Case Report
2017
September
Volume : 5
Issue : 3
Complete hydatidiform mole with a coexistent live fetus in a twin pregnancy
Kashif M Mohiuddin, Chinmayee Ratha, Satish Rao I
Pdf Page Numbers :- 111-114
Kashif M Mohiuddin1,*, Chinmayee Ratha2 and Satish Rao I1
1Department of Pathology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India
2Department of Fetal medicine, Navodaya hospital, PG Road, Secunderabad-500003, Telangana, India
*Corresponding author: Dr. Kashif M Mohiuddin, Department of Pathology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India. Tel.: 9848969543; Email: kashifhazim@gmail.com
Received 12 April 2017; Revised 15 June 2017; Accepted 24 June 2017; Published 30 June 2017
Citation: Mohiuddin KM, Ratha C, Satishrao I. Complete hydatidiform mole with a coexistent live fetus in a twin pregnancy. J Med Sci Res. 2017; 5(3):111-114. DOI: http://dx.doi.org/10.17727/JMSR.2017/5-21
Copyright: © 2017 Mohiuddin KM et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: The reported incidence of hydatidiform mole with coexisting pregnancy is one in 22 000–100 000 pregnancies, most of them being complete hydatidiform moles (CHM) with a fetus; however, the reported prevalence, for a partial mole with a coexisting fetus is 0.005–0.01% of pregnancies.
Case report: This is a case report of a hydatidiform mole with a coexistent live fetus diagnosed at 18 weeks. After thorough counselling, the pregnancy was continued as per the patient’s desire. The pregnancy was closely monitored with serial Serum β hCG, and ultrasound for fetal growth. An emergency caesarean delivery was done at 30 weeks, due to bleeding per vaginam. A live baby was delivered with near normal Apgar score. The placenta with molar tissue was sent for histopathological examination. The histopathology revealed a complete mole with normal placenta. Her serum β hCG reached normal levels after delivery, and she is now on surveillance. Though the general trend is to terminate pregnancy in twins with coexistent mole in anticipation of complications, under close surveillance, optimal outcomes can be achieved.
Conclusion: The option of continuing a twin pregnancy with a complete mole is acceptable. However a close surveillance is required to detect potential early signs of complications. Histopathological examination is essential in distinguishing between partial and complete mole and/or with ancillary studies.
Keywords: complete hydatidiform mole; twin pregnancy; partial mole; trophoblast; hydatidiform mole
Full Text
Introduction
Twin pregnancy with CHMF (complete hydatidiform mole coexisting with a live fetus) resulting in a healthy take-home baby is rare, with only less than 60 cases documented in detail in literature. The estimated incidence is of one in 22,000–100,000 pregnancies [1], with most being complete hydatidiform moles (CHM) with a fetus; however, the reported prevalence for a partial mole with a coexisting fetus is 0.005–0.01% of pregnancies [2]. These cases are at high risk of spontaneous abortion, preterm delivery, intrauterine fetal death, antepartum bleeding, preeclampsia, persistent trophoblastic disease (PTD).
Case report
A 25-years-old female with complete mole and a coexistent live fetus detected on ultrasound at 18 weeks of gestation with a normal karyotype fetus on amniocentesis at 20 weeks. The pregnancy was continued as per the patient’s desire and was closely monitored. At 30 weeks the patient had bleeding per vaginum for which emergency caesarean section was performed and a live baby with a near normal Apgar score was delivered. The placenta with molar tissue was sent for histopathological examination. Her serum β hCG reached normal levels after delivery, and she is now on post-molar surveillance. The placenta with molar tissue was received in formalin. It had normal eccentric cord (19 cm, diameter of 0.6 to 0.1 cm) with three vessels. The cord had mild increase in coiling (6 twists) towards the left. There was normal presence of peri-arterial Wharton’s jelly. The disk (344 gm; fixed and trimmed; 16 × 12 × 4 cm) was roughly oval [Figure 1a]. The fetal surface is smooth, shiny with prominent vessels. Molar tissue [Figure 1a] was adherent to the placenta at one pole which was of size 12 × 12 × 3 cm composed of multiple grape like vesicles weighing 240 gm. The serial sections of placenta were unremarkable [Figure 1b]. On microscopy the sections from cord, membranes and disk were unremarkable. The molar tissue predominantly showed degenerative changes and was composed of villi [Figure 2a] which were diffusely edematous [Figure 2d, e] displaying cisterns and trophoblastic proliferation. The trophoblastic proliferation involved the entire circumference of the villi in molar tissue [Figure 2b, c].

Figure 1: (a) Placenta and molar tissue, (b) Serial sections of placenta.
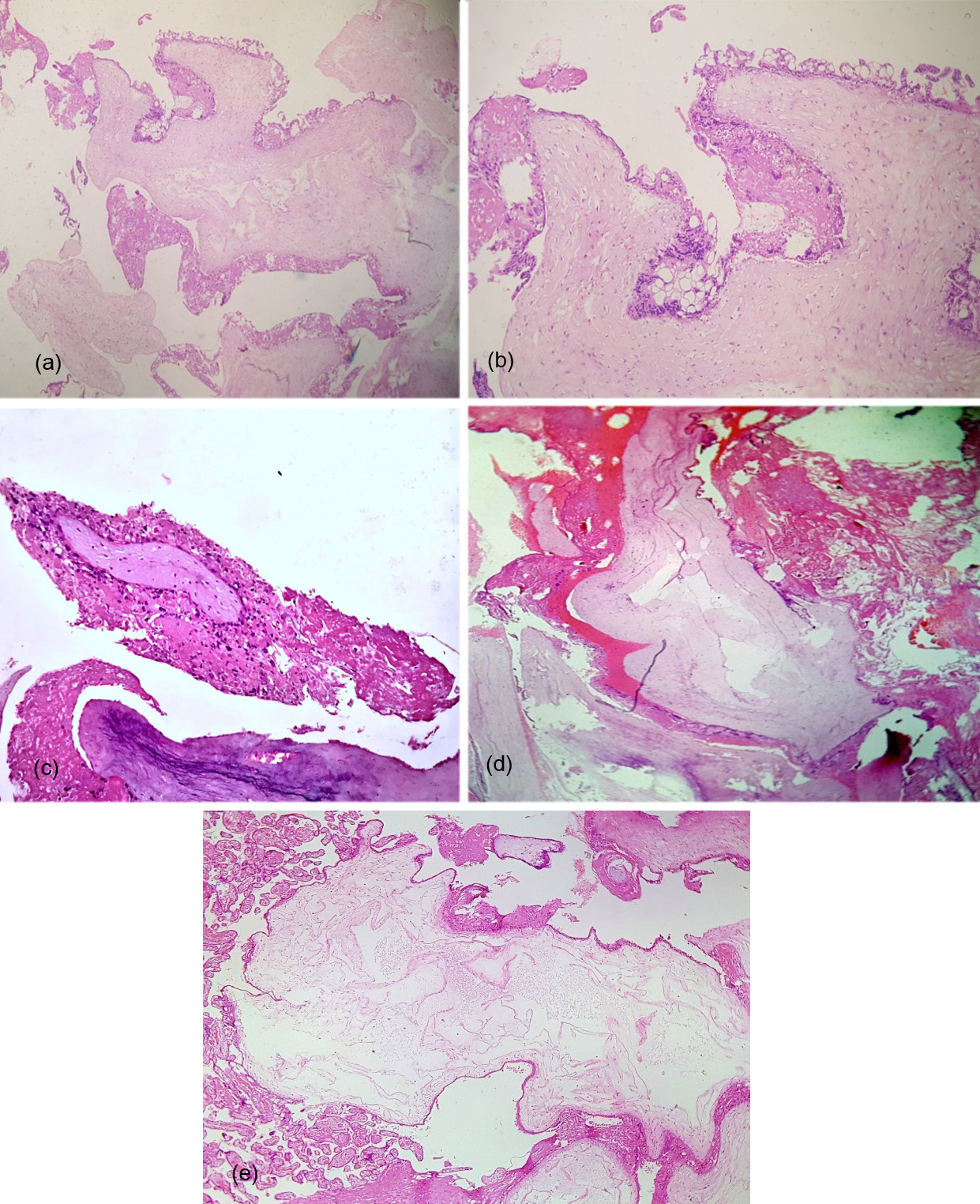
Figure 2: (a) Low power view of abnormal Villi, H&E 40x, [b, c] Villi with circumferential trophoblastic proliferation, H&E 100x, [d, e] Edematous villi.
Discussion
There are about less than 250 cases of complete mole with twin pregnancy documented in literature, and only less than 60 cases have resulted in live birth [3]. Vassilakos et al. based on cytogenetic analysis first described, partial and complete hydatidiform mole (CHM), which arise by different mechanisms [4]. Partial moles are derived from dispermic fertilization of a haploid normal oocyte and give rise to triploid set of chromosomes whereas CHM contains a diploid set of 46 paternally derived chromosomes, without any fetal parts. The fetuses are almost always triploid in partial moles and the indication for a termination of pregnancy is recommended. In contrast, the fetus may be normal in a twin pregnancy with a CHMF and continuation of pregnancy is commonly associated with maternal complications.
Ultrasonography is helpful in diagnosis of a hydatidiform mole with co-existent fetus in the first trimester [5]. Prenatal testing of the fetal karyotype is essential as it helps in deciding continuation and prognosis of the pregnancy. Termination of pregnancy is recommended in a triploid fetal karyotype and where as a diploid fetal karyotype is usually associated with a viable fetus with a normal placenta co-existing alongside a molar tissue as in this case, in which the pregnancy can be continued with close monitoring.
Usually partial mole associated fetuses are triploid but fetuses with normal karyotype also can occur in this setting. The fetuses with partial mole are associated with asymmetrical intra uterine growth restriction (IUGR) and malformations [6]. Histopathological examination is important in distinguishing between the moles either by histopathology and/or with ancillary methods like p57 immunostain. In the present case the features were compatible with complete mole, while clinically it was believed to be a partial mole.
Table 1 depicts the diagnostic features of moles which are helpful in distinguishing them from each other based on clinical and histopathological features [7]. Ancillary methods may be helpful in difficult situations. P57 which is paternally imprinted can be used in flow cytometry or immunohistochemistry for discriminating complete from partial moles [8]. Mesenchymal dysplasia and hydropic changes in the placenta can be diagnosed by clinical and the histopathological features.
Table 1: Depicts the diagnostic features of moles [7].
|
Diagnostic features
|
CHM
|
VECHM
|
PHM
|
|
Clinical presentation
|
Vaginal bleeding in second trimester (average 16 weeks), excessive uterine size, hyperemesis, toxaemia, preeclampsia or hyperthyroidism
|
Missed abortion (6.5–12 weeks of gestation)
|
Vaginal bleeding, missed or incomplete abortion in late first or early second trimester
|
|
Pretreatment hCG (mIU/ml)
|
Elevated (>100 × 103 in>43% of cases)
|
Normal or elevated (<100 × 103)
|
Normal or elevated (<100 × 103 in >93% of cases)
|
|
Ultrasound
|
Snow storm pattern without foetus formation
|
-
|
Focal cystic change with foetus formation
|
|
Macroscopy
|
Bulky specimen with hydropic change involving all villi, absence of gestational sac and foetal development
|
Frequently no gross abnormality
|
Hydropic change involving some villi, gestational sac and foetal tissue may be present
|
|
Chorionic villi
|
Diffuse enlargement, round to oval shapes
|
Normal size, polypoid or cauliflower shapes
|
Mild, with syncytiotropho- blast knuckles
|
|
Trophoblastic hyperplasia
|
Marked, often circum- ferential with intervillous trophoblast bridging
|
Mild, often on villous tips
|
Mild, with syncytiotropho- blast knuckles
|
|
Cytological atypia
|
Marked
|
Mild to moderate
|
Limited to mild
|
|
Villous stroma
|
Marked oedema with frequent cistern formation and trophoblastic inclusions, absence of vasculature and nucleated RBCs
|
Cellular and myxoid with prominent karyorrhexis, fetal capillaries may be present
|
Occasional cistern formation, round to oval trophoblastic pseudo-inclusions, presence of vasculature and nucleated RBCs (not always evident)
|
|
p57 immunostain
|
Absence of nuclear staining in cytotrophoblast and villous stromal cells
|
Absence of nuclear staining in cytotrophoblast and villous stromal cells
|
Presence of nuclear staining in cytotrophoblast and villous stromal cells
|
|
DNA genotyping
|
Diploid diandric (paternal-only) genome
|
Diploid diandric (paternal-only) genome
|
Triploid diandric- monogynic genome
|
Abbreviations: CHM: complete hydatidiform mole; VECHM: very early complete hydatidiform mole; PHM: partial hydatidiform mole.
Prenatal diagnosis by amniocentesis as done in this case has been suggested to rule out triploidy or other genetic abnormalities, before continuation of a pregnancy [6]. Due to confined placental mosaicism there may be variation between fetal and placental karyotype is the reason why chorionic villous sampling is not recommended. The survival of the fetuses with complete mole are better than that of fetuses with partial mole [9] unless when it occurs in a dizygotic twin, with one fetus and the other oocyte giving rise to a partial diploid mole, however, abnormal fetus may result in a monozygotic twin with triploidy giving rise to a partial mole [10]. In case of maternal complications like severe preeclampsia or bleeding one must be prepared for termination, and conservative management in these pregnancies puts the mother at risk of serious complications.
Steller et al. suggested that the risk of PTD is higher in cases of CHMF compared with single molar pregnancies and commonly progresses to metastatic disease [11] however Sebire and Niemann found out that the risk of PTD after CHMF is not significantly higher than in single molar pregnancies [12, 13].
Conclusion
A twin pregnancy with a complete mole and a coexisting live fetus requires a thorough evaluation, and pregnancy may be continued under close surveillance for an optimal outcome. Histopathological examination is essential for distinguishing between partial and complete mole and/or along with ancillary studies. Close follow-up is necessary during and after gestation to exclude persistent trophoblastic disease.
Conflicts of interest
There are no conflicts of interest.
References
[1] Sebire NJ, Foskett M, Paradinas FJ, Fisher RA, Francis RJ, et al. Outcome of twin pregnancies with complete hydatidiform mole and healthy co-twin. Lancet. 2002; 359:2165–2166.
[2] Elizabeth A, Danemond S, Hull A. Placental pathology casebook. Complete hydatidiform mole with coexistent term twin pregnancy. J Perinatol. 2001; 21(1):72–75.
[3] Dolapcioglu K, Gungoren A, Hakverdi S, Hakverdi AU, Egilmez E. Twin pregnancy with a complete hydatidiform mole and co-existent live fetus: two case reports and review of the literature. Arch Gynecol Obstet. 2009; 279:431–436.
[4] Moini A, Riazi K. Molar pregnancy with a coexisting fetus progressing to a viable infant. Int J Gynecol Obstet. 2003; 82:63–64.
[5] Montes-de-Oca-Valero F, Macara L, Shaker A. Twin pregnancy with a complete mole and co-existing fetus following in vitro fertilization. Hum Reprod. 1999;14:2905–2907.
[6] Guven ESG, Ozturk N, Deveci S, Hizli D, Kandemir O, et al. Partial Molar Pregnancy and coexisting fetus with Diploid Karyotype. J Matern FetalNeonatal Med. 2007; 20(2):175–181.
[7] Gestational trophoblastic disease; Molar pregnancies. World health organization classification of tumours of female reproductive organs, 4th edition, page no.165
[8] Massardier J, Golfier F, Journet D, Frappart L, Zalaquett M, et al. Twin pregnancy with complete hydatidiform mole and co existent fetus: Obstetrical and oncological outcomes in a series of 14 cases. Euro J Obstet Gynecol Reprod Biol. 2009; 143(2):84–87.
[9] Matsui H, Sekiya S, Hando T, Wake N, Tomoda Y. Hydatidiform mole a coexistent with a twin live fetus - A national Collaborative study in Japan. Hum Reprod. 2000; 15(3):608–611.
[10] Chu W, Chapman J, Persons DL, Fan F. Twin pregnancy with partial hydatidiform mole and coexistent fetus. Arch Pathol Lab Med. 2004; 128(11):1305–1306.
[11] Steller MA, Genest DR, Bernstein MR, Lage JM, Goldstein DP, et al. Natural history of twin pregnancy with complete hydatidiform mole and coexisting fetus. Obstet Gynaecol. 1994; 83(1):35–42.
[12] Sebire NJ. Prenatal diagnosis and management of twin pregnancies complicated by a co-existing molar pregnancy. Prenat Diagn. 2006; 26(4):373.
[13] Niemann I, Sunde L, Peterson LK. Evaluation of the risk of persistent trophoblastic disease after twin pregnancy with diploid hydatidiform mole and coexisting normal fetus. Am J Obstet Gynecol. 2007; 197(1): 45.e1-45.e5.