Full Text
Introduction
Common cartilaginous lesions of synovium include primary synovial chondromatosis (PSC) also known as Reichel syndrome, and secondary synovial chondromatosis (SSC) [1]. Histologically proved chondrosarcomas of the synovium either de novo or secondary to previously existing synovial chondromatosis is rarely encountered. In PSC, multiple nodules of varying size of metaplastic hyaline cartilage are noted [2, 3]. Quite often, these cartilaginous nodules may ossify and hence the term synovial osteochondromatosis is interchangeably used. Any synovial joint or synovial sheath of tendon or a bursa may be involved [4]. Generally, it is monoarticular but multiple joint involvement has been described [5]. SSC is often the sequalae of degenerative joint disease. This results in intra-articular loose bodies as a result of trauma, osteoarthritis, or neuropathic arthropathy. It is quite distinct from PSC and presents a different imageological pattern.
Imaging methods
• Conventional/ Digital
• Arthrography
• Ultrasonography/Color Doppler
• MDCT
• MRI
• Radionuclide scanning
• PET CT
Imaging characteristics and review of the literature
PSC has been described in detail with radiological characteristics by several authors [1-3]. This disorder may manifest at any age without any sex preference. Clinically the patient may complain of pain, swelling or disability in moving the involved joint. In general, no previous history of trauma is elicited.
Conventional radiography
This reveals characteristic multiple intraarticular calcifications. These are mostly of similar size and shape. They may be localised or distributed throughout the joint, extend into the synovial recesses or extend along the synovial sheath of the tendon [4]. Similar appearances are seen when encountered in bursa. Although, it is monoarticular, few reports were published regarding their polyarticular nature [5]. The calcifications may be nodular, ring or arc like. Radiologically it is difficult to differentiate between calcification and ossification, unless the cortex and medulla are distinctly outlined. Extrinsic erosion of the adjacent bone is seen in some cases [6-9]. When clinically suspected particularly in the region of the hip joint, the plain films may or may not show calcifications but the erosions surrounding the neck of the femur, in the shape of “apple-core” defect are suggestive of this diagnosis. However, the “apple-core” defect of the femoral neck may also be noted in pigmented villonodular synovitis, amyloidosis,chronic tubercular and rheumatoid arthritis [6, 7].
Contrast arthrography
This is an ideal imaging method to show the filling defects in the synovial cavity which is filled with contrast. However, the filling defects are not specific for chondromatosis. In addition, it is an interventional procedure. Hence, it is not very popular, specially after the introduction of Multi detector computed tomography (MDCT).
Ultrasonography
It is not commonly used except in situations where the calcifications of the chondromatous bodies are not depicted on conventional films. It reveals small heterogeneous nodules containing foci of hyperechogenicity. It may help to observe the mobility of these foci when they are loose. It may also help in identifying the extra-articular extent of the lesion [10]. Color Doppler plays a role only in identifying their avascular nature.
Multi detector computed tomography
It is optimal in depicting the mineralized intraarticular bodies as well as the extrinsic bone erosion [11]. Variable sizes of thickened synovium are noted. The large calcified bodies may have radiolucent centres due to incomplete calcification/ossification.
Magnetic resonance (MR)
MR imaging helps in detecting the extent of the synovial disease and the surrounding soft tissue involvement. The signal intensity with T1 weighting is low to intermediate intensity, while T2 shows hypo intensity [12].
Radionuclide scanning
Radionuclide scanning is helpful very rarely [13]. Unless adequate mineralization is present, the lesions may not be picked up by the isotope Technetium99.
PET CT
PET CT is rarely used.
Malignant transformation of PSC or SSC to chondrosarcoma is very rare. However, few reports have been found in the literature [14, 15]. Malignancy is suspected when there is recurrence or when the adjacent bone narrow is involved.
SSC is often encountered in the elderly since degenerative joint disease is common at this age. This is due to trauma to the intraarticular hyaline cartilage, menisci and synovium. It is also encountered in secondary degenerative joint disease, neuroarthropathy and osteochondral fractures. Rarely it may be the result of osteonecrosis of the bones of the joint. It manifests most commonly in the knee, hip and other major joints. Radiologically, these are loose bodies and are larger and they are not continuous as noted in PSC. They are rarely seen beyond the synovial space of the joint and the underlying pathology of the joint indicates its nature [16, 17].
Discussion
Synovial cartilaginous lesions are either primary or secondary. The etiology of PSC is not exactly known, although genetic studies reveal some of the major factors involved. Pathologically it is a neoplastic process which is benign in nature. The hyaline cartilage nodules are formed in the subsynovial tissue of a joint or synovial sheath of the tendon or bursae. These synovial nodules may be detached may get conglomerate. Imaging findings particularly with conventional radiography are pathognomonic and show multiple intraarticular calcifications in the shape of nodules, arcs or circles. Prior to the stage of mineralization, conventional radiography, ultrasonography and contrast arthrography may be of help (Figures 1a-l).
A summary of imaging findings is noted in the Table 1:
Table 1: Primary synovial chondromatosis.
|
Ø Multiple round calcified nodules of similar size and variable calcification.
Ø The size may range from tiny speckled calcifications to large round, lamellated cartilage or ossified nodules.
Ø These nodules may form a conglomerate mass rather than free-floating.
Ø Degree of calcification is variable.
Ø Associated erosions may be seen as an apple-core deformity in the neck of the femur.
Ø MR signal depends upon the degree of mineralisation.
Ø Malignant transformation is extremely rare.
|

Figure 1: Primary synovial osteochondromatosis: (a) knee joint; (b) infrapatellar bursa; (c) hip joint; (d) apple-core; (e) femoral neck with erosions.

Figure 1: Primary synovial chondromatosis: (f) wrist; (g) elbow; (h) conventional; (i) CT.
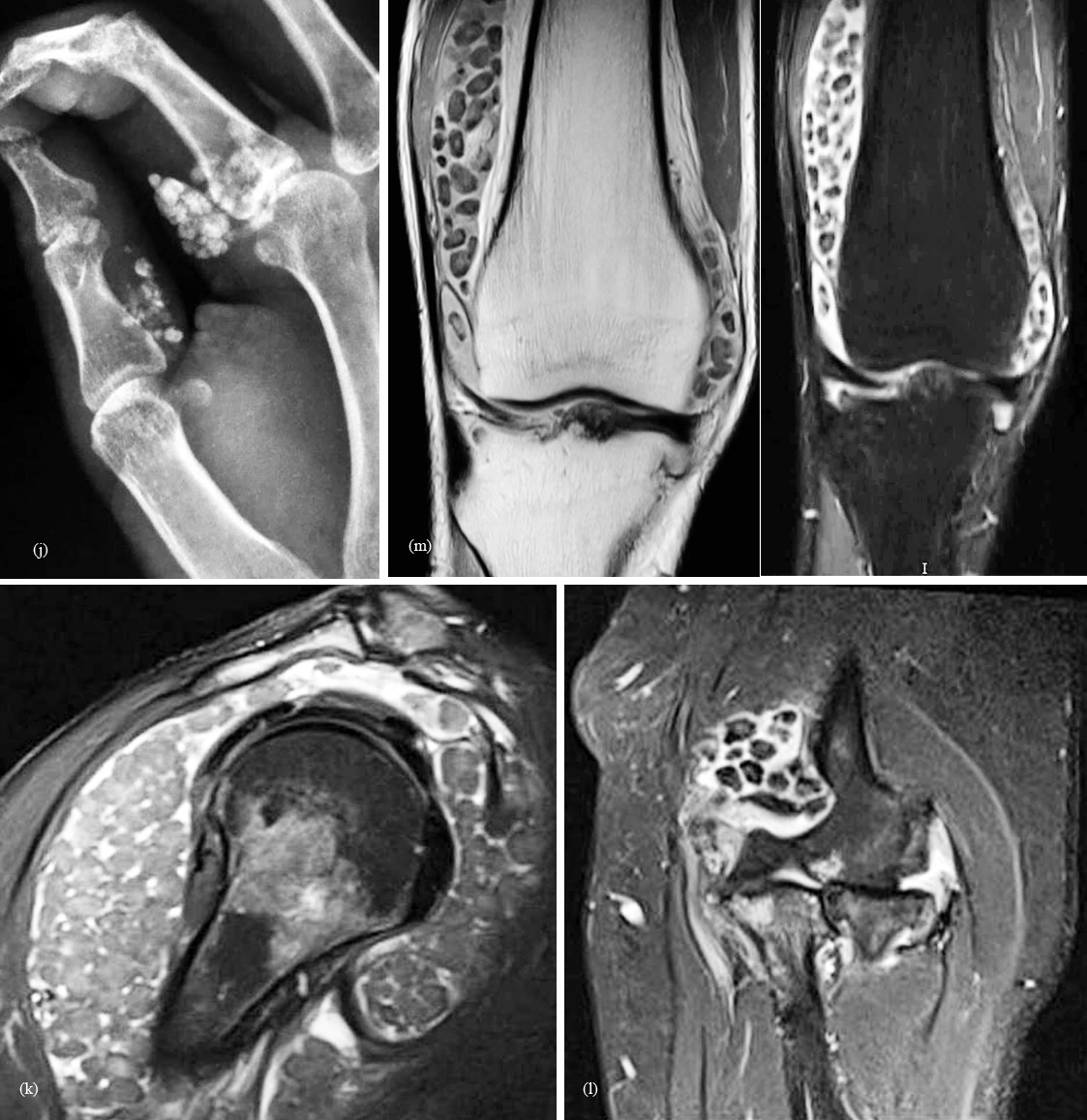
Figure 1: (j) Polyarticular primary synovial chondromatosis in the hand; (k) shoulder; (l) elbow; (m) MRI synovial chondromatosis of the knee.
Secondary synovial chondromatosis (SSC)
SSC is a disorder that results in intra-articular loose bodies as a result of trauma, osteoarthrosis, or neuropathic arthropathy. It is quite distinct from PSC. Pathologically concentric rings of growth may be seen scattered in the joint (Figure 2a, b, c, d). These are also called “Joint mice”. MRI clearly depicts the large osteochondral bodies (Figure 2e).
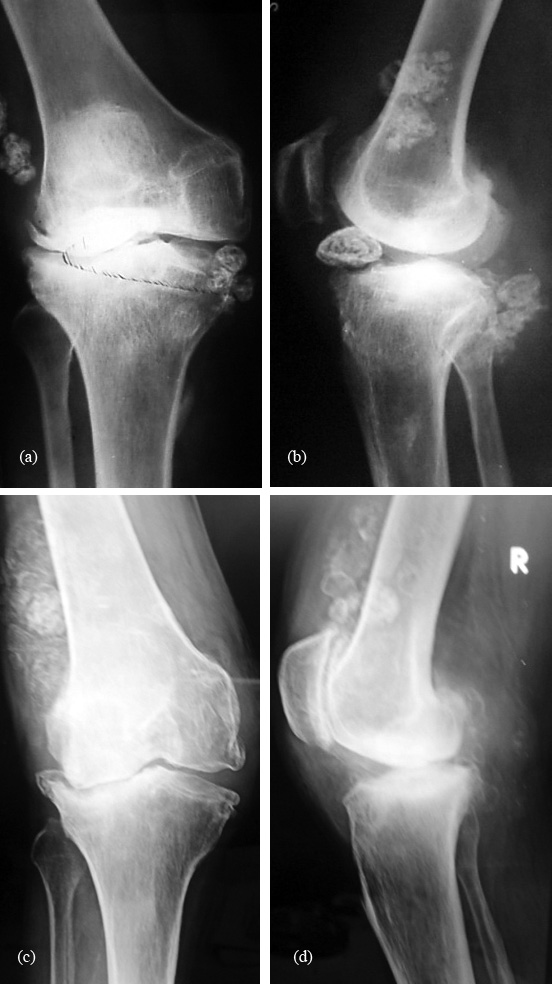
Figure 2a-d: Secondary osteochondromatosis of the knee due to degenerative changes (joint mice).

Figure 2e: MRI T2 secondary osteochondramotosis.
Differential diagnosis
A number of proliferative synovial disorders may simulate synovial chondromatosis, specially in the absence of mineralisation. Pigmented villonodular synovitis (PVNS) is a rare benign proliferative disorder affecting synovial membranes of joints, bursae or tendons resulting from possibly neoplastic synovial proliferation with villous and nodular projections and haemosiderin deposition. PVNS is most commonly mono articular (80% knee joint) but occasionally it can be oligoarticular. Radiographic appearances of PVNS vary by the subtype, localized or diffuse, and the specific joint involved with intraarticular lesions [18]. The localized extra-articular subtype of this disease is called Pigmented villo nodular teno synovitis (PVNTS) or Pigmented villo nodular bursitis (PVNB). It typically manifests as a soft-tissue mass in 50% - 70% of cases. Extrinsic erosion, often with well-defined sclerotic margins, of the underlying bone is the most common osseous abnormality, seen in 9% - 25% of cases. This feature appears more often in lesions of the foot or ankle, owing to the overlying dense ligaments that restrict outward growth of lesions.
Radiographs demonstrate joint effusion, soft-tissue swelling, absence of calcification, extrinsic erosion of bone, preservation of joint space, and normal bone mineralization. Extrinsic erosion of bone and sub-chondral lucent areas are well-defined geographic lesions that frequently display a rim of sclerosis and that involve both sides of the joint. The knee joint, because of its large capacity that allows extension and decompression of normal tissues into multiple adjacent bursal regions (such as the suprapatellar and gastrocnemius/semimembranosus bursae), is less frequently affected by extrinsic erosion of bone (Figure 3). The major difference between synovial chondromatosis and PVNS is the total absence of calcifications of the synovium in the latter. Magnetic resonance imaging may show low-signal intensities and blooming artifacts may simulate PSC, but the low-signal intensities are not as low as seen in PSC and also the morphology is different depicting the villous nature.
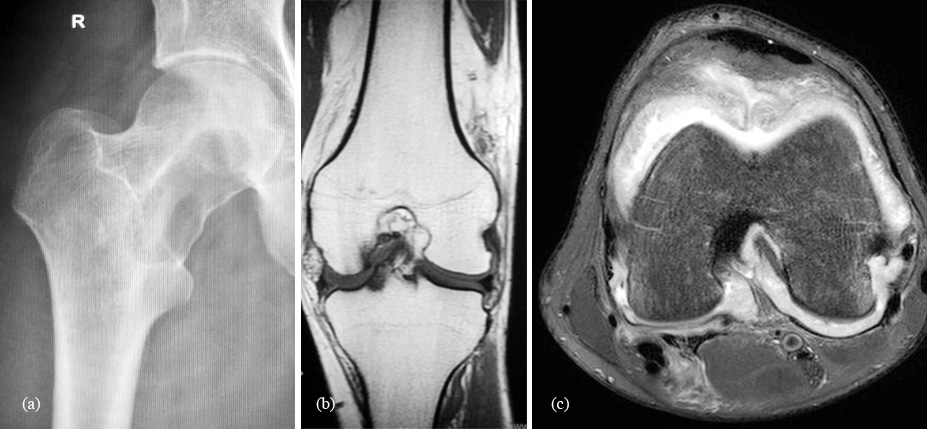
Figure 3: Pigmented villo nodular synovitis: (a) femoral neck; (b) and (c) MRI of the knee
Synovial hemangioma
It is rare and represents a benign malformation of blood vessels on the synovial lined surface. Radiologically, in about 50% of the patients phleboliths may be noted on plain films. The phleboliths have central lucency surrounded by calcification. Associated effusion, erosions and periosteal reaction may be noted (Figure 4). In children early maturation of the epiphysis may be observed [19, 20]. MRI reveals the vascular nature of the lesion.
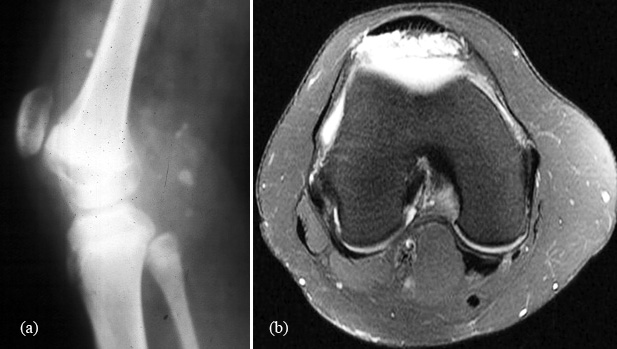
Figure 4: Synovial hemangioma of the knee: (a) note the phleboliths; (b) leash of vessels seen in MRI.
Lipoma arborescence
It is a benign synovial lesion characterised by proliferative fat cells in the sub-synovial tissue. It generally involves suprapatellar pouch of the knee joint, but also encountered in other joints. Radiologically, it is difficult to diagnose it on plain films. With ultrasonography and MRI the diffuse frond-like proliferation can be clearly seen (Figure 5). The characteristic feature on MR imaging particularly in fat suppressed and in STIR sequences is diagnostic. Originally described by Hoffa, the macrospic frond-like appearance was considered to resemble a tree in leaf; hence, the Latin term arborescens (meaning “tree-forming” or “treelike”). The knee is the most commonly involved joint. MRI is the modality of choice for diagnosis; the frond-like lesion follows the signal intensity of fat on all sequences [21].
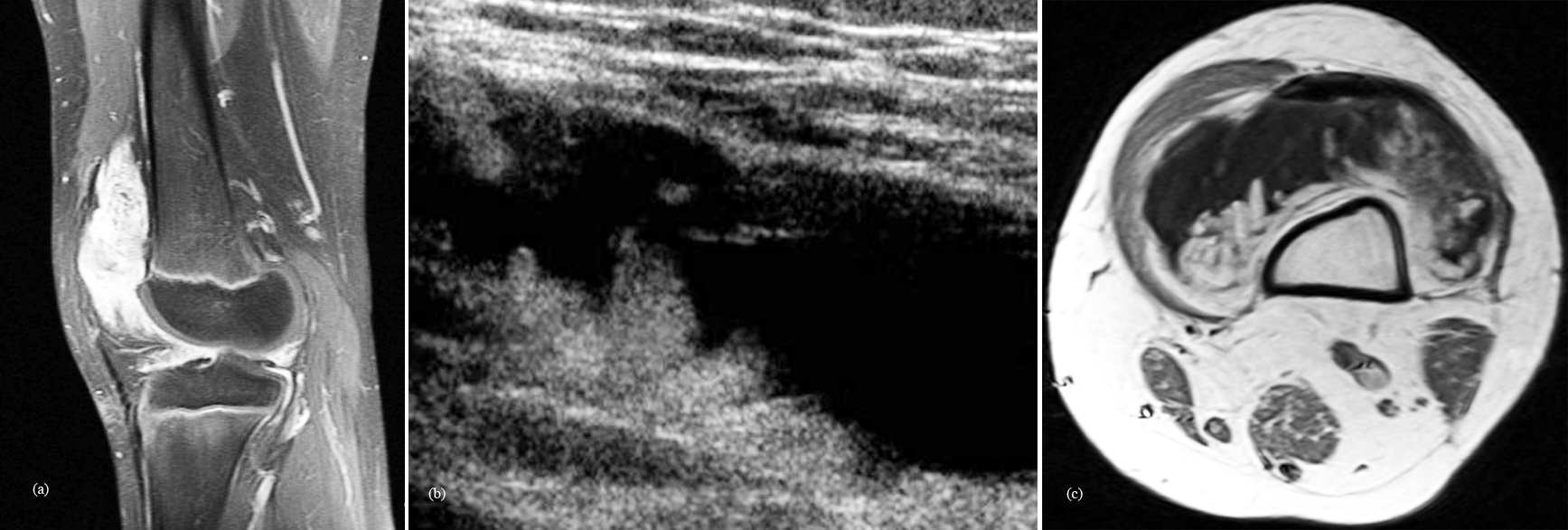
Figure 5: Lipoma arborescens of the knee: (a) MRI; (b) Ultrasonography; (c) MRI T1.
Chronic tuberculosis of the joints
In tuberculosis of the joints, synovial proliferation is common with caseous granulations resembling melon seed bodies, rice bodies or millet seeds. Plain films are not helpful but ultrasonography and MRI may reveal the typical appearance of hyperintensity of the nodules. Even without bone involvement, these bodies may be seen in tuberculous bursitis (Figure 6) [22, 23].
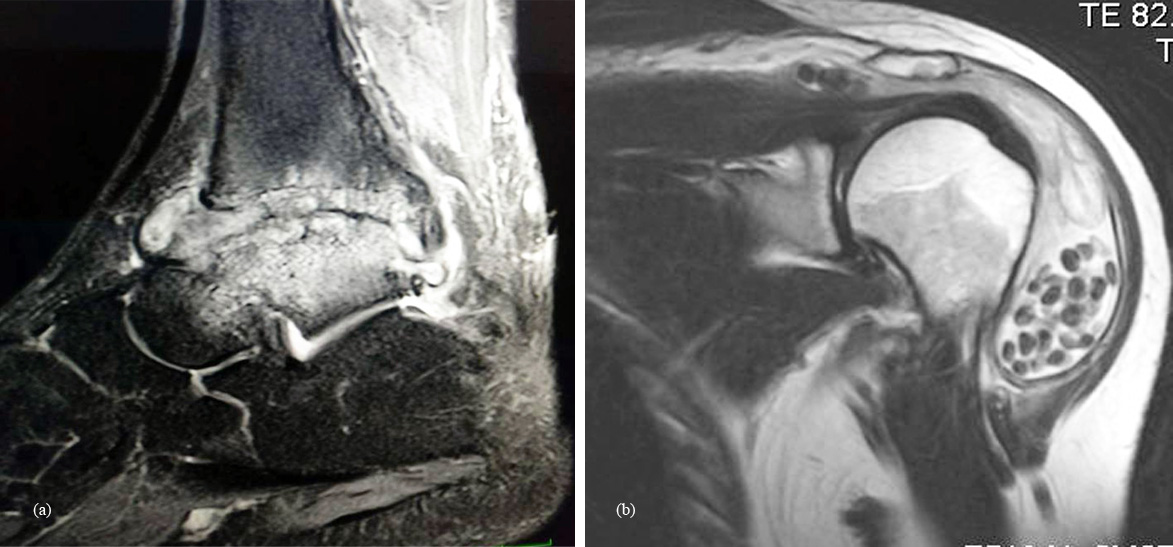
Figure 6: Tuberculosis: (a) ankle; (b) shoulder.
Neuroarthropathy
The etiologies of neuropathic arthropathy are varied. Majorly, two types of neuroarthropathy are noted, 1) Hypertrophic 2) Atrophic. In hypertrophic type the joint is subluxated, fragmentation of bone occurs with synovial thickening and calcific debris (Figure 7). This calcific debris may resemble synovial chondromatosis. However, the additional radiological findings differentiate between these two entities [24].

Figure 7: Neuropathic shoulder with calcific debris.
Chronic rheumatoid arthritis
In chronic RA, hypertrophic synovial nodules are sometimes noted, simulating other types of proliferative synovitis (Figure 8).
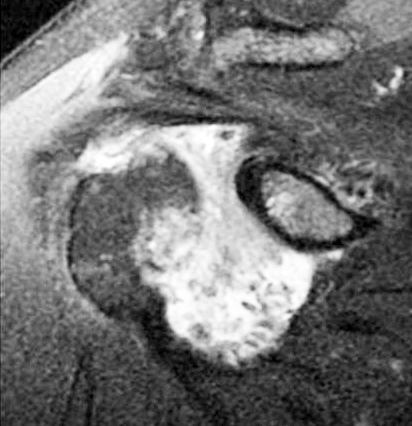
Figure 8: Rheumatoid arthritis of the shoulder MRI, note the hypointense nodules.
Crystal arthropathies
These include crystal deposition such as, hydroxy apatite, monosodium urate, calcium oxalate and calcium pyrophosphate dihydrate crystals in the periarticular tissues (Figure 9). However, the site of calcifications and morphology of calcifications differ from SSC [25].

Figure 9: Calcific tendinitis of the shoulder.
Conclusion
Cartilaginous lesions of the synovium majorly include primary synovial chondromatosis and secondary synovial chondromatosis. Chondrosarcoma of the synovium is very rare. Imaging wise, conventional, CT and MRI play a major role in the diagnosis. In the differential diagnosis, other proliferative synovial disorders such as pigmented villonodular synovitis, lipoma arborescence, chronic rheumatoid and tubercular arthritis should be included. In secondary synovial chondromatosis, degenerative joint disease and neuroarhropathy should be considered in the differential. Crystal deposition disorders such as Calcium Pyrophosphate Dihydrate Crystal Deposition Disease (CPPD), gout, hydroxy apatite and calcium oxalate crystal diseases may be considered.
Acknowledgements
NIMS, KIMS and KREST Museum of Hyderabad.
Conflicts of interest
Author declares no conflicts of interest.
References
[1] Jaffe HL. Tumours and tumorous conditions of bones and joints, 1st edition. Lea & Fabiger. Philedelphia, USA. 1958; 558–567.
[2] John X, Connell O, MB, FRCPC. Pathology of the synovium. American society of clinical pathologists. 2000; 114:773–784.
[3] Miller MV, King A, Mertens F. Synovial chondromatosis. In: Flethcer CDM, Unni KK. Pathology and genetics of tumors of soft tissue and bone. IARC, Lyon, France. p246.
[4] Sim FH, Dahlin DC, Ivins JC. Extra-articular synovial chondromatosis. J Bone Joints Surg Am. 1977; 59(4):492–495.
[5] Seckley J, Anderson SG, Snow TM, Benjamin M. A rare case of polyarticular synovial osteochondromatosis. J Anat. 2002; 200(5):523–534.
[6] Norman A, Steiner GC. Bone erosion in synovial chondromatosis. Radiology. 1986; 161(3):749–752.
[7] Goldberg RP, Weissman BN, Naimark A, Braunstein E. Femoral neck erosions: sign of hip joint synovial disease. AJR Am J Roentgenol. 1983; 141(1):107-111.
[8] Crotty JM, Monu JU, Pope TL. Synovial osteochondromatosis. Radiol Clin North Am. 1996; 34(2):327–342.
[9] Murphey MD, Vidal JA, Fanburg-Smith JC, Gajewski DA. Imaging of synovial chondromatosis with radiologic-pathologic correlation. Radiographics. 2007; 27(5):1465–1488.
[10] McKenzie G, Raby N, Ritchie D. A pictorial review of primary synovial osteochondromatosis. Euro Radiol. 2008; 18(11):2662–2669.
[11] Burnstein MI, Fisher DR, Yandow DR, Hafez GR, De Smet AA. Case report 502: Intra-articular synovial chondromatosis of shoulder with extra-articular extension. Skeletal Radiol. 1988; 17(6):458–461.
[12] Ginaldi S. Computed tomography feature of synovial osteochondromatosis. Skeletal Radiol. 1980; 5(4):219–222.
[13] Narváez JA, Narváez J, Ortega R, De Lama E, Roca Y, et al. Hypointense synovial lesions on T2-weighted images: differential diagnosis with pathologic correlation. AJR Am J Roentgenol. 2003; 181(3):761–769.
[14] Shanley DJ, Evans EM, Buckner AB, Delaplain CB. Synovial osteochondromatosis demonstrated on bone scan: correlation with CT and MRI. Clin Nucl Med. 1992; 17(4):338–339.
[15] Kenan S, Abdelwahab IF, Klein MJ, Lewis MM. Case report 817: Synovial chondrosarcoma secondary to synovial chondromatosis. Skeletal Radiol. 1993; 22(8):623–626.
[16] Wittkop B, Davies AM, Mangham DC. Primary synovial chondromatosis and synovial chondrosarcoma: A pictorial review. Eur Radiol. 2002; 12(8):2112–2119.
[17] Villacin AB, Brigham LN, Bullough PG. Primary and secondary synovial chondrometaplasia: Histopathologic and clinicoradiologic differences. Hum Pathol. 1979; 10(4):439–451.
[18] Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, et al. Pigmented villonodular synovitis: Radiologic – pathologic correlation. Radioographics. 2008; 28(5):1493–1518.
[19] Greenspan A, Azouz EM, Matthews J, Décarie JC. Synovial hemangioma: Imaging features in eight histologically proven cases, review of the literature and differential diagnosis. Skeletal Radiol. 1995; 24(8):583–590.
[20] Devaney K, Vinh TN, Sweet DE. Synovial hemangioma a report of 20 cases with differential diagnostic considerations. Hum Pathol. 1993; 24(7):737–745.
[21] Vilanova JC, Barceló J, Villalón M, Aldomà J, Delgado E, et al. MR imaging of lipoma arborescens and the associated lesions. Skeletal Radiol. 2003; 32(9):504–509.
[22] Woon CY, Phoon ES, Lee JY, Puhaindran ME, Peng YP, et al., Rice bodies, millet seeds, and melon seeds in tuberculous tenosynovitis of the hand and wrist. Ann Plast Surg. 2011; 66(6):610–617.
[23] Pimprikar MV, Kekatpure AL. Subdeltoid bursa tuberculosis with rice bodies formation: Case report and review of literature. J Orthop Case Rep. 2014; 4 (2):57–59.
[24] Subbarao Kakarla. Radiology of Neuroarthropathy. JMSR. 2014; 2(4):203–208.
[25] Subbarao Kakarla. Radiology of crystal arthropathies. JMSR. 2015; 3(4):187–191.