typical with starting dose for treatment of NMOSD is 1000 mg of methylprednisolone intravenously for 5 days, commonly followed by an oral steroid taper for 2–8 weeks depending on the severity of the attack. Equivalent doses of other corticosteroids are likely equally effective as are other routes of administration given that bioavailability of intravenous versus oral corticosteroids are approximately the same. The initial goal for corticosteroid use in acute NMOSD relapses is to reduce the edema and secondary inflammation in the lesion. This may have the immediate effect of mild to modest improvement in neurological function. For long lesions or severely inflamed attacks, additional steroid doses may be indicated.
If there is minimal or no improvement with high-dose corticosteroids based on the judgment of the treating physician, the use of plasma exchange (PLEX) has been shown to be effective in NMOSD [8, 9]. The most frequent treatment approach for relapses of NMOSD comprises a schedule of high-dose steroids similar to that adopted in MS, but steroids are only partially effective. Their benefit is most apparent in blunting the extent and severity of the inflammatory response; in fact, only one-third of the patients with NMOSD revert to their previous neurologic status without additional interventions. Escalation to plasmapheresis after steroids in NMOSD relapses leads to a return to baseline in up to two-thirds of the patients. High-dose IVMP provides only a moderate degree of neurologic recovery from acute NMO relapses. Adding plasma exchange to high-dose IVMP improves the outcome at discharge and on follow-up in cases where IVMP alone is insufficient [10].
Conclusions
The diagnosis and treatment in NMOSD and “myelin-oligodendrocyte-glycoprotein-encephalomyelitis” (MOG-EM) require special clinical expertise. The 2015 NMOSD diagnostic criteria and the availability of antibody testing and MRI are the basis to diagnose and differentiate NMOSD or MOG-EM. Early diagnosis and initiation of adequate therapy are essential (steroids followed by PLEX)—at least in seropositive patients–to avoid disease attacks and persistent deficits. Plasmapheresis is an effective therapy in patients with NMOSD and should be considered as a treatment of NMOSD attack if the patient fails to respond to initial therapy or have a severe relapse. Long term immunosuppressive treatment, e.g., with RTX or AZA, has emerged to be the most effective therapies to reduce disease activity. Further therapeutic options, in particular various monoclonal antibodies are currently under clinical investigation in NMOSD.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, et al, A serum autoantibody marker of neuromyelitis optica:distinction from multiple sclerosis. Lancet 2004; 364 (9451):2106–2112.
[2] Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker of optic-spinal multiple sclerosis binds to aquaporin-4 water channel. J Exp Med. 2005; 202(4):437–477.
[3] Zhang W, Jiao Y, Cui L, Liu L, Zhang L, et al. Etiological,clinical,and radiological features of longitudinal extensive myelopathy in Chinese patients. J Clin Neurosci. 2016; 32:61–66.
[4] Wingerchuk DM,Weinshenker BG. The emerging relationship between neuromyelitis optica and systemic rheumatologic autoimmune disease. Mult Scler. 2012; 18(1):5–10.
[5] Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorder. Neurology 2015; 85(2):177–189.
[6] Collongues N, de Seze J. Current and future treatment approachs for neuromyelitis optica. The Adv anaeurol Disord. 2011; 4(2):111-121.
[7] Levy M. Plasmapheresis for acute attack in neuromyelitis optica spectrum disorders. Neurol Neuroimmunol Neuroinflamm. 2018; 5(6):e510.
[8] Kessler RA, Mealy MA, Levy M. Treatment of neuromyelitis optica spectrum disorder: acute, preventive, and symptomatic. Curr Treat Options Neurol. 2016; 18(1):2.
[9] Wingerchuk DM, Pittock SJ, Lucchinetti CF, Lennon VA, Weinshenker BG. A secondary progressive clinical course is uncommon in neuromyelitis optica. Neurology 2007; 68(8):603–605.
[10] Abboud H, Petrak A, Mealy M, Sasidharan S, Siddique L, et al. Treatment of acute relapses in neuromyelitis optica: steroids alone versus steroids plus plasma exchange. Mult Scler. 2016; 22(2):185–192.