Full Text
Case 1
A 32-year-old female with a past medical history of systemic lupus erythematosus (SLE), post renal transplant presented to the outpatient room with dyspnea, cough and mucoid expectoration since 1 month without any fever, hemoptysis, or chest pain. Upon arrival the outpatient department, she was having oxygen saturation of 95 to 97 percent in room air and all vital signs were within normal range. On physical examination, there were significant signs for decreased air entry on the right side. The remaining physical examination was unremarkable. Chest radiograph revealed a foreign body in the right intermediate bronchus (RIB). Computed axial tomography (CT) chest revealed FB in RIB (Figure 1A, 1B). The patient denied the use of any sedative medications or alcohol intake. She underwent flexible bronchoscopy. After administration of 100 mcg of fentanyl, a flexible fiber optic bronchoscope was introduced orally. Topical lidocaine was administered to the glottis and the trachea was entered. A foreign body was identified in the right intermediate bronchus (Figure 2A, 2B). Endobronchial forceps was used to grasp the foreign body. Light traction was applied and the foreign body was slowly dislodged. With the FB grasped by the forceps, the bronchoscope, forceps, and FB were extracted en bloc through the vocal cords and then the foreign body was removed. The patient was observed for a few hours during which she reported dramatic improvement of dyspnea and she was discharged in a stable condition. She came for follow up after 20 days. She recovered well and was absolutely free of symptoms.
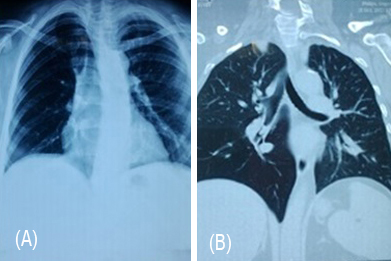
Figure 1: (A) Chest radiograph showing atelectasis of right middle lower lobe. (B) CT image showing foreign body in right intermediate bronchus.
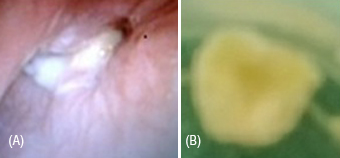
Figure 2A, B: Foreign body was identified in the right intermediate bronchus.
Case 2
A 22 year old male patient came with complaints of shortness of breath, cough with expectoration since 3 months, purulent in nature. It was diagnosed outside as bronchial asthma and started on inhalers. Patient felt no improvement with inhalers. There was no chest pain, fever, hemoptysis or pedal edema. Bowel and bladder habits were normal. His past history revealed that he was perfectly well upto the age of 6 years. At the age of 6 years he was admitted in a hospital with complaints of cough with expectoration, fever and diagnosed as right sided pleural effusion with pneumonia. Pleural fluid aspiration was done. At that time, he was treated with antibiotics. Pneumonia and pleural effusion were resolved, he had symptomatically improved. But from then on, patient had same complaints fever, cough with expectoration, purulent in nature on and off. Patient was hospitalized for the same complaints for several times, and was treated as having different diseases like typhoid, lower respiratory tract infection and malaria. Patient gave history of hospitalization almost once in every 6 months for the last few years.
Physical development was not much different from the same age group people. No other comorbidities or addictions and no family history of asthma. On examination, nothing significant was formed except decreased air entry in right lower zone. His routine investigations showed normal with slight increase in leucocytes. His chest radiograph showed right middle and lower lobe collapse (3A).
Sputum was negative for Koch’s. His computed axial tomography (CT) chest showed circumscribed foreign body in RIB. He was planned for bronchoscopic removal of foreign body. Bronchoscopy revealed, right intermediate bronchitis stenosis like a pin hole meatus, and pus was leaking from that site (Figure 4A, B, C). Suctioning of all the purulent material was done, sent for analysis and advised for cardiothoracic surgeon’s opinion. Patient underwent right lower lobectomy on follow up, his complaints resolved completely.

Figure 3: Radiograph of chest showing atelectasis right middle and lower lobe
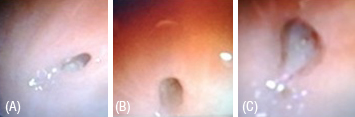
Figure 4A, B, C: Bronchoscopy: right intermediate bronchus stenosis like a pin hole meatus with pus leaking from that site.
Discussion
Foreign body aspiration is sometimes referred to as a cafe coronary (elderly adults) [1]. Foreign bodies have a tendency to lodge in the right main stem bronchus because it is more vertical and larger in diameter than the left main stem bronchus. However, as in these case reports, foreign bodies may enter the right intermediate bronchus.
The nature of aspirated foreign bodies varies significantly with the geographical and cultural differences throughout the world. Food is the most common aspirated foreign body. Nuts, seeds, pins, nails, and dental appliances following dental procedures have all been documented [2, 3]. Since foreign bodies are typically stuck distally in the lower lobe bronchi or the bronchus intermedius, acute presentation in adults is rare; however, life-threatening asphyxia and sudden decompensation secondary to complete obstruction may occur [4]. Our patients presented with cough which is the most common presenting symptom. Other symptoms include fever, chest pain, and hemoptysis.
Dyspnea was reported by our patient but is generally a rare presenting symptom. Physical examination of adults with foreign body aspiration is often unrevealing. Stridor, wheezing, or diminished breath sounds may be encountered if the degree of obstruction is severe enough. Foreign bodies can remain undetected for months in adults which require a high index of suspicion for diagnosis as most adults do not recall a history of choking [5]. Many foreign bodies are incidentally seen on radiographic imaging requested for symptoms mistakenly attributed to other medical conditions including asthma and unresolving recurrent pneumonia [5, 6] similar to second case. If a diagnosis of foreign body aspiration is delayed, a retained foreign body may result in unresolving pneumonia, lung abscess, and bronchiectasis. Also, formation of granulation tissue around the foreign body may occur and may resemble bronchogenic carcinoma [7]. Numerous risk factors may facilitate foreign body aspiration in adults including impairment of swallow reflex and ineffective airway protective mechanisms such as aging, alcohol, sedative use, altered sensorium, neurological dysfunction and loss of consciousness.
Therapeutic removal of foreign bodies is not a new concept. The earliest report of airway foreign body removal was performed via bronchotomy by Louis in 1759 [8]. The first endoscopic removal of a foreign body occurred in 1897 [9] and since then bronchoscopy has remained the gold standard for evaluation of patients with high clinical suspicion for foreign body aspiration.
Our case describes the successful extraction of a large foreign body using fiber optic bronchoscopy. The success rate of fiber optic bronchoscopic extraction in adults ranges from 60 to 90 % [10, 11]. The procedure is usually done under local anesthesia. Despite a high success rate, fiber optic bronchoscopy extraction entails some risks. The fiber optic forceps provide less grasping power of a foreign body compared to rigid bronchoscopy forceps which may result in migration of the foreign body to the contralateral lung and can lead to a fatal outcome [12]. For this reason, one should have a low threshold for conversion to a rigid bronchoscopy. Fiber optic is a preferable option in contrast to rigid bronchoscopy in the case of a distally wedged FB, in mechanically ventilated patients, or in the presence of spine, craniofacial, or skull fractures that prevent the manipulation required for rigid bronchoscopy [10]. In younger children, the optimal extraction technique is an outstanding issue currently under debate. Surgical extraction of foreign body through bronchotomy or even segmental resection under general anesthesia is the last resort when extraction using bronchoscopy is unsuccessful. Presence of an experienced thoracic surgeon and anesthesiologist is essential to prevent significant morbidity and mortality associated with unsuccessful attempts of retrieval by bronchoscopy.
The use of corticosteroids and antibiotics in the setting of foreign body aspiration is controversial. It is usually recommended to use a short course of corticosteroids before FB removal when a well-tolerated FB is encased in a bulky and bleeding granulation tissue. Corticosteroids are not recommended as a prophylactic measure for postoperative subglottic edema; however, it can be used in conjunction with aerosolized epinephrine or helium oxygen therapy in cases of established subglottic edema. Antibiotics are not indicated except in the setting of documented respiratory tract infection.
Immediate removal of tracheobronchial foreign body is essential to prevent life-threatening complications. Bronchoscopic extraction of foreign body even by a skilled operator is not a risk-free procedure and it has to be done in a monitored setting with complete resuscitative measures available as acute decompensation may occur secondary to accidental dislodgment of the foreign body. Procedure outcome varies significantly by the type and location of the obstructing foreign body as well as the level of experience of the bronchoscopist.
Conclusion
Clinical suspicion, early diagnosis and removal of foreign body (FB) gives dramatic clinical improvement as happened in the first patient, where as lack of suspicion and delayed diagnosis have led to lobectomy in second patient. This could have been prevented if it is identified early in child hood itself.
Conflicts of interest
Authors declare no conflicts of interest.
Acknowledgements
Acknowledgements are due to department of Radiology and Imaging, and thoracic surgery, KIMS, Secunderabad.