Full Text
Introduction
Primary tumors of sacrum are rare. Metastatic tumors are more common due to the abundant hemopoietic tissue. Neural tumors and cysts are not included in this paper. The most common malignant tumor of the sacrum is chordoma. Metastasis from chordoma are rare. The benign tumors, such as osteoid osteoma, osteoblastoma, osteochondroma are also rare. However, giant cell tumor and aneurysmal bone cysts are encountered not quite so rarely. The imaging features of malignant tumors are described in the discussion [1]. Although conventional radiography gives a clue to a diagnosis, further advanced imaging is necessary to arrive at a final diagnosis. However, in some benign and malignant tumors, histopathological confirmation is necessary.
Imaging methods
- Conventional radiography
- CT
- MRI
- Radionuclide scanning
- PETCT
Classification of tumors
- Benign
- Giant cell tumor: 2nd most common primary sacral tumor
- Aneurysmal bone cyst
- Osteoid osteoma
- Osteoblastoma: accounts for ~17% of spinal osteoblastoma(s)
- Osteochondroma
- Hemangioma Sacro coccygeal teratoma
- Malignant
- Sacral chordoma
- Chondrosarcoma
- Ewing sarcoma
- Osteosarcoma Plasmacytoma/multiple myeloma
- Lymphoma
- Malignant fibrous histocytoma
Imaging features & discussion
Benign tumors
The radiological characteristics of these tumors are same as often seen in tumors of long bones [2-4]. It is often difficult to differentiate between giant cell tumor and aneurysmal bone cyst on conventional films. CT/MRI are needed to detect fluid-fluid levels that are often encountered in aneurysmal bone cysts.
Giant cell tumor
When the entire spine is taken into account, sacrum occupies a top place in having the giant cell tumor [5]. As noted in the long bones, it is subarticular in position and when aggressive may cross the sacroiliac joint and invade the ilium. On plain films a large, expansile, lytic area is noted (Figure 1a). The average age is between 25 and 40 years. CT identifies the large soft tissue mass associated with this tumor (Figure 1b-e). Giant cell tumor is in subchondral location and is often seen in upper segments. It may grow into the ilium crossing the sacroiliac joint [1]. A large osteolytic and expansile lesion with several septations is noted on conventional films. CT may show a thin sclerotic rim with a soft tissue mass. MRI shows intermediate signals in both T1 and T2 images.

Figure 1: (a) Giant cell tumor. (b, c) CT GCT (Note the large soft tissue component with central residual bone). (d) GCT in the upper segment of sacrum (Note the lytic area with sclerotic rim).
Aneurysmal bone cyst
Aneurysmal bone cyst (ABC) is an expansile lytic lesion with blood filled cystic spaces. It may be primary or secondary [2, 6]. However, secondary ABC’s are rare in sacrum. They resemble giant cell tumors on plain films. CT/MRI generally show fluid-fluid levels (Figure 2).
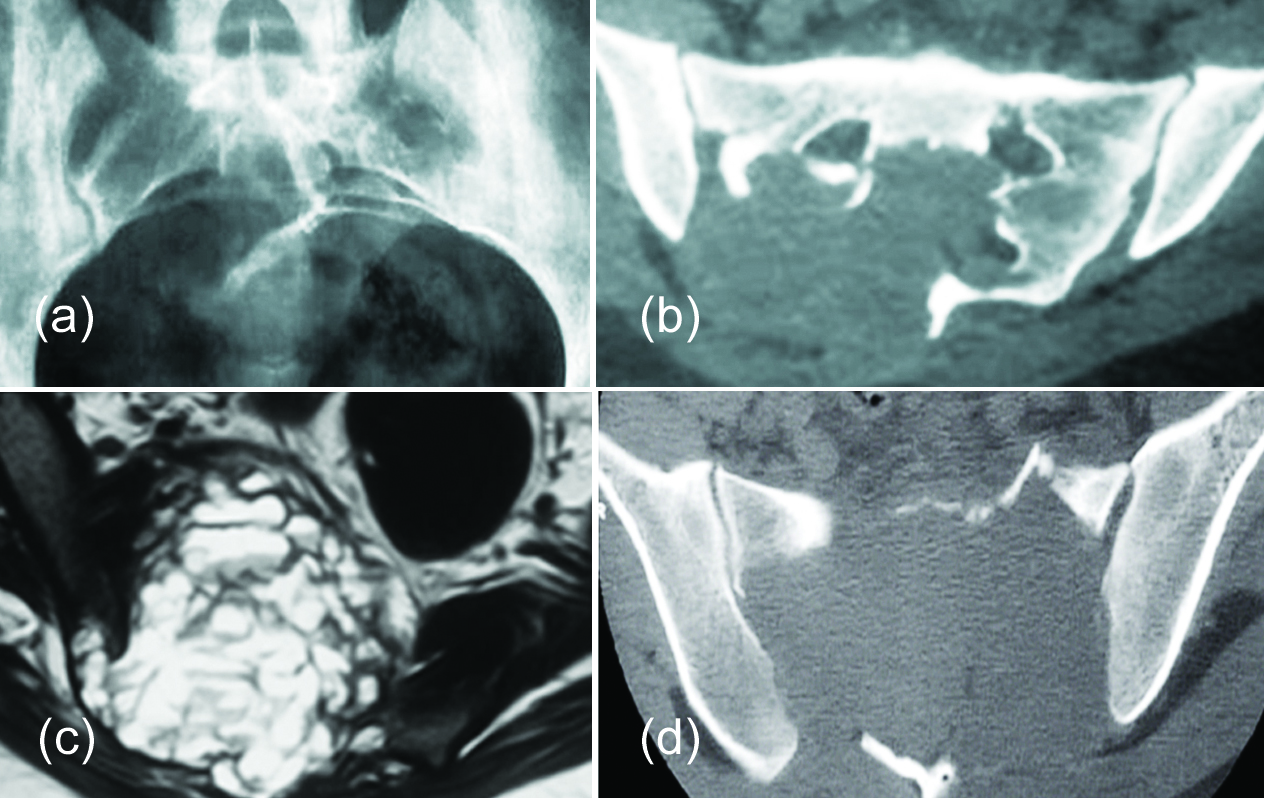
Figure 2: Aneurysmal bone cyst of 20-year-old female; (a) Plain film, (b) CT, (c) MRI showing fluid-fluid levels. (d) CT ABC (another patient).
Osteoid osteoma
Osteoid osteoma is a painful benign bone tumor encountered in young people. Conventional films often miss the diagnosis due to overlying intestinal contents. CT is the best modality to demonstrate the central calcified nidus with surrounded by reactive new bone (Figure 3). Radionuclide scan helps in locating the lesion [7]. Osteoid osteoma presents a typical picture of a calcified nidus surrounded by reactive new bone. CT or radionuclide scanning will depict the central calcified nidus [3].
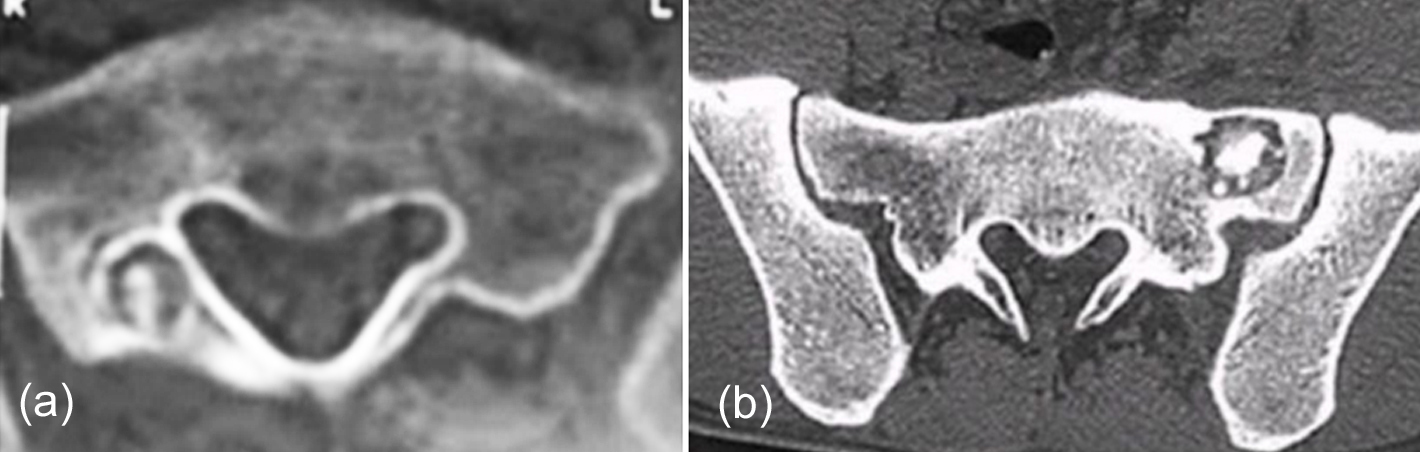
Figure 3a, b: CT Osteoid osteoma in two different patients showing the central nidus.
Osteoblastoma
Osteoblastoma is an unusual benign tumor occurring in the sacrum. The features are same as osteoid osteoma, except the nidus is more than 2cms in diameter and plain films often fail to demonstrate due to overlying intestinal contents. Occasionally, it may resemble aneurysmal bone cyst with large lucent nidus [4]. CT is the best modality to demonstrate the lytic lesion with the calcified nidus [8] (Figure 4).

Figure 4a, b: CT Osteoblastoma with mineralized nidus.
Osteochondroma
Benign cartilaginous tumors such as enchondroma of the sacrum are extremely rare. However, osteochondroma is one of the lesions seen occasionally. It may be sessile or pedunculated. Sessile lesions are often missed, whereas pedunculated lesions are noted even on plain films. CT helps in determining whether it is benign or malignant. The calcifications and the continuity of the cortical margin are characteristic features (Figure 5) of pedunculated osteochondroma.

Figure 5a, b: CT Osteochondroma of the sacrum.
Hemangioma
Hemangioma of the sacrum is extremely rare, although it is a common benign lesion in the rest of the vertebral column. Radiologically, spicules and honey combing is noted surrounded by thin sclerotic rim.
Sacro coccygeal teratomas
Sacro coccygeal teratomas (SCT) are common in infancy. These are composed of a mixture of solid and fluid components. SCTs are more often benign although malignant lesions may be encountered. Radiologically, a large soft tissue mass is seen with partial destruction of the sacrum. A cystic mass with small calcifications may be present particularly in infants (Figure 6). Rarely, it may be encountered in adults and some of them may be malignant as confirmed by histology.

Figure 6a, b: Sacrococcygeal teratoma (Note the large soft tissue mass).
Primary malignant tumors
Chordoma
Chordoma is the most common primary malignant tumor arising from the sacrum. Often it develops in the sacrococcygeal region. The average age ranges between 4th and 7th decades of life [5, 7, 8]. On plain films, it manifests as a large lytic lesion with or without internal calcifications (Figure 7a). Chondroid type of chordoma invariably shows typical cartilaginous classifications, nodular, arc like and ring type. A large soft tissue mass is usually present and may extend to the sacral canal, clearly noted on CT films (Figure 7b,c). On MRI low to intermediate signal intensity is noted on T1, and increased signal intensity on T2. Soft tissue component may or may not show enhancement (Figure 7d,e).
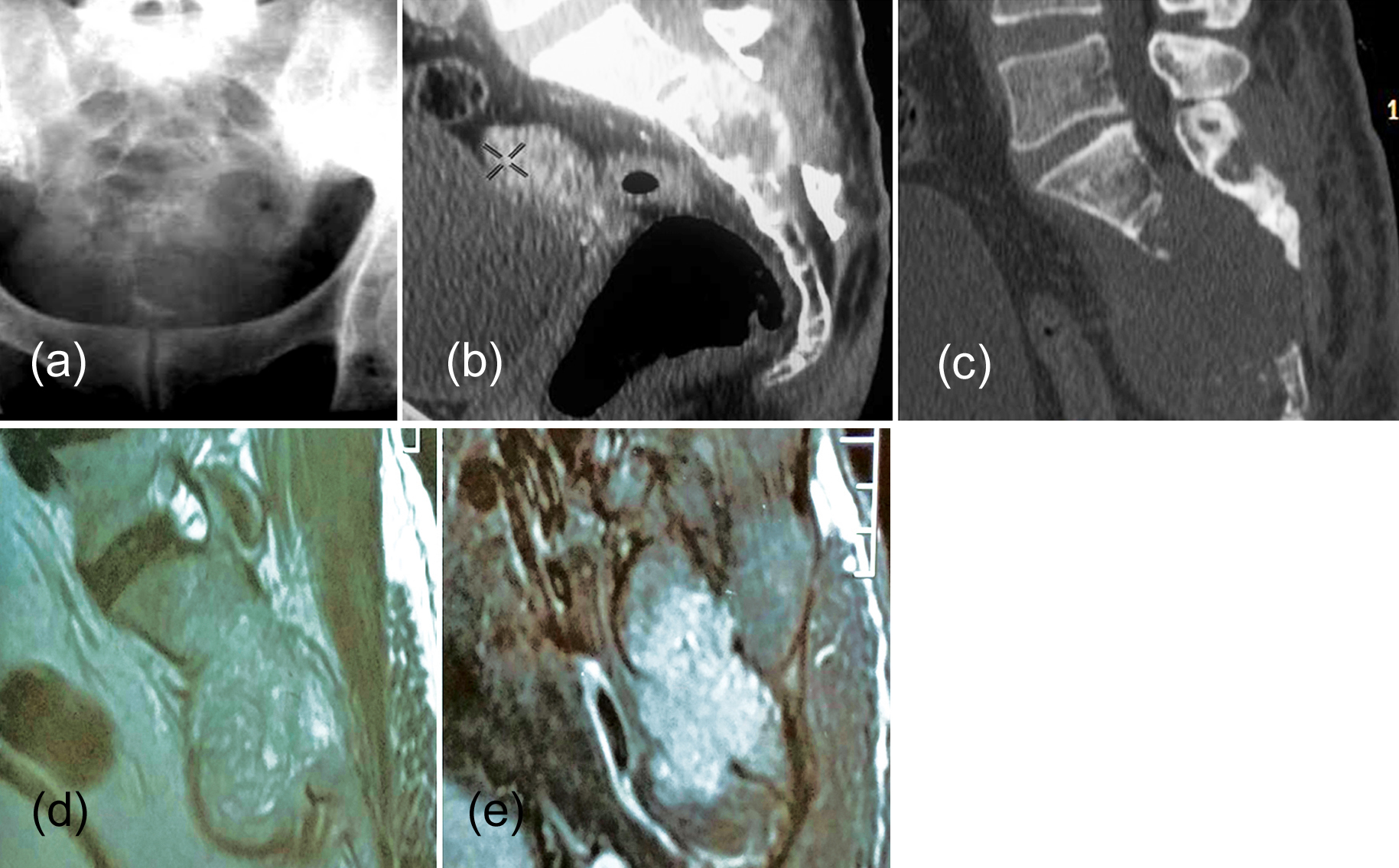
Figure 7: Chordoma; (a) plain film, (b, c) lytic lesion with large soft tissue mass. (d, e) MRI chordoma - (d) T1, (e) T2.
Chondrosarcoma
Chondrosarcoma is a rare lesion in the sacrum. Radilogically, it may simulate chondroid type of chordoma. On conventional films, a lytic lesion is noted with nodular, arc like and circular calcifications with a large soft tissue mass. CT is ideal to demonstrate these findings (Figure 8). MRI may show extension of the tumor into the soft tissues with a large soft tissue mass.

Figure 8: Chondrosarcoma CT; (a) AP, (b) lateral.
Ewing sarcoma
Ewing sarcoma is usually encountered in the 1st and 2nd decades of life. In the vertebral column, sacrum particularly, ala of the sacrum is a common site for the Ewing sarcoma. On conventional radiographs permeative osteolysis and areas of sclerosis are noted. No periosteal reaction is noted in the sacrum. Complete sclerosis like ivory vertebrae is not seen in sacrum. CT demonstrates osteolytic lesion with sclerosis and soft tissue swelling (Figure 9a). Soft tissue extension and involvement of the spinal canal are best observed on MRI (Figure 9b).
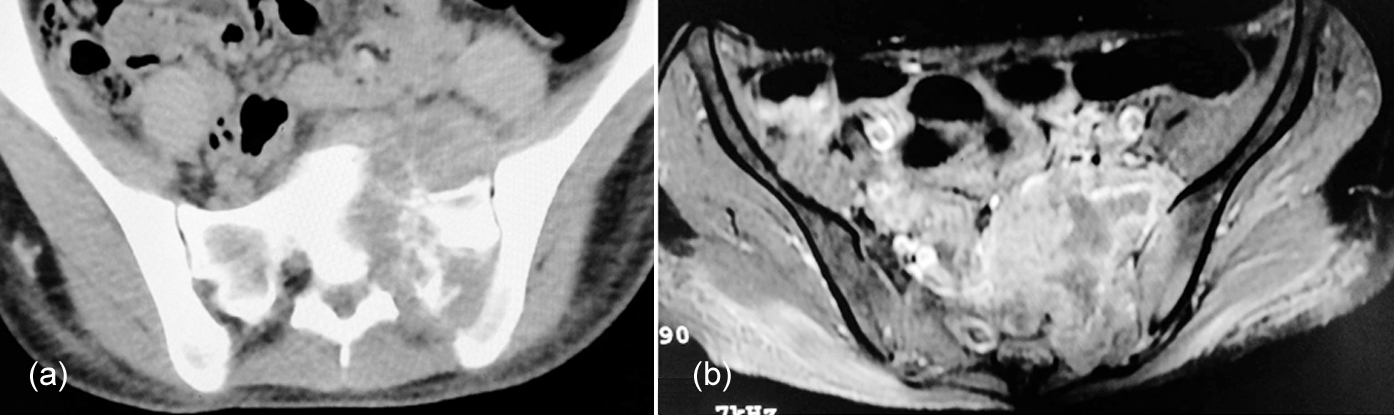
Figure 9: Ewing sarcoma; (a) CT, (b) MRI.
Primary osteosarcoma of the sacrum
Primary osteosarcoma of the sacrum is rare. A common radiological manifestation is a sclerotic lesion with osteoid mineralisation. Conventional radiology demonstrates diffuse, dense, sclerotic areas with lytic lesions (Figure 10a,b). CT demonstrates cloud-like osteoid and the extension into the adjacent bones. MRI may show soft tissue extension (Figure 10c,d). In children sacrum may be involved in osteosarcomatosis along with other bones. Secondary osteosarcoma may be seen after radiation therapy. It is also seen secondary to malignant transformation of Paget disease in adults.
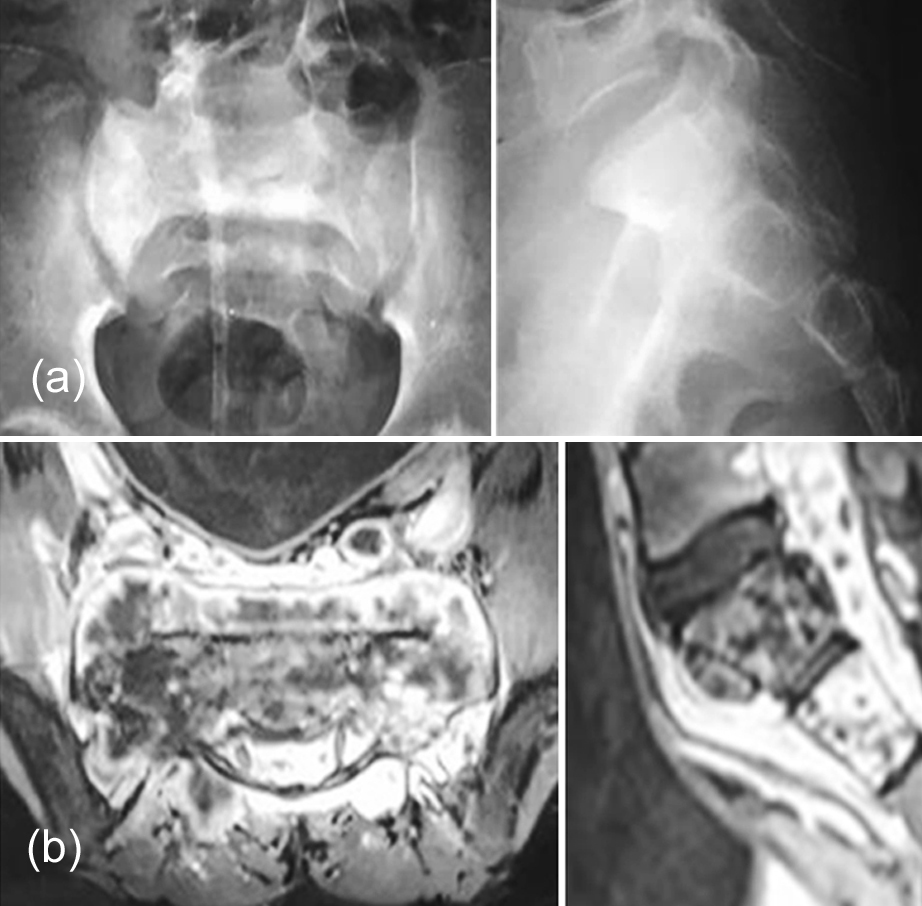
Figure 10a, b: Osteosarcoma, (a) AP, (b) lateral.
Plasmacytoma/ multiple myeloma
Plasmacytoma/ multiple myeloma is the most common tumor among older people. Plasmacytoma is the localised form of myeloma and sacrum is not an exceptional site. Radiologically a large, expanding lytic lesion is noted with thin transitional zone. The borders may be sclerotic. CT demonstrates the large lytic area and associated soft tissue swelling if any (Figure 11a, b). It may be small and localised (Figure 11c).
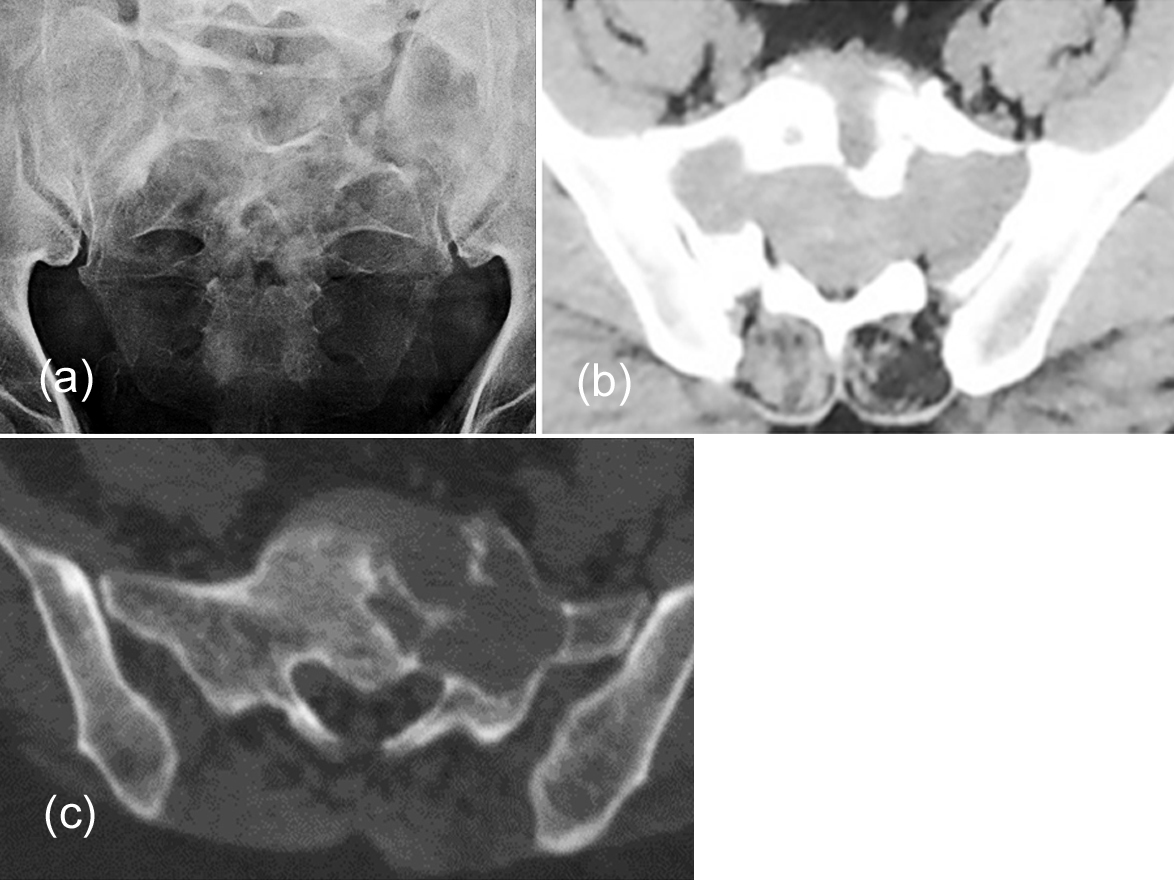
Figure 11: Large plasmacytoma; (a) plain film, (b) CT, (c) CT of another patient, small plasmacytoma.
Primary lymphoma of sacrum
Primary lymphoma of sacrum is quite rare. Sacrum may be involved in systemic Hodgkins and Non-Hodgkins lymphomas (Figure 12).
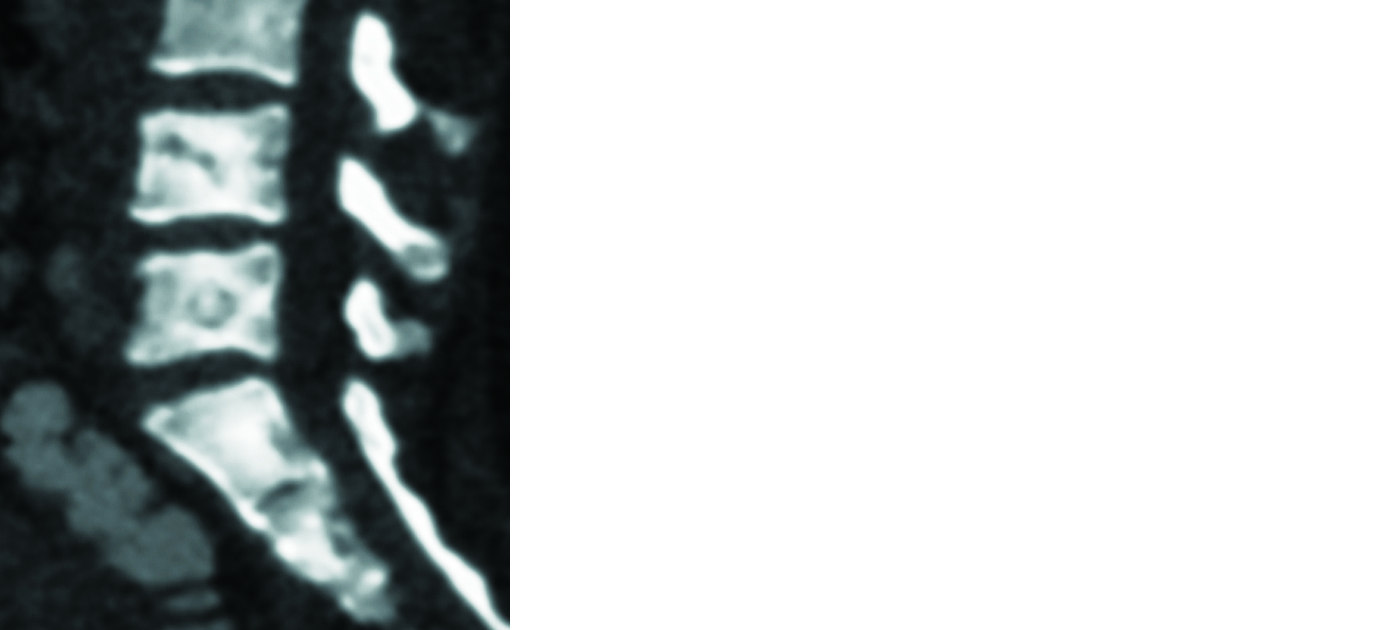
Figure 12: CT Non-Hodgkins lymphoma involving lumbar spine and sacrum.
Malignant fibrous histiocytoma of sacrum
Malignant fibrous histiocytoma of sacrum is quite rare. Radiologically, a large lytic area may be noted on the conventional film (Figure 13). It may simulate plasmacytoma or metastasis. CT and MRI may help in outlining the associated soft tissue swelling. Final diagnosis is made by histology only.

Figure 13: Malignant fibrous histiocytoma.
Differential diagnosis of primary malignant tumours of sacrum
In the differential diagnosis, both lytic and sclerotic metastasis are to be considered (Figure 14a,b). In a Bizzare trabecular pattern with sclerosis, fibrous dysplasia and Paget disease have to be considered (Figure 14c,d). A lytic area with soft tissue mass, neurogenic tumors have to be considered (Figure 15). Tuberculosis, pyogenic osteomyelitis and Langerhans Cell Histiocytosis may resemble primary sacral tumors. However, clinical, laboratory and histological findings have to be correlated. Brown tumours confined to sacrum are rare.

Figure 14a, b: (a) Metastasis from carcinoma thyroid; (b) Sclerotic metastasis from carcinoma of prostate.

Figure 14c, d: CT; (c) Paget disease, (d) Fibrous dysplasia.

Figure 15a, b: Myxopapillary appendymoma MRI.

Figure 15c, d: Schwannoma; (c) CT, (d) MRI.
Conclusion
Primary tumors of the sacrum are less frequent as opposed to the tumors arising from long tubular bones. Sacrum is obscured by overlying intestinal contents and hence conventional radiology is less effective in the diagnosis. In benign and malignant tumors CT and MRI will certainly help in defining the structure of the tumor and to arrive at a proper diagnosis. The imaging features are well illustrated. In most of the malignant tumors histopathology is absolutely necessary for final diagnosis.
Acknowledgements
KRUST museum, NIMS, KIMS-Secunderabad, India.
Conflicts of interest
Author declares no conflicts of interest.
References
[1] Unni KK, Inwards CY. Dahlin’s Bone Tumors. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.
[2] Llauger J, Palmer J, Amores S, Bagué S, Camins A. Primary tumors of the sacrum: diagnostic imaging. AJR Am J Roentgenol. 2000; 174(2):417–424.
[3] Ong KO, Ritchie DA. Pictorial essay: tumours and pseudotumours of sacrum. Can Assoc Radiol J. 2014; 65(2):113–120.
[4] Diel J, Ortiz O, Losada RA, Price DB, Hayt MW, et al. The sacrum: pathologic spectrum, multimodality imaging, and subspecialty approach. Radiographics. 2001; 21(1):83–104.
[5] Kwon JW, Chung HW, Cho EY, Hong SH, Choi SH, et al. MRI findings of giant cell tumors of the spine. AJR Am J Roentgenol. 2007;189(1):246–250.
[6] Gerber S, Ollivier L, Leclère J, Vanel D, Missenard G, et al. Imaging of sacral tumors. Skeletal Radiol. 2008; 37(4):277–289.
[7] Biagini R, Orsini U, Demitri S, Bibiloni J, Ruggieri P, et al. Osteoid osteoma and osteoblastoma of the sacrum. Orthopedics. 2001; 24(11):1061–1064.
[8] Shaikh MI, Saifuddin A, Pringle J, Natali C, Sherazi Z. Spinal osteoblastoma: CT and MR imaging with pathological correlation. Skeletal Radiol. 1999; 28(1):33–40.