Full Text
Introduction
Intertrochanteric (IT) fractures of femur are common in elderly people with osteoporotic bones and often the result of minor domestic falls. Osteoporosis coupled with a tendency to fall is responsible for high incidence of hip fractures at this age. Life expectancy of Indian population is steadily increasing and this inturn, increases the geriatric population and the hip fractures.
The incidence of these fractures in females steadily increases with advancing age and overall female to male ratio is about 2:1.
Case presentation
Conservative treatment of her fractures with skeletal traction, which used to be the standard in earlier parts of 20th century, which involves prolonged confinement to bed. This type of treatment often resulted in systemic and local problems like pulmonary and renal complications, deep vein thrombosis, bed sores, disuse atrophy of muscles and bones, etc. The morbidity and mortality was very high. To overcome these problems internal fixation techniques have been used with better outcomes, in the later half of the 20th century. Since then, there has been a steady improvement in the internal fixation techniques. In the last few decades, sliding hip screw (DHS) became the standard way of fixation of IT fractures world over. In the late nineties, a new technique in the form of cephalomedullry fixation was introduced and is found to give equally good or even better results. Its usage for fixation of IT fractures rose from 3.1% in 1999 to 67% in 2006 in the developed world.
DHS is still the most commonly used device for fixation of IT fractures. DHS permits the proximal fragment to collapse or settle and seek its own position of stability. For stable IT fractures it is the surgery of choice. Many studies have reported predictable stability and healing in these stable fracture patterns. However fixation of unstable fractures with this devise remains a persistent challenge. Mechanical failure including loss of purchase of the compression screw within the femoral head, pulling of the side plate and dis-engagement of the screw and barrel have been reported to occur in as many as 28% of fractures. Additionally, over impaction of the fracture fragments may lead to significant loss of limb length. Malunion is very common following DHS fixation of IT fractures particularly the unstable variety.
On the other hand, caphalo-medullary fixation is said to have the following potential advantages as noted in Table 1. However, cephalo- medullary fixation is associated with the following disadvantages as noted in Table 2.
Table 1: Caphalo-medullary fixation potential advantages.
|
The device being intramedullary, load transfer is more efficient
|
|
Shorter lever arm between hip rotation center and femoral fixation component leads to a stronger construct and results in less transfer of stress and less implant failure.
|
|
Advantage of controlled collapse is maintained.
|
|
Sliding is limited by intramedullary location, so less shortening and deformity.
|
|
All the advantages of minimal access surgery.
|
Table 2: Caphalo-medullary fixation disadvantages.
|
Surgery is technically more demanding
|
|
procedure related complications are common
|
|
post operative mobilization and rehabilitation can still be difficult
|
In a recent randomized controlled trial by Parker and Bowers [1], comparing DHS and Proximal femoral nail, operative difficulties, operative time and radiological screening times were found to be more with P.F.N, but recovery of mobility was superior.
As for arthroplasty of IT fractures is concerned, there is little published data. Cemented bipolar arthroplasty with trochanteric reconstruction is a very good option for patients whose life expectancy is not more than ten years and who has unstable IT fractures. This is particularly so if the bones are severely osteoporotic or the hip is arthritic. Correct axial seating (restoration of length), femoral version and abductor function restoration are important technical aspects for a successful outcome. Pressurization of cement is better avoided for the fear of embolic manifestations, particularly in patients with cardiopulmonary compromise. Arthroplasty does not require `C` arm usage and also permits immediate weight bearing and faster rehabilitation.
Bipolar arthroplasty is done by me at KIMS for comminuted intertrochanteric fractures for the last ten years with very satisfying results. The typical patient for this type of surgery is aged 65 years or above with an unstable intertrochanteric fracture, associated with significant osteoporosis.
Pre operative evaluation
On admission a careful history is obtained particularly noting the pre operative mobility, usage of walking aids, medical co-morbidities, medications like anti platelet agents, steroids etc. Clinical examination focuses on general health status, local skin condition and neurovascular status in the limb. Necessary investigations are carried out and the results are reviewed. Operation theatre is booked for a planned surgical procedure the next day. Mean while appropriate referral services are arranged and their suggestions are implemented to optimize the patient’s health status to the extent possible.
Surgical procedure
Surgery is done (Figures 1 to 4) through a modified Hardinge`s approach with the patient in the lateral position. Hip joint capsule is incised in line with the femoral neck. Fracture is exposed and the broken greater trochanter is reduced anatomically and the distance from the tip of this trochanter to a marked point on the intact proximal end of the femoral shaft is measured. This measurement will help the surgeon to insert the prosthesis to the correct depth, so that limb length is restored and post op. dislocation is avoided by maintaining the soft tissue tension. The level of the top of the greater trochanter in relation to the femoral head center, on the intact contralateral side need to be taken into consideration for this purpose. A sub capital osteotomy of the femoral neck will facilitate femoral head extraction and the extracted head is measured to select the implant of appropriate size. At this stage, all the loose bits of fractured bone are excised leaving the lesser and greater trochanteric fragments into which the iliopsoas and abductors are inserted respectively. Acetabulum is cleared of any loose bits of bone and packed with a couple of gauze pieces. Now proximal femur is prepared with a rasp and washed thoroughly to remove all marrow elements. Selected Bipolar prosthesis is cemented into the femur to the correct depth based on the earlier measurements. Correct version also needs to be maintained. After the setting of cement, acetabulum is cleaned and cleared of any loose bits of bone and cement and the prosthesis is reduced. Reduction should be stable on longitudinal traction and external rotation of the limb. The incised hip capsule is repaired (Capsuloplasty) which will enhance the joint stability. Next is the greater trochanter fragment along with attached abductors is reduced onto the shaft fragment and fixed with a modified tension band technique as shown in the picture (Trochanterplasty). If the fragment is big and includes part of the upper shaft along with it, then a low profile plate with uni cortical screws can be used to fix the same. Good bone to bone contact is essential and cancellous bone graft can be packed into the gaps if any. Lesser trochanter fragment is usually small and can be left without fixation. This will not compromise the function. Elevated abductor vastus lateralis muscle flap is repaired anatomically. Wound is closed in the usual manner, over a suction drain.

Figure 1: Exposure of fracture site.

Figure 2: Biplolar prosthesis (Cement).
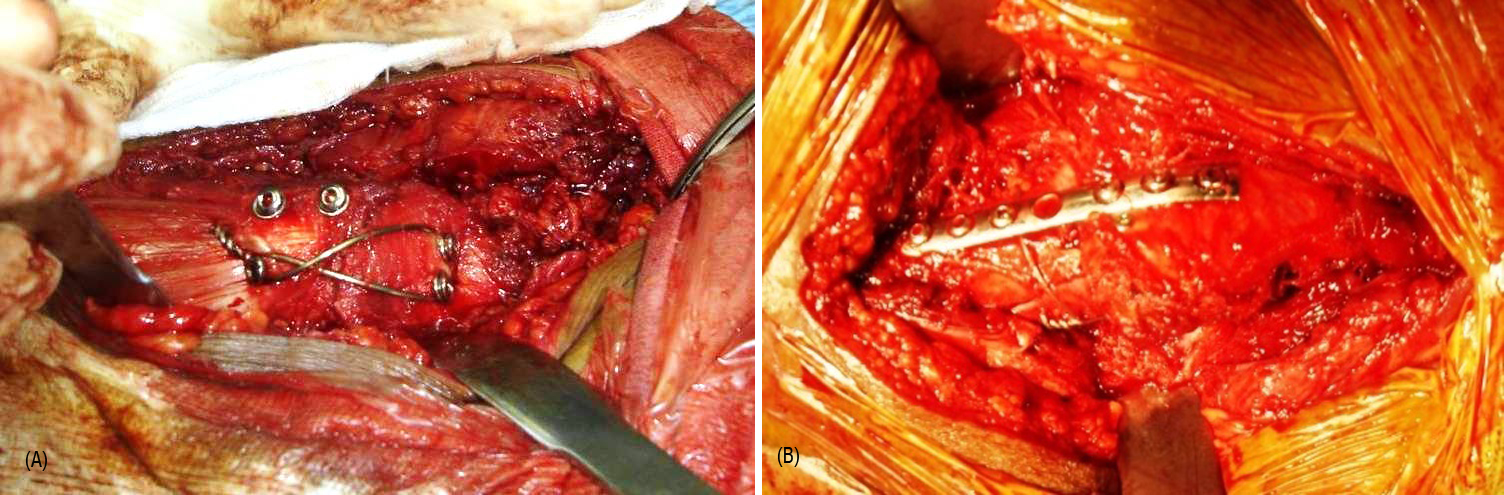
Figure 3: Trochanter reconstruction (A) Tension band, (B) Plating.
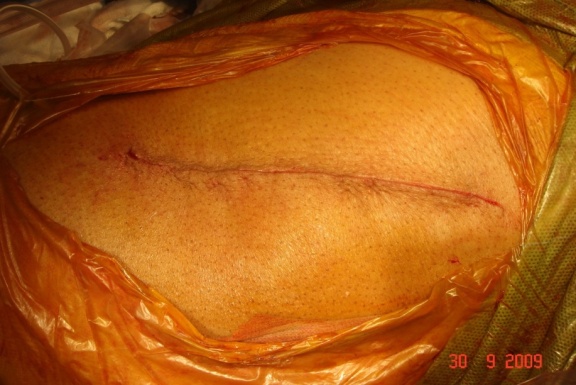
Figure 4: Wound closer.
Long stemmed Bipolar implant is used if there is significant sub trochanteric extension of the fracture. Calcar replacement option is also available for cases with significant postero-medial comminution.
Post operative management
From day one, in-bed exercises and mobility are advocated, to prevent complications like DVT, bed sores and pneumonia. Next day, out of bed mobility with the help of a walker is allowed with weight bearing as tolerated. On day three, wound dressings are changed and discharge planned based on patients comfort and mobility, usually on day 4 or 5 (Figures 5A, 5B, 6A and 6B).
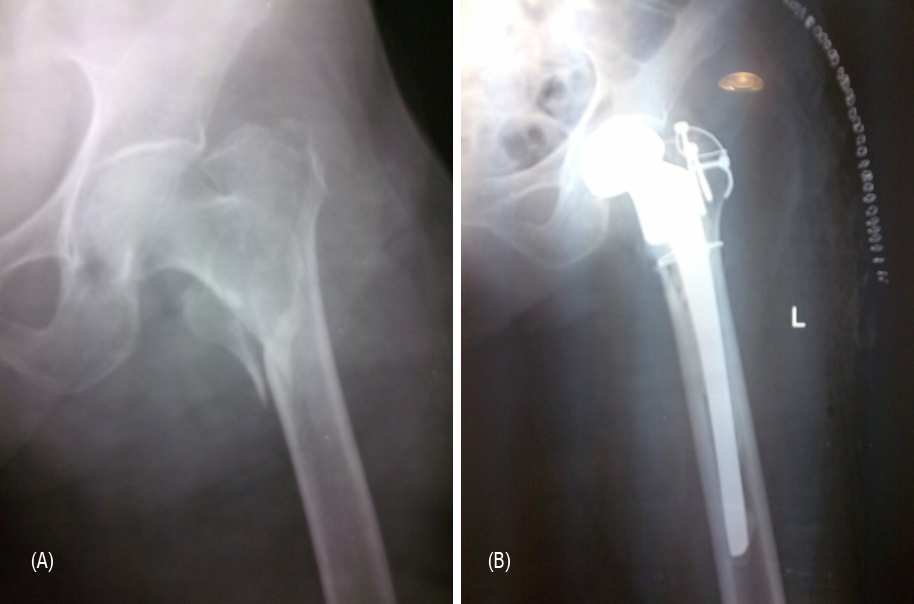
Figure 5: (A) Comminuted IT fracture. (B) Post operative radiograph.

Figure 6: (A) Patient sitting on 1st post operative day. (B) Patient walk with walking aid after 2 weeks post operative.
Total hip replacement is not advisable for IT fractures as a primary procedure, due to high risk of dislocation. Total hip replacement may be the only option for certain complications following internal fixations for intertrochanteric fractures. In such rare instances, when THR is under taken, one may have to use large heads, constrained liners, long stems with calcar replacement (Figures 7A, 7B, 7C, 7D).

Figure 7: (A) comminuted IT fracture of the left femur, (B) Postoperative radiograph, (C) Similar IT fracture of right femur 4 months later, (D) Similar reconstruction postoperative radiograph.
Conclusion
DHS is the procedure of choice for stable intertrochanteric fracture of any duration, without arthritis changes in the leg. For comminuted IT fractures in relatively young non active people PFN may be the surgery of choice. For comminuted IT fracture in elderly people, whose life expectancy is around 8 to 10 years comminuted bipolar arthroplasty is appropriate. For fixed osteosynthesis provides for IT fractures total high replacement is removed.
Conflicts of interest
Author declares no conflicts of interest.
References
1. Parker MJ, Bowers TR, Pryor GA. Sliding hip screw versus the Targon PF nail in the treatment of trochanteric fractures of the hip: a randomised trial of 600 fractures. J Bone Joint Surg Br. 2012; 94(3):391-397.
2. Calder SJ, Anderson GH, Jagger C, Harper WM, Gregg PJ. Unipolar or bipolar prosthesis for displaced intracapsular hip fracture in octogenarians: a randomised prospective study. J Bone Joint Surg Br. 1996; 78(3):391-394.
3. Green S, Moore T, Proano F. Bipolar prosthetic replacement for the management of unstable intertrochanteric hip fractures in the elderly. Clin Orthop Relat Res. 1987; (224):169-177.
4. Rogmark C, Carlsson A, Johnell O, Sernbo I. A prospective randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur. Functional outcome for 450 patients at two years. J Bone Joint Surg Br. 2002; 84(2):183-188.
5. Tabsh I, Waddell JP, Morton J. Total hip arthroplasty for complications of proximal femoral fractures. J Orthop Trauma. 1997; 11(3):166-169.