Full Text
Fibrous dysplasia (FD) is a developmental non hereditary osseous disorder. It is often observed in childhood but presents throughout life. The osseous structure is destroyed and is replaced by fibrous tissue. The bone forming cells fail to mature and produce too much of fibrous and connective tissue. A defective gene exists in the cells that form the bone and other tissues. However, gene testing and DNA are not helpful. Research is going on to find out the genetic and molecular basis of this disorder.
FD is classified into monostotic, polyostotic and polyostotic associated with precocious puberty. Café au lait spots on the skin and endocrinal changes are also present in addition to polyostotic fibrous dysplasia and are called “McCune-Albright Syndrome”. This is found more often in girls although FD in general is more common in boys.
Clinical presentation depends mostly on the bone affected and often is detected as an incidental finding in the radiological investigations done for other ailments. Some of these lesions do not require any treatment unless there is deformity and disability to the patient.
Although fibrous dysplasia is usually sporadic, a number of associations are well recognised:
- McCune-Albright syndrome: In 2 - 3 % of cases with the polyostotic form
- isolated endocrinopathy without the full McCune-Albright syndrome
o precocious puberty in girls o hyperthyroidism
o hyperparathyroidism : renal stones, calcinosis
o acromegaly
o diabetes mellitus
o cushing syndrome : osteoporosis, acne
o growth retardation
o neurofibromata
o rickets / osteomalacia
Mazabraud syndrome
It is FD with soft tissue myxomas which are rare. These are typically multiple intramuscular lesions in the vicinity of most severely affected bone.
Cherubism
It is another form of FD encountered in children with bilateral swelling of the jaws. The mandible is more commonly affected than the maxilla. Spontaneous regression may occur as the child grows into adults’ stage. Radiological manifestations include diffuse thickening of the jaws (Figure 1).

Figure 1: Cherubism – note the symetrical enlargement of the mandible.
Fibro osseous dysplasia / ossifying fibroma
Generally occurs in children less than 10 years. Spontaneous regression is known. Any surgical correction leads to recurrence. Osteofibrous Dysplasia (OD) OD is another entity commonly involving the tibial shaft. Radiologically, an elongated lytic lesion with areas of sclerosis and anterior bowing of the tibia are classical features (Figure 2).
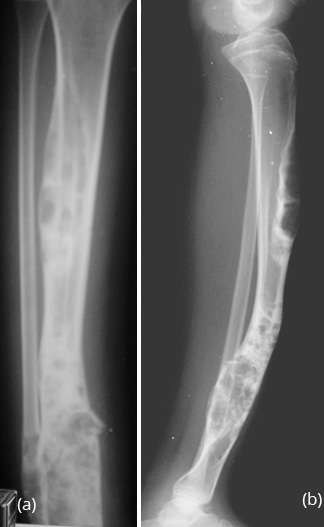
Figure 2a,b: Osteofibrous dysplasia of the tibia. Note the lytic and sclerotic changes scattered. Anterior bowing of the tibia is a characteristic finding.
Imaging findings
Conventional radiology is best for diagnosis. The involved bone is expanded with a lytic centre surrounded by thick rind. The matrix is ground glass but rarely may contain calcifications.
Craniofacial bones are affected in 10-25%. In the skull, the base is most often involved with dense sclerosis (Figure 3).
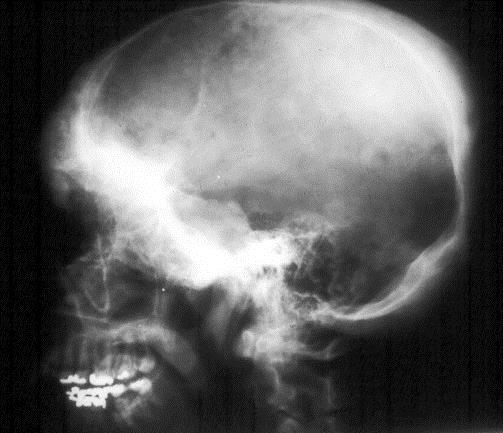
Figure 3: FD skull. Note diffuse sclerosis of the bones at the base.
Occasionally, moth eaten appearance may be seen, simulating metastasis or myeloma (Figure 4ab). The age of the patient often differentiates from other lesions.
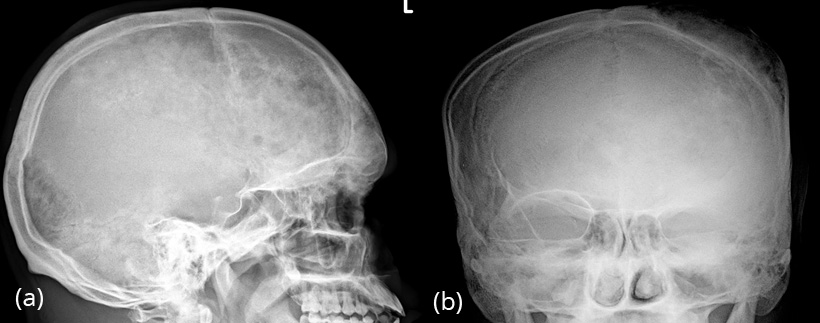
Figure 4a,b: FD skull in a 24yr old. Note the moth eaten appearance of the frontoparietal bones.
Paranasal sinuses are frequently involved (Figure 5a). When the maxilla is involved it may simulate chronic sinusitis (Figure 5b).
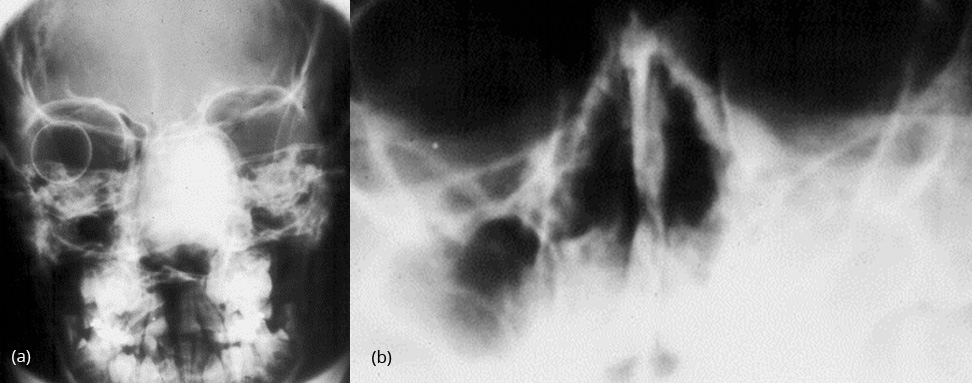
Figure 5: FD – (a) Involving ethmoids, (b) Involving the left maxillary sinus.
The vault of the skull shows a large lytic lesion containing islands of bone surrounded by sclerotic bone. This is often misdiagnosed as Paget’s disease (Figure 6).

Figure 6: FD skull – sclerosis of the base of the skull with islands in the vault simulating Paget’s.
Bony thoracic cage In the bony thoracic cage the ribs are frequently affected (Figure 7).
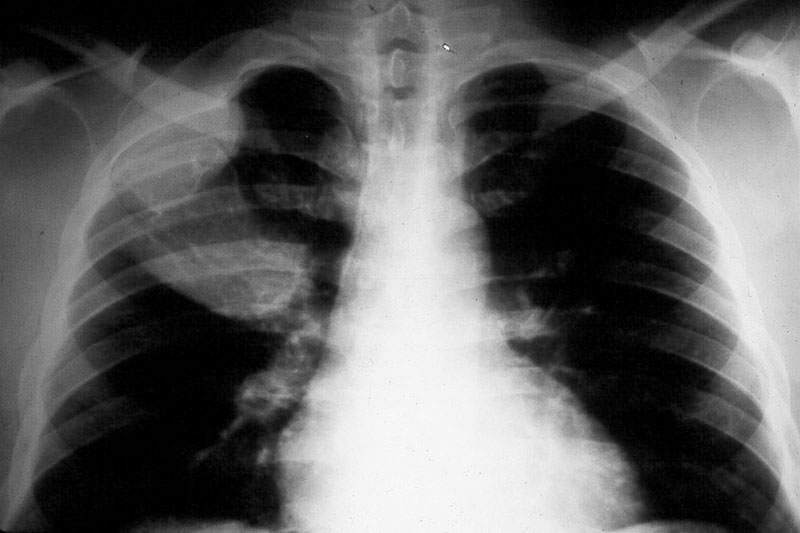
Figure 7: FD – note the expanding lesions of the right 1st and 2nd ribs.
The lesions are often long and expand the bone (Figure 8).
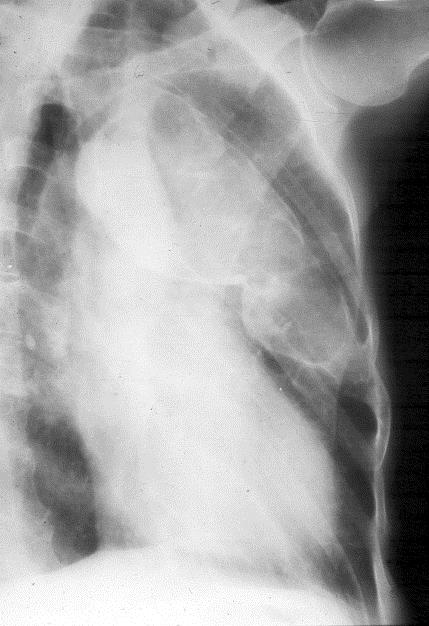
Figure 8: FD – Oblique view of the left 4th rib with expansion.
Ground glass appearance in an expanded lesion is characteristic (Figure 9).

Figure 9: FD – Right 5th rib shows localized expansion with new bone formation.
Uniform expansion with lobulated and thin cortex is often noted (Figure 10).

Figure 10: FD – Right 5th rib shows localized expansion with lobulation of the cortex The clavicles are rarely affected. The lesion can be a mixture of lysis and osteolysis or entirely lytic and expanding (Figure 11ab).
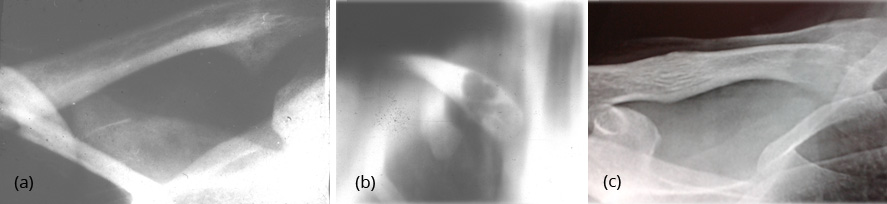
Figure 11: FD Clavicle – (a) Sclerotic lesion, (b) Tomogram showing a cystic lesions in the medial end, (c) Sclerotic lesion.
The scapular lesion may simulate aneurysmal bone cyst or show a combination of sclerosis and lysis (Figure 12).

Figure 12: FD Scapula - expanding cystic lesion.
In the humerus, a combination of osteolysis with a rind or diffuse expansion of the shaft may be noted (Figure 13).

Figure 13: FD – Humerus. Note the expanding lytic lesion in a 3 yr old .
In the radius and ulna, cystic lesions may be noted or diffuse sclerosis with deformity (Figure 14a,b,c,d).
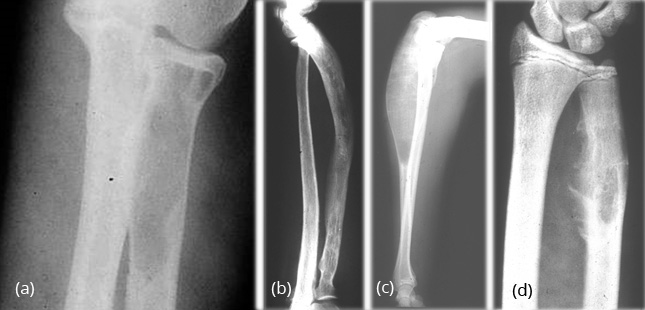
Figure 14: FD – (a, b) Radius, (c, d) Ulna In the hands, monostotic is rare.
Polyostotic is common with asymmetrical bilateral changes with mixed densities are encountered (Figure 15a,b).

Figure 15: FD – (a) Monostotic involving 5th metacarpal, (b) Polyostotic bilateral involving phalanges and metacarpals.
In the pelvis, proximal ends of the femura are commonly involved. Generally it is unilateral (Figure 16). In polyostotic form, involvement of the iliac and other bones is common (Figure 17). Radiologically, the head and neck of the femur are deformed and present a shepherd’s crook deformity (Figure. 18). On occasion, a cystic lesion with multiple loculations is encountered (Figure 19).

Figure 16: FD – Femur. Note the diffuse involvement.

Figure 17: FD – Polyostotic involving left iliac bone and femur.

Figure 18: FD – 8 yr old child – shepherd crook deformity of femur.

Figure 19: FD – Multiloculated appearance.
Shafts of femur, tibia, fibula etc., show expanding lesion with a thick rind. Ground glass appearance of the matrix is the hall mark for diagnosis (Figures 20a,b,c & 21a,b).
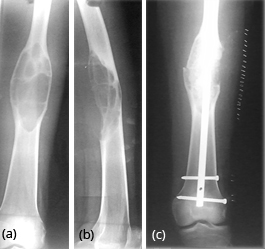
Figure 20: FD – (a,b) Mid shaft of femur simulating aneurysmal bone cyst, (c) post operative.

Figure 21a,b: FD tibia – incidentally found when investigating for trauma.
Short bones of the feet are also affected with variable expansions associated with lysis and sclerosis.
Isolated involvement of the vertebral column is quite rare. Radiologically, the lesion may simulate hemangioma or Paget’s disease (Figure 22a,b).
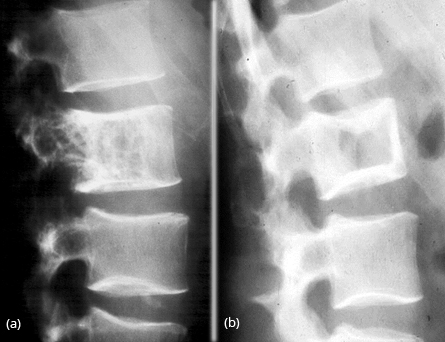
Figure 22: FD vertebra – (a) Simulates hemangioma, (b) Simulates picture frame appearance of Paget’s disease.
Fibrous Dysplasia – Radiological findings
- Lytic area with a rind.
- “Smoky” matrix
- “Calcific” matrix
- Thin cortex when aggressive
- Mixed osteolysis & sclerosis
Complications
- Fractures
- Pseudoarthrosis
- Deformed limbs
- Modelling deformities
- Malignant transformation
- Rickets / Osteomalacia
CT findings (Figure 23a,b, 24)
- Ground-glass opacities : 56 % 4
- Homogeneously sclerotic : 23 %
- Cystic : 21 %
- Well-defined borders
- Expansion of bone, with intact cortex
- Endosteal scalloping may be seen [6]

Figure 23: CT FD – (a) skull and paranasal sinuses, (b) lateral view with involvement of the vault and frontoparietal bones.

Figure 24: CT FD spine – cross section. Note the ground glass appearance.
MRI – (Figure 25a,b,c)
MRI is not particularly useful in differentiating fibrous dysplasia from other entities as there is marked variability in the appearance of the bone lesions, and they can often resemble tumour or more aggressive lesions.
On T1-weighted images, the signal intensity is usually low to intermediate, depending on the ratio of fibrous tissue to mineralized matrix. Lesions with high fibrous tissue content tend to have intermediate signal intensities, whereas lesions with highly mineralized stroma tend to show lower signal intensities. On T2-weighted images, the MR signal intensities are more variable. Some lesions with a highly mineralized matrix show correspondingly low signal intensities, whereas lesions with high fibrous tissue content and cystic spaces return high signal intensities (Figure 26a,b).
Heterogeneous enhancement after administration of gadolinium is noted.
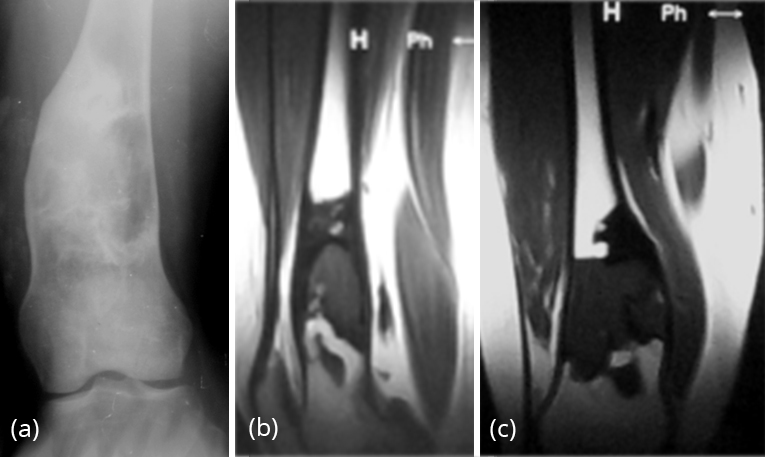
Figure 25: FD – (a) plain film, (b, c) MRI – Lower end of femur showing low intensity signal.
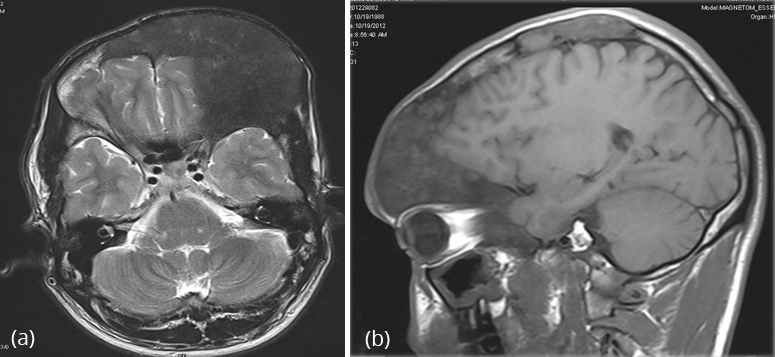
Figure 26a,b: FD MRI – Axial and lateral sections.
Nuclear medicine
Demonstrates increased tracer uptake on Technitium99 MDP bone scans. (Lesions remain metabolically active into adulthood) (Figure 27a,b).

Figure 27: (a) FD – Tracer uptake in right clavicle, (b) FD – Total body nuclide scan - Tracer uptake in right scapula, right radius, right iliac bone and proximal right femur- Polyostotic and unilateral in McCune Albright syndrome.
Prognosis
Usually no treatment is required as the bone lesions usually do not progress beyond puberty. If mass effect is severe, the deformity leads to disability, surgical decompression may be considered.
Complications
Not surprisingly bone affected by fibrous dysplasia is weaker than normal and thus susceptible to pathological fractures. Occasionally, rickets in children and osteomalacia in adults in encountered with fibrous dysplasia due to unknown humoral mechanism (Figure 28a,b).

Figure 28: (a) FD of proximal tibia with rachitic changes with increased distance between metaphysis and epiphysis of tibia, (b) FD metacarpals with rachitic changes, cupping of the radius and ulna of the wrist in a 7 yr old boy.
Differential diagnosis - Tibial lesions
Due to variability of appearance of fibrous dysplasia the potential differential is very long, but will be significantly influenced by the dominant pattern.
Paget's disease
- Radiologically may be similar particularly of the skull
- Different demographics
- Lesion goes to the articular margin
Neurofibromatosis type I
- Vertebral column is primary target
- Ribbon ribs
- Pseudoarthrosis may be common
- Other features of the disease usually present
Osteofibrous dysplasia
Diffusely elongated lesion with multiple loculations.
Fibro osseous dysplasia (ossifying fibroma) (Figure 29)
- Almost exclusively in tibia with anterior bowing
- Lesion begins in cortex
- Usually seen in children <10 years
Cortical fibrous dysplasia of tibia
- Usually cortical, no cystic changes
Adamantinoma
- 80% seen in the tibia
- Age – adolescents and adults
- May appear indistinguishable (Figure 30)

Figure 29: Ossifying fibroma – Note the extensive changes in the tibia simulating FD. Anterior bowing is characteristic.
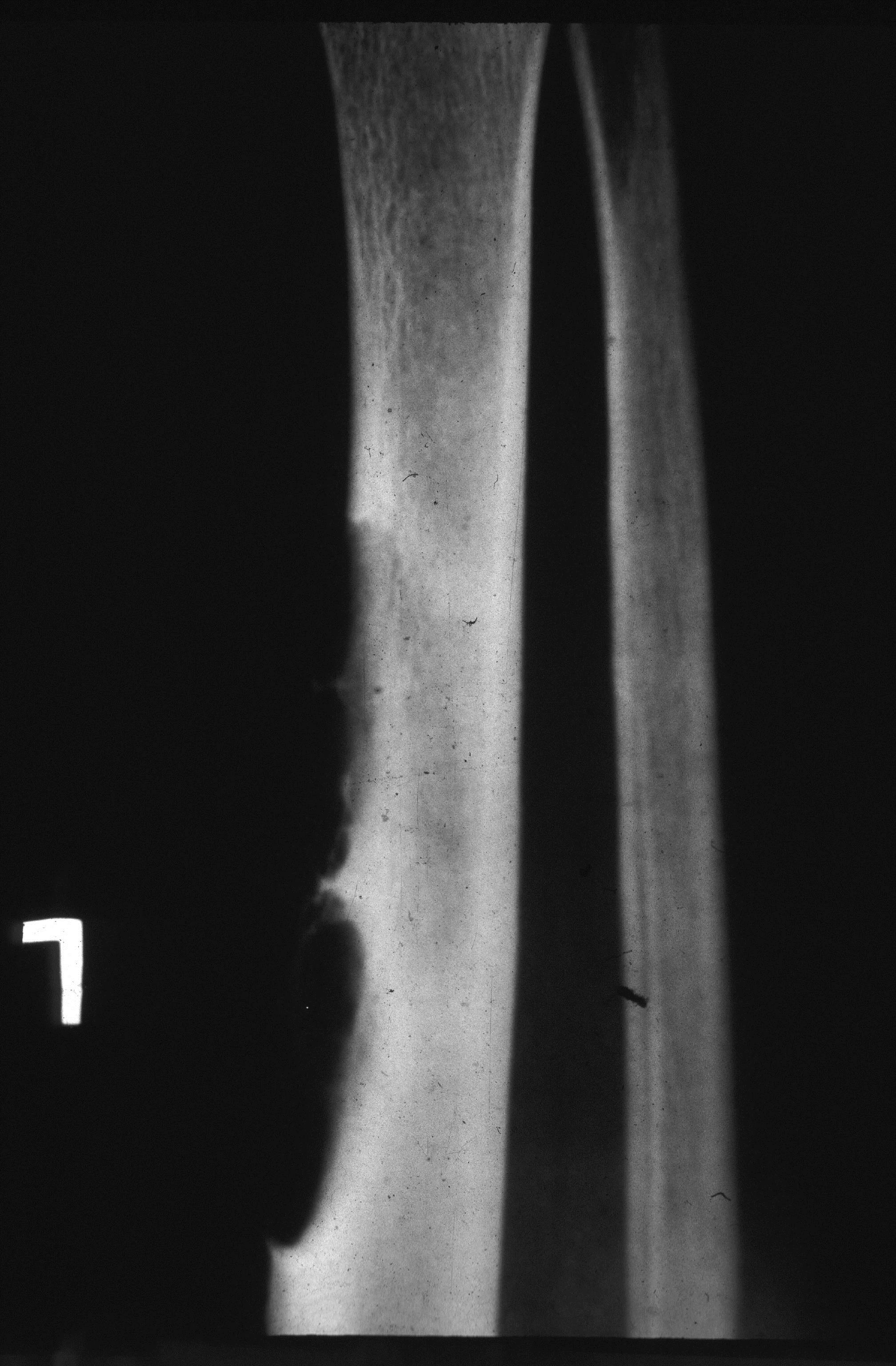
Figure 30: Adamantinoma of the tibia occurs at a later age (20 – 30 yrs). Satelite lesions are common.
To sum up, radiological and imaging findings of fibrous dysplasia constitute a spectrum of manifestations. Monostotic fibrous dysplasia is more common than polyostotic and McCune Albright Syndrome. Complications, deformities and disabilities require surgical management. On going research for genetic nature is conducted in several centres.
Conflicts of interest
Author declares no conflicts of interest.
References
1. Brant WE, Helms CA. Fundamentals of diagnostic radiology. Lippincott Williams & Wilkins 2007.
2. Brown EW, Megerian CA, Mckenna MJ et-al. Fibrous dysplasia of the temporal bone: imaging findings. AJR Am J Roentgenol 1995, 164:679-682.
3. Chong VF, Khoo JB, Fan YF. Fibrous dysplasia involving the base of the skull. AJR Am J Roentgenol 2002, 178:717-720.
4. Dähnert W. Radiology review manual. Lippincott Williams & Wilkins (2007).
5. Edeiken J, Hodes PJ. Roentgen diagnosis of Disease of Bone Baltimore: Williams and Wilkins, 1967.
6. Fitzpatrick KA, Taljanovic MS, Speer DP et al. Imaging findings of fibrous dysplasia with histopathologic and intraoperative correlation. AJR Am J Roentgenol 2004, 182:1389-1398.
7. Greenfield GB. Radiology of Bone Disease (4th ed) Philadelphia: JB Lippincott Co. 1986, 456-58.
8. Kransdorf MJ, Murphey MD. Diagnosis please. Case 12: Mazabraud syndrome. Radiology 1999, 212:129-132.
9. Larheim TA, Westesson P. Maxillofacial Imaging. Springer Verlag, 2008.
10. Maramattom BV. Leontiasis ossea and post traumatic cervical cord contusion in polyostotic fibrous dysplasia. Head & Face Medicine 2006, 2:24. doi:10.1186/1746-160X-2-24.
11. Murry RO, Jacobson HG. The Radiology of Skeletal Disorders (2nd ed) London: Churchill Livingsone, 1977.
12. Warrick LK: Some aspects of polystotic fibrous dysplasia: Knox memorial lecture 1972. Clin Radiol 1973, 24:125-38.