Full Text
Introduction
Metastases (Secondaries) literally means “a placing in the midst of neoplasm remote from the primary”. Metastasis to bone spread by extension, through hematogenous and lymphatic routes. In practice, these metastases may resemble primary bone tumors on imaging. Such lesions include giant cell tumor, brown tumor, pseudo tumor of hemophilia, aneurysmal bone cyst and chondromyxoid fibroma. Even primary tumors such as lytic osteosarcoma and plasmacytoma may simulate blow out metastasis [1]. Image guided biopsy most often distinguishes primary from secondary, although occasionally undifferentiated metastases may pose a problem [2, 3].
Review of the literature
In considering the pathogenesis of the lytic lesion, it is important to look into pathological factors. Majority of tumor emboli are deposited in the bone marrow. Most of these metastatic bone tumors have been present for sometime before they are recognised as perceptible alteration of bone density. Hematogenous dissemination occurs by the spread through blood vessels mainly the veins which are the path ways for tumor emboli. The three major organs which contain metastasis are lung, liver and bones.
In several large postmortem series, it is estimated the incidence of metastases to the bone to be from 22 to 35% of all patients with malignancies. 80% of all metastases have the primary in the lung, breast, genitourinary and gastrointestinal malignancies. About 70% of metastases in women are from breast and uterine cervix [4, 5]. Melanoma also can produce osseous metastases [6, 7].
Discussion
It is often noted that during a routine survey of bones, a large lytic lesion is noted without any known malignancy. At this time, it is a challenge to have a cost effective work up to detect the primary tumor. Another major problem is to assess the metastatic disease in the presence of a known malignancy. It is ideal to have bone scintigraphy to have a total body scan to identify/ rule out metastatic disease. However, total body MRI is the best choice but it is costly and not easily available. Metastatic disease may present as a single or multiple foci of lytic, blastic or mixed pattern. Bone metastases constitute 70% of all malignant bone tumors. Metastases to the bone may be lytic which constitute about 75%. Bone metastasis are seen in 7-28% of follicular thyroid carcinoma patients and 1.4-7% of papillary thyroid carcinoma patients. Bone is the second most common site for metastases from thyroid after lung. Thyroid carcinoma metastases are mostly osteolytic [8]. Sclerotic metastases constitute 15%. Mixed type of both lytic and sclerotic lesions constitute about 10%. Metastases occurring distantly from the origin of the primary malignant tumor is due to molecular mechanism. The spread may be direct extension of the tumor, through lymphatic or through hematogenous routes. Occasionally, metastases may be transplanted during surgery by using the same instruments etc., [9].
Why lytic bone metastases occur and form different morphological changes on imaging is not known. They may be permeative, moth eaten, geographic or ballooned out. The latter is generally solitary but may be at multiple sites. These lesions often arise from the trabecular bone. Cortical metastases are also well known, particularly in carcinoma of lung etc.,
Imaging methods
· Conventional/ Digital
· MDCT
· MRI, MRA
· Scintigraphy
· Pet CT
· Angiography
Role of CT angiography: Bone window settings show high level of details of bone. High vascularity can be detected in CTA.
Role of MRI in metastases: Detects 28% more mets than scintigraphy, focal lytic areas show decreased signal on T1 and increased signal on T2.
Pet CT: Detects many more than actual lesions, because any other non neoplastic lesion can be detected. Hence it is non specific but advantageous to detect the primary also.
Angiography: It is not done as a routine except to embolize a highly vascular and potentially bleedable lesion
In any case, “Early detection is early cure!”
The common primary malignancies that produce ballooned out metastatic lesions arise from thyroid, lung, breast, kidney and melanoma.
Bone metastasis are seen in 7-28% of Follicular thyroid carcinoma patients and 1.4-7% of papillary thyroid carcinoma patients. Bone is the second most common site for metastases from thyroid after lung. Thyroid carcinoma metastases are mostly osteolytic (Figure 1a-g). CTA would help the highly vascular nature (Figure 1h,i,j).
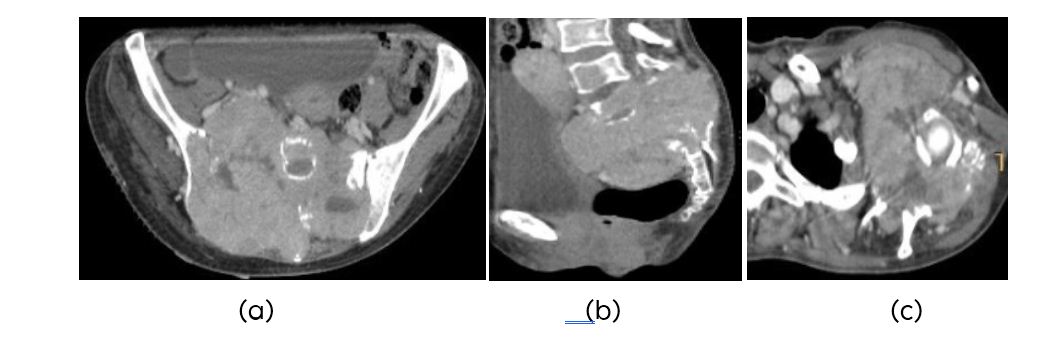
Figure1: (a, b) CT-Follicular carcinoma of thyroid metastasis to sacrum, (c) Scapular metastasis.
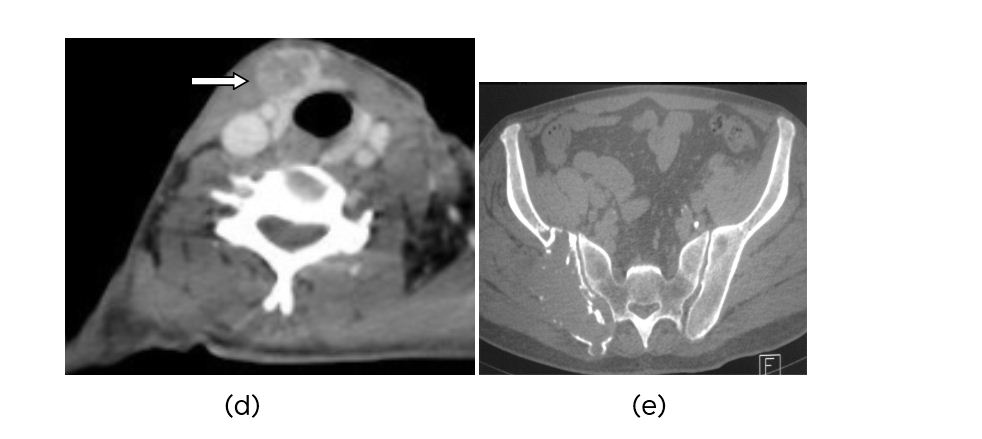
Figure 1: (d) CT-Thyroid nodule, (e) CT-Pelvis showing metastasis.
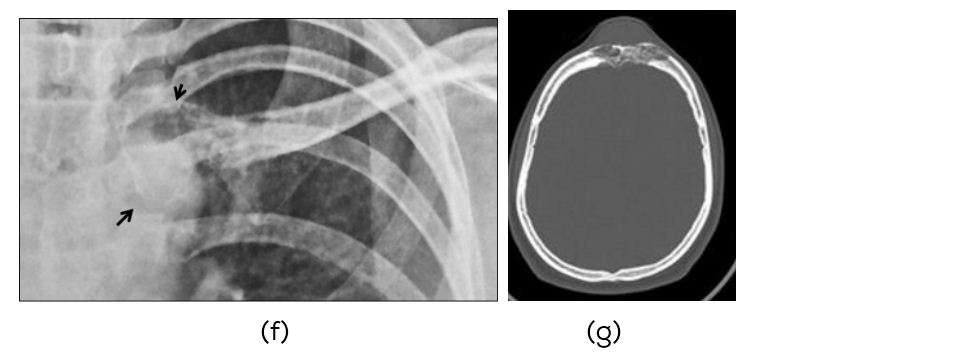
Figure 1: Metastases to the right clavicle and skull from undifferentiated carcinoma of the thyroid: (f) Clinical, (g) Skull.
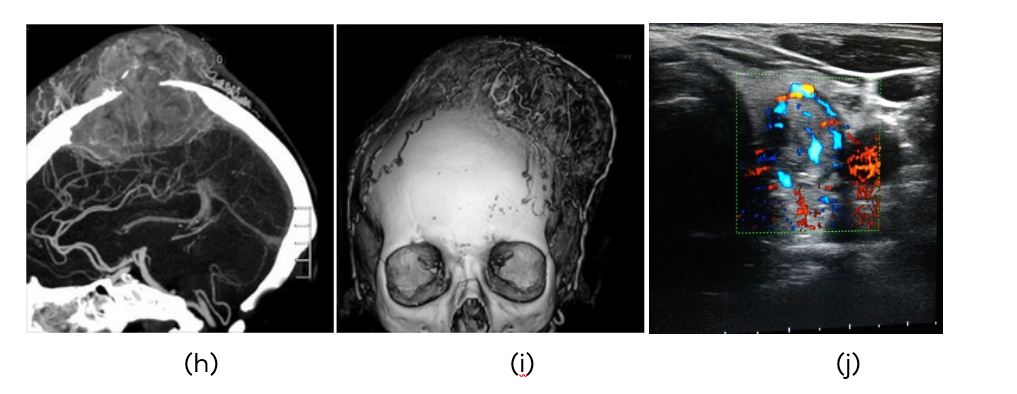 Figure 1: (h, i) CTA metastasis to the skull from thyroid carcinoma, (j) Color doppler of thyroid showing highly vascular tumor.
Figure 1: (h, i) CTA metastasis to the skull from thyroid carcinoma, (j) Color doppler of thyroid showing highly vascular tumor.
Carcinoma of the lung is another malignancy where blow out metastases are common. Plain films are adequate but CT and other imaging methods delineate the nature of matrix (Figure 2a-l).
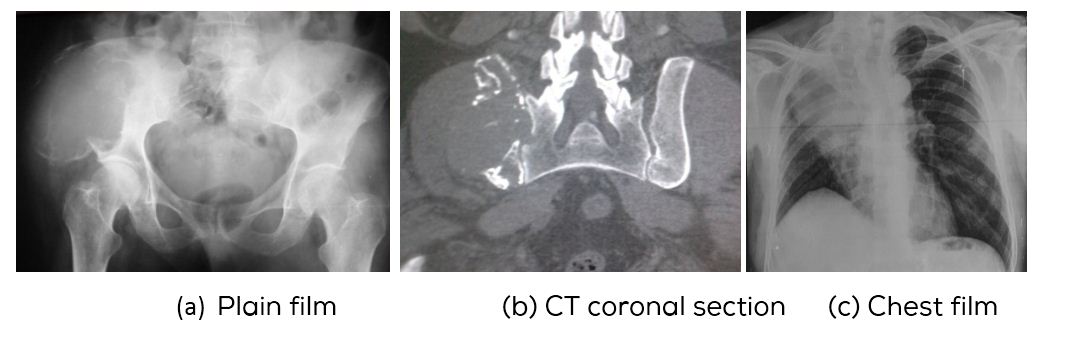
Figure 2: (a) Blowout metastasis, (b) CT right iliac bone, (c) Carcinoma of right upper lobe.
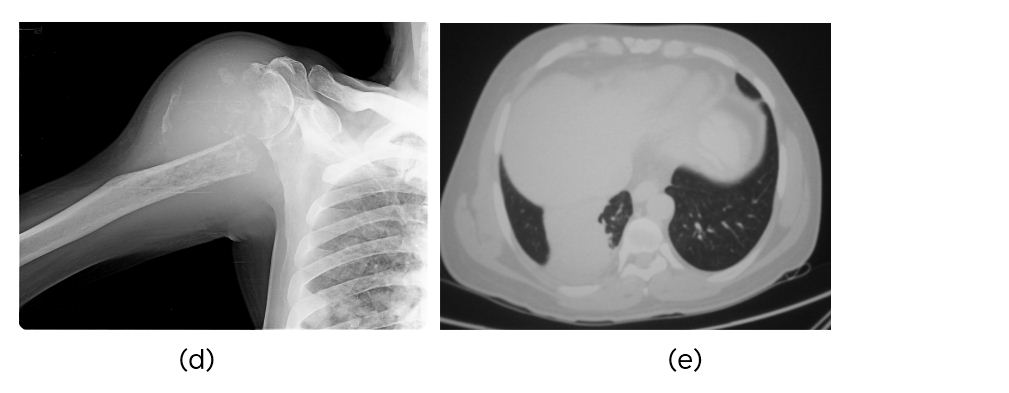
Figure 2: (d) Metastasis to humerus, (e) CT carcinoma of the right lung.
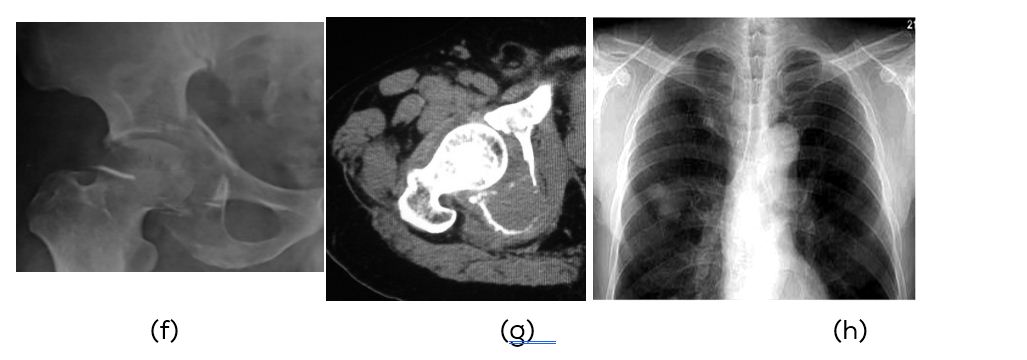
Figure 2: (f) Plain film, (g) CT Metastasis, (h) Primary adenocarcinoma of right lung.
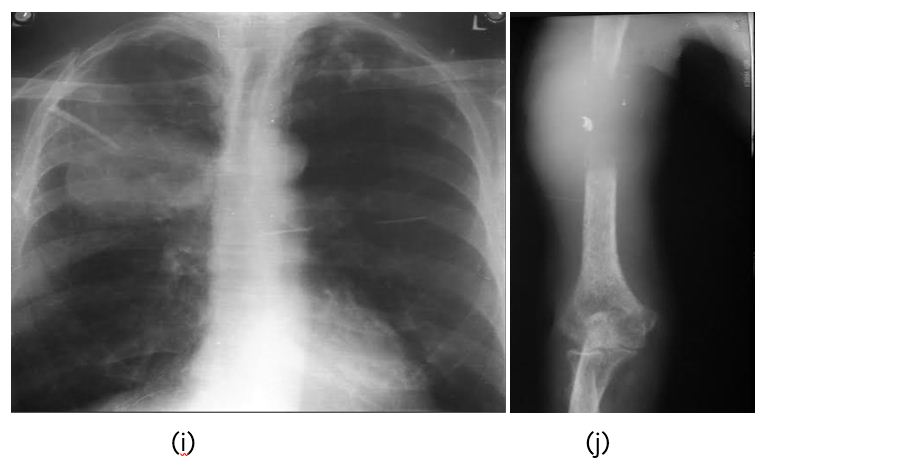
Figure 2: (i) Carcinoma of lung, (j) Metastasis to humerus.
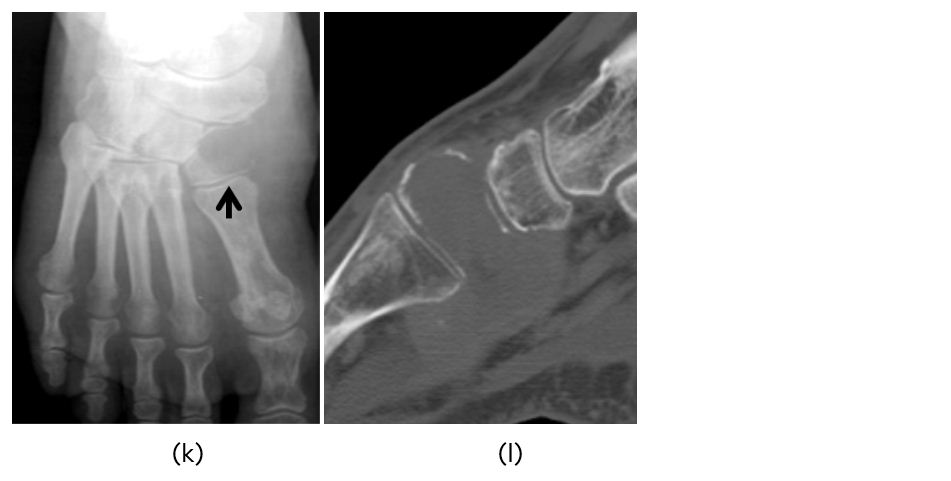
Figure 2k,l: Metastasis to medial cuneiform from carcinoma of the lung.
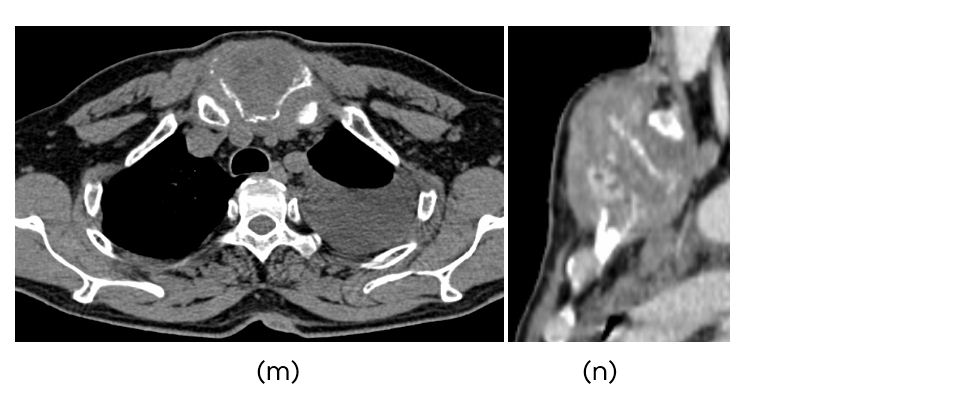
Figure 2: (m) CT showing pleural effusion, (n) Metastasis to sternum from carcinoma of the left lung.
Bone metastases from carcinoma lung occur in 62.5% (ribs>spine). Sternal metastasis from lung cancer-3.8% of which 95% occur in the body 5% in the manubrium part (Figure 2m,n). Sternal metastasis remain solitary, confined to sternum as it does not have contact with parvertebral venous plexus unlike vertebral metastasis which show multicentric lesions. Isolated sternal metastasis from renal cell carcinoma, hepatocellular carcinoma, and breast carcinoma has been reported in the literature.
Blow out metastases from carcinoma of the breast are less common than thyroid and lung. However, occasionally this type of metastasis may be encountered (Figure 3a-d).
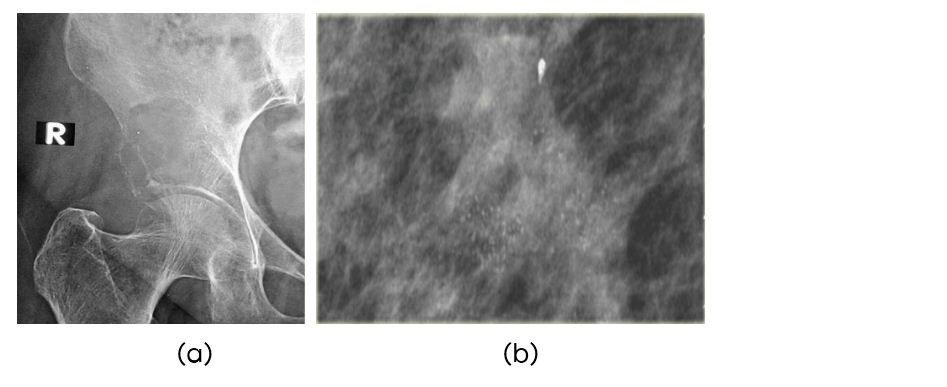
Figure 3: (a) 65-year old female metastasis to ilium, (b) Mammogram showing carcinoma of breast (amorphous calcifications).
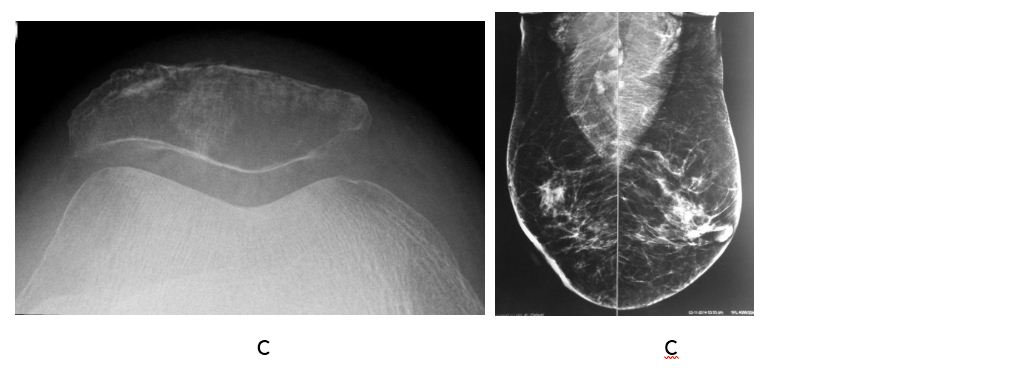
Figure 3: (c) Metastasis to patella, (d) Mammogram showing infiltative duct carcinoma of breast.
Although, melanoma is not a common malignant tumor amongst Indians but blow out metastasis also may be seen in this entity (Figure 4).
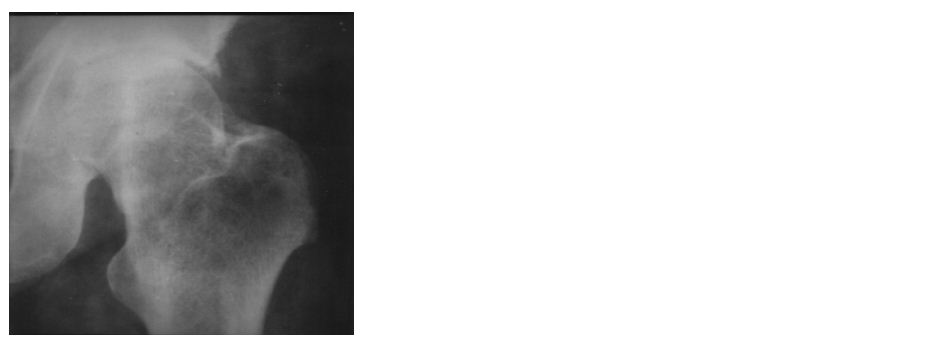
Figure 4: Metastasis to greater trochanter from melanoma of the back.
Literature is filled with case reports of blow out metastases occurring in other malignancies arising from gastrointestinal, head and neck, genitourinary tract and other systems.
MRI depicts the lesion and shows different components of the tumor (Figure 5a,b).

Figure 5: (a) 55-year-old female head of the humerus, (b) MRI showing metastasis from carcinoma of breast.
Role of radionuclide scanning in metastases
Valuable imaging modality with technetium phosphate compounds. Highly sensitive for lytic lesions. However, it is non specific. A solitary focus of increased radio activity is seen in 10% of metastases [10, 11] (Figure 6a,b).
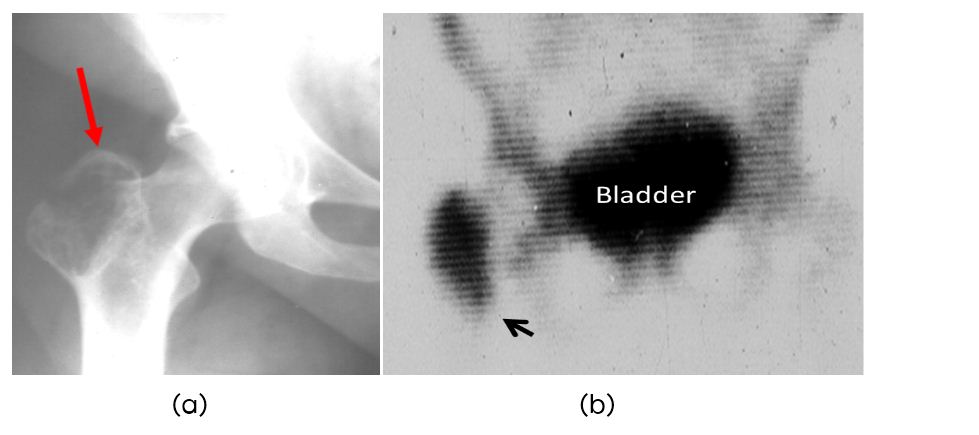
Figure 6: Metastasis to greater trochanter from carcinoma of breast. (a) Plain film, (b) Scintigraphy.
Differential diagnosis
In the differential diagnosis of blow out metastases, the following primary malignant and benign lesions come into consideration. These are listed in Table 1.
Table 1: Differential diagnosis of blow out metastases.
|
· Primary malignancies of the bone, lytic osteogenic sarcoma etc (Figure 7).
· Plasmacytoma (Figure 8)
· Aggressive giant cell tumor (Figure 9)
· Aneurysmal bone cyst (Figure 10)
· Simple bone cyst (Figure 11)
· Brown tumor (Figure 12)
· Pseudo tumor of hemophilia (Figure 13)
· Chondromyxoid fibroma (Figure 14)
|
Benign tumors and tumor like bone lesions with blow out appearance include giant cell tumor, aneurysmal bone cyst, simple bone cyst, brown tumor, pseudo tumor of hemophilia and chondromyxoid fibroma [12].
To differentiate primary malignancies of the bone, certain criteria such as, site, age, aggressive nature, transitional zone, matrix mineralisation and soft tissue swelling should be considered. Metastasis may occur in any part of the bone whereas most of the primary malignancies occur in the metaphyseal zone. Beyond the age of 45 years, plasmacytoma and lymphoma are the only primaries producing lytic changes. Otherwise metastasis should be considered. The transitional zone in metastasis is usually thin. The matrix is lucent in lytic metastasis. Unless there is pathological fracture soft tissue swelling is usually not present in metastasis.

Figure 7: Osteosarcoma of femur lytic type.
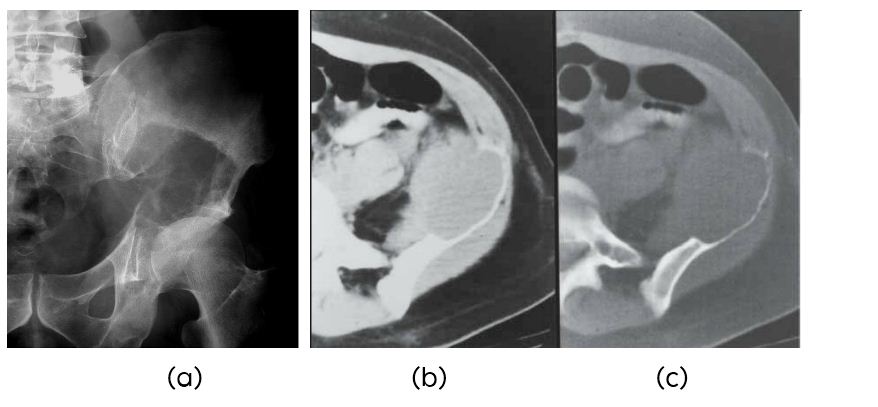
Figure 8: 52 years - Plasmacytoma of left iliac bone: (a) Plain film, (b, c) CT.

Figure 9: 25-years-old female - Giant cell tumor of calcaneum.
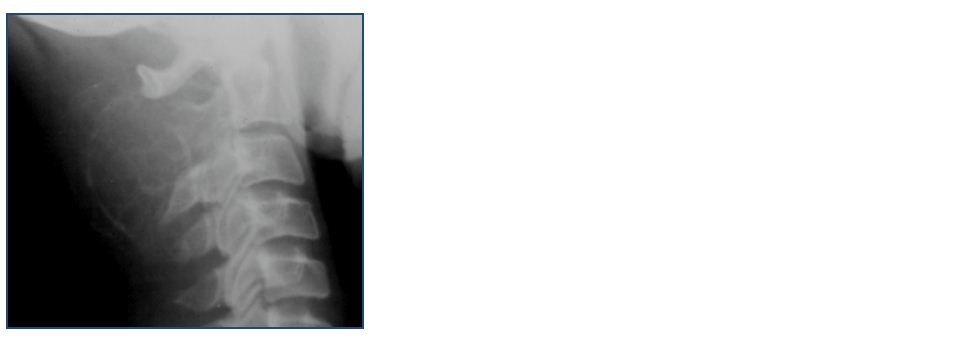
Figure 10: Aneurysmal bone cyst involving spinous process of C2. Note the thin shell of cortex.

Figure 11: Simple bone cyst in a 8-year-old.
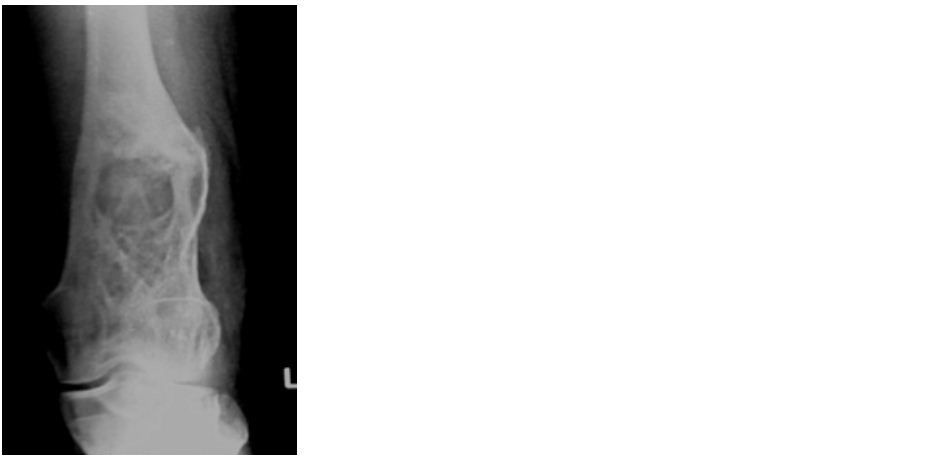
Figure 12: Brown tumor in hyperparathyroidism.
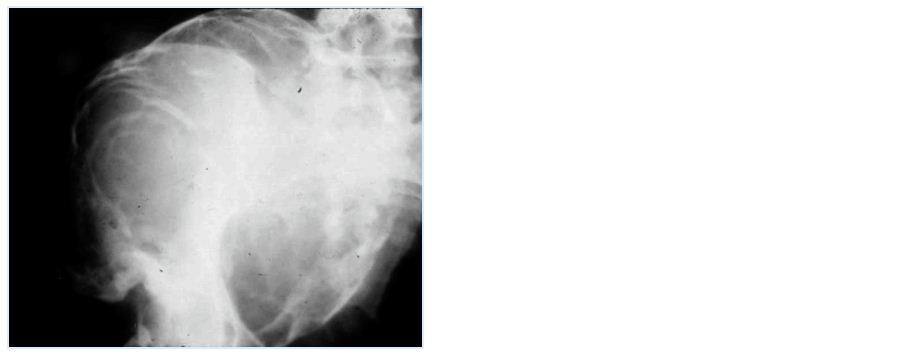
Figure 13: Hemophilic pseudotumor involving iliac bone.

Figure 14: 27-year-old male - Chondromyxoid fibroma in the tibia.
Conclusion
In medical practice, particularly in orthopedic oncology, ballooned out lesions of bone are often encountered. The metastatic blowout lesion is often solitary. These should be distinguished from primary bone tumors as well as tumor like lesions. The radiological criteria for the diagnosis of primary bone tumors are mentioned. A blow out lesion of bone is an indication to search for primary lesion, in the thyroid, lung, breast, kidney etc.
Acknowledgements
NIMS; KIMS and KREST Museum, Hyderabad, India.
Conflicts of interest
The author declares no conflicts of interest.
References
[1] Subbarao K. Imaging approach to malignant bone tumors. Nepalese Journal of Radiology 2013; 3(1): 1–13.
[2] Rosenthal DI. Radiologic diagnosis of bone metastases. Cancer 1997; 80 (Issue Supplement S8):1595–1607.
[3] Simon MA, Bartucci EJ. The search for the primary tumor in patients with skeletal metastases of unknown origin. Cancer 1986; 58(5):1088–1095.
[4] James H, Thrall. Diagnostic imaging in bone disease. Radiol Clin North Am. 1987; 25(6):1049–1288.
[5] Choufani E, Diligent J, Galois L, Mainard D. Metastatic renal cell carcinoma presenting as foot metastasis: case report and review of the literature. J Am Podiatr Med Assoc. 2011 May;101(3):265–268.
[6] Forbes GS, McLeod RA, Hattery RR. Radiographic manifestations of bone metastases from renal carcinoma. AJR Am J Roentgenol. 1977;129(1):61–66.
[7] Jash D, Saha K, Maji A, Agarwal S. Bronchogenic carcinoma presenting as solitary sternal metastasis. 2013; 2(3): 243–245.
[8] Wu K, Hou SM, Huang TS, Yang RS. Thyroid carcinoma with bone metastases: a prognostic factor study. Clin Med Oncol. 2008; 2:129–34.
[9] Fon GT, Wong WS, Gold RH, Kaiser LR. Skeletal metastases of melanoma: radiographic, scintigraphic, and clinical review. AJR Am J Roentgenol. 1981;137(1):103–108.
[10] McDougal IR. Skeletal scintigraphy. West J Med. 1979; 130(6): 503–514.
[11] Healey JH, Turnbull AD, Miedema B, Lane JM. Acrometastases. A study of twenty-nine patients with osseous involvement of the hands and feet. J Bone Joint Surg Am. 1986; 68(5):743–746.
[12] Miller TT. Bone tumors and tumorlike conditions: analysis with conventional radiography. Radiology. 2008; 246(3):662–74.