Case Report
2015
September
Volume : 3
Issue : 3
Apathetic thyrotoxicosis
Srinivas V, Sravan Kumar S
Pdf Page Numbers :- 137-140
Srinivas V1,* and Sravan Kumar S1
1Department of Internal Medicine, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India
*Corresponding author: Dr. Srinivas V, MD., Senior Consultant Internal Medicine, Department of Internal Medicine, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India. Tel.: 040 44186767; Email: sri_vut@yahoo.co.in.
Received 13 April 2015; Revised 9 June 2015; Accepted 19 June 2015; Published 26 June 2015
Citation: Srinivas V, Sravan Kumar S. Apathetic thyrotoxicosis. J Med Sci Res. 2015; 3(3):137-140. DOI: http://dx.doi.org/10.17727/JMSR.2015/3-027
Copyright: © 2015 Srinivas V, et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
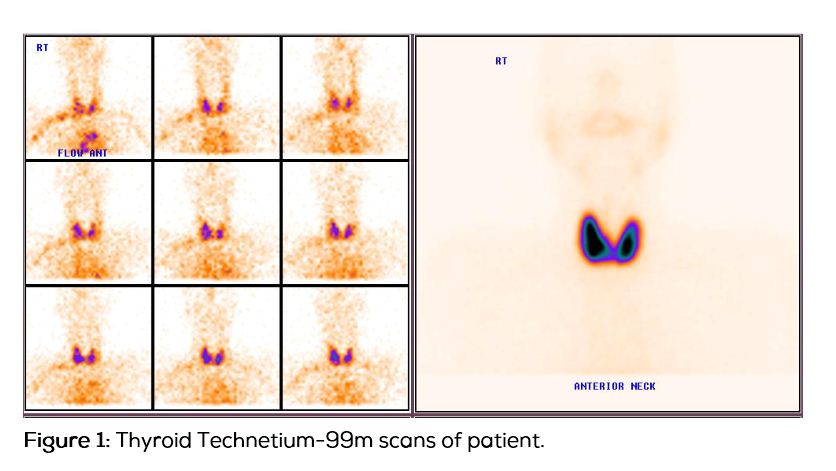
A 66-year-old male patient presented to the hospital with the complaints of weakness, loss of weight of about 10 kg in 2 months, decreased appetite, increased frequency of urination, not associated with burning sensation or hematuria. There was no history of fever or cough, altered bowel habits, or diabetes mellitus. Patient was suspected to harbour malignancy, underwent upper gastrointestinal endoscopy (UGI), high resolution computed tomography (HRCT) chest in an outside hospital which were normal. Patient came to this hospital for CT scan of abdomen. Patient was examined thoroughly and the clinically positive findings were, generalised wasting, tremors in the hands, heart rate 110 per min which led to investigate in lines of thyrotoxicosis. Thyroid stimulating hormone (TSH) was 0.01 free T3 was high and all other investigations normal. Random blood Sugar 115mg %, prostate-specific antigen 2.5ng/ml. patient underwent tc99 scan which was suggestive of were Graves’ disease. Endocrinology department has taken the patient and started on neomercazole, proponolol and discharged.
Keywords: apathetic thyrotoxicosis; hyperthyroidism; weight loss; thyroid hormone
Full Text
In 1931 Lahey [1] described a form of hyperthyroidism in which the patients appeared apathetic to their surroundings. These patients were withdrawn and listless and had immobile facies and dulled eyes. They seemed to exhibit few, if any, signs of classic hyperkinetic hyperthyroidism. Their condition was more like that of patients with hypothyroidism. These patients were diagnosed apathetic hyperthyroidism. Masked hyperthyroidism is the diagnostic descriptor of a patient in whom the classic signs and symptoms of hyperthyroidism are overshadowed by those classically due to other problems, such as cardiac or gastrointestinal diseases [2]. Monosymptomatic hyperthyroidism is the description used when all symptoms of hyperthyroidism are referred to one organ system. In masked and monosymptomatic varieties it is possible that the symptoms and signs of hyperthyroidism are too subtle to be recognized. Estimates of the frequency of apathetic or masked or monosymptomatic varieties of hyperthyroidism are about 5 percent or less [8]. In this case report, the patient was an elderly man, who experienced his usual state of health except for unexplained weight loss. This unusual expression should reinforce that hyperthyroidism can be difficult for family physicians to diagnose clinically and that a high index of suspicion must be maintained, to diagnose properly, this easily treated problem.
Case report
A 66-year-old male patient presented to the hospital with complaints of weakness, loss of weight of about 10 kgs in two months, listlessness and lethargy. Other causes for weight loss were ruled out and upper GI endoscopy, CT scan chest were done and both were normal. Ultrasound abdomen was normal, stool for occult blood, serum PSA, virology was negative. He had been unable to walk because of extreme weakness. Patient also gives history of polyuria, nocturia not associated with fever, or hematuria. There was no history of cough, or altered bowel habits. Patient was admitted in an outside hospital where he was suspected to have malignancy. CT scan abdomen was advised which the patient denied and came to this hospital. He was examined thoroughly. There was generalised wasting of shoulder, pelvic girdle muscles and small muscles of the hand. General examination revealed pr 110 /min BP 124/70, CBP was within normal limits, RBS 115mg%, PSA was 2.5ng/ml. USG abdomen was normal. ECG showed sinus tachycardia. Thyroid function tests were ordered because of tachycardia weight loss, tremors. The TSH was 0.01 microiu/ml, free T3 22.16pmol/ml, free T4 68.73pmol/ml, there was no thyroid swelling, no eye signs, no altered bowel habits. Thyrotoxicosis was confirmed, endocrinology consultation was taken, Technetium-99m scan (Figure 1) was ordered and it was suggestive of Graves’ disease, rest all other investigations LFT Rft CBP, cue viral screening all were normal. Patient was found to have hypovitaminosis D. patient was put on neomercazole. Propranolol was started and patient was discharged in a stable condition.
Discussion
Apathetic thyrotoxicosis, as a distinct entity was first described by Lahey [3] and subsequently by others [4, 5]. The salient features of apathy and depression are associated with profound weight loss, proximal and distal muscle weakness and wasting, ptosis, dry skin, mild tachycardia and often congestive cardiac failure. Absence of hyperkinetic motor activity, hand tremor and ocular signs, typical of Graves' disease is noteworthy. The thyroid gland if palpable is minimally enlarged. This absence of the typical signs and symptoms of thyrotoxicosis may cause the diagnosis to be missed. It is important to emphasize this point, because these patients under usual conditions do not appear extremely ill but under stress may quietly and peacefully sink into coma and die an absolutely relaxed death without activation, unlike the classic thyrotoxic patient who goes into crisis. Thus the disease may remain atypical throughout its course. Once this condition is suspected thyroid function tests will confirm the diagnosis [6].
If apathetic thyrotoxicosis is strongly suspected clinically but conventional thyroid function test results are normal, the physician should insist on radioimmunoassay which readily confirms the diagnosis.
The pathogenetic events leading to a state of apathy and depression in these patients are not known. A widely held hypothesis is that in depression there is a deficiency of brain biogenic amines, primarily the catecholamines noradrenalin and dopamine [7]. In thyrotoxicosis there is a decrease in circulating catecholamines8. Insidious onset and delay in diagnosis of apathetic thyrotoxicosis may allow depletion of body stores of noradrenalin. Another possibility is unresponsiveness to catecholamines at the receptor level, which explains the ptosis noted in these patients. However, a paradoxic improvement has been observed with adrenergic blockade in patients with apathetic crisis, though the ptosis remained unaffected.
In general there is lack of precise knowledge of the effect of thyroid hormones on the central nervous system. Recent evidence indicates that thyrotropin-releasing hormone (TRH) has an immediate therapeutic antidepressant effect when administered to severely depressed euthyroid patients [9].
Studies indicate that TRH potentiates behavioural effects of levodopa and pargyline in mice and is equally active in hypophysectomized and intact animals, thus excluding a role for either TSH or thyroid hormones [9]. TRH may have a direct effect on the brain in alleviating depression either by increasing dopaminergic receptor sensitivity or altering the metabolism of dopa in such a way so as to increase the concentration of active dopamine in the brain. Only when methodology is sufficiently improved to permit measurement of circulating TRH and to detect abnormal reduction in blood levels it will be possible to know whether there is undue depletion of TRH in apathetic hyperthyroid patients. However, whether it is depletion of TRH or catecholamines, or unresponsiveness to the latter, that is implicated in the pathogenesis of mental apathy and depression in susceptible patients is speculative at this stage. The three patients described had all the features of apathetic thyrotoxicosis but in the absence of typical signs and symptoms of thyroid overactivity the diagnosis was initially missed. We would like to emphasize that ptosis may be a valuable clue to the correct diagnosis. There was no subjective improvement in the patients' apathy or depression immediately or over the ensuing 24 hours after an intravenous bolus injection of 200 ug of TRH, the opposite of the beneficial response observed in euthyroid depressed patients. Furthermore, the TSH response to TRH in these patients was similar to that obtained in Graves' disease. Its presence in 3 out of 20 patients hospitalized with thyrotoxicosis over a 12-month period would suggest that apathetic thyrotoxicosis is more common than is generally believed. Because this condition if untreated may be fatal, and if recognized responds gratifyingly to treatment, it is important that the physician should be alert to the possibility of its presence in a depressed patient with the other signs displayed similar to those in the above 3 cases.
Conclusion
In this case report an elderly man was found to have hyperthyroidism, with unintentional weight loss as the only symptom. The lack of other classic symptoms, the patient's sex (male), and his relatively young age made the diagnosis more difficult. The work-up of a relatively healthy patient of any age complaining only of weight loss must include a thyroid hormone assessment even if no signs or symptoms are present to suggest hyperthyroidism. Although unintentional weight loss is more commonly caused by a malignancy than by hyperthyroidism, screening for hyperthyroidism should be done initially in the evaluation. If the thyroid screening is normal, the longer and more expensive work-up for malignancy must be started.
Acknowledgements
Acknowledgements are due to Department of Radiology and Imaging, KIMS, Secunderabad, Telangana, India.
Conflict of interest
The authors declare no conflict of interest.
References
1. Lahey FH. Apathetic thyroidism. Ann Surg. 1931; 93(5):1026–1030.
2. Johnson PC, Kahil ME. Apathetic hyperthyroidism. A type of masked thyrotoxicosis. Tex Med. 1967; 63(2):59–62.
3. Lahey FH. Non-activated (apathetic) type of hyperthyroidism. N Engi J Med. 1931; 204:747–748.
4. McGaa RR, Whittaker RL, Tullis IF. Apathetic thyroidism: a review of the literature and report of four cases. Ann Intern Med. 1959; 50(6):1418–1432.
5. Thomas FB, Mazzaferri EL, Skillman TG. Apathetic thyrotoxicosis: a distinctive clinical and laboratory entity. Ann Intern Med. 1970; 72(5):679–685.
6. Fairclough PD, Besser GM. Apathetic T-3 toxicosis. Br Med J. 1974; 1(5904):364–365.
7. McClure DI. Biochemistry of depression. Can Psychiatr Assoc J. 1971; 16(3):247–252.
8. Stoffer SS, Jiang NS, Gorman CA, Pikler GM. Plasma catecholamines in hypothyroidism and hyperthyroidism. J Clin Endocrinol Metab. 1973; 36(3):587–589.
9. Prange AJ Jr, Lara PP, Wilson IC, Alltop LB, Breese GR. Effects of thyrotropin-releasing hormone in depression. Lancet. 1972; 2(7785):999–1002.