Full Text
Introduction
There is a new public health crisis, coronavirus disease 2019 (COVID-19) pandemic, threatening the world with the emergence and spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Till date, there are very limited treatment options and no vaccines available for this infection. Therefore, infection prevention and control practice is the utmost important practice to combat this health crisis. Several properties of this virus make prevention difficult such as non-specific features of the disease, the infectivity even before onset of symptoms (incubation period) and transmission even after clinical recovery, transmission from asymptomatic people, tropism for mucosal surfaces such as the conjunctiva and prolonged duration of the illness.
In healthcare settings, the most common pathway of human-to human transmission has been the contact of the mucosae with infectious respiratory droplets or fomites [1]. Some research has shown that SARS-CoV can survive in sputum, serum, and faeces for at least 96 hours and in urine for 72 hours [2], and it can survive on surfaces up to 9 days [3]. Thus, it is essential to practice precautionary measures to limit the transmission of COVID-19 in health care facilities.
Various COVID-19 IPC guidelines have been adopted throughout the world. Therefore, a critical review of the available literature related to the COVID-19 outbreak is essential as part of informing and updating IPC guidelines. In this study, we explained the current recommendations for infection prevention and control (IPC) that should be followed by heath care professionals, when they are caring patients with suspected or confirmed SARS-CoV-2 infection.
Methods
We reviewed global COVID-19 IPC guidelines from the World Health Organization (WHO) and the US Centres for Disease Control and Prevention (CDC). We selected these international guidelines because they are commonly used as reference globally [4, 5]. We also reviewed national guidelines on COVID-19 prepared by Ministry of Health and Family Welfare, Govt of India, and guidelines provided by Indian Council of Medical Research (ICMR), New Delhi- National Institute of Virology, Pune and various Indian review literatures [6, 7].
Principle strategies of infection prevention and control (IPC) associated with COVID-19
The recommended Infection prevention and control (IPC) strategies may need to be sufficiently broad to control these transmission modes. The basic IPC strategies [8] include screening and triage of patients, standard precautions for all patients, implementing additional precautions, administrative controls and environmental & engineering controls (Table 1).
Table 1: Principle strategies of infection prevention and control (IPC) associated with COVID-19.
|
Screening and triage
|
Standard precautions
|
Additional precautions
|
Administrative controls
|
Environmental and engineering controls
|
|
Screening area
|
Hand hygiene
|
Isolation and cohorting of COVID-19 suspected or confirmed patients
|
Administrative measures related to healthcare workers.
|
Ventilation
|
|
Triage area
|
Respiratory hygiene
|
Contact and droplet precautions
|
Administrative measures to manage visitors
|
Ultraviolet germicidal irradiation (UVGI)
|
|
Designated waiting area
|
Use of PPE
|
Airborne precautions
|
|
Spatial separation and physical barriers
|
|
Inpatient area
|
Environmental cleaning
|
|
|
Environmental cleaning and disinfection
|
|
|
Biomedical Waste management
|
|
|
|
1. Screening and triage
Screening and triage of patients is essential to screen everyone at the entry point of the health-care facility (first point of contact) as well as inpatients with suspected COVID-19 for early recognition followed by immediate isolation [9].
In the screening area, health-care facilities should establish well-equipped display information at the entrance, directing patients to report to the designated area for screening. All patients must wear masks [10].
The staffs must be alert, well-trained regarding signs & symptoms and the latest case definitions of COVID-19. Screening personnel must wear personal protective equipment (PPE), based on WHO’s rational use of PPE guidance [10] (including mask and eye protection) and maintain a distance of at least 1 metre from patients, ideally with a separation created by a glass/plastic screen. Screening algorithm to be followed with the help of screening questionnaires to identify COVID-19 suspect patients promptly and direct them to an isolation room or dedicated COVID-19 waiting area.
In the Triage, all patients must be triaged using standardized and validated triage tool according to WHO Interim guidance [11] and clinical management protocol: COVID-19 (Govt of India, Ministry of Health and Family Welfare) [12]. Suspected COVID-19 patients with symptoms of respiratory distress and severe underlying conditions must be prioritized for medical evaluation.
Designated waiting area should have a designated, well-ventilated area with chairs placed at least 1 metre apart where patients with suspected COVID-19 can wait. There must be a dedicated toilet, hand hygiene station and closed bins for disposal of paper tissues used for respiratory hygiene. There should be a display board for patients to show them how to perform hand hygiene and respiratory etiquette [12].
Inpatient area
There are number of patients, who are presenting with extrapulmonary and atypical presentations, such as haemoptysis, cardiac, neurological, gastrointestinal, ocular and cutaneous manifestations, as well as venous and arterial thrombosis. Those may lead to misdiagnosis, delayed diagnosis and isolation of suspected COVID-19 [13]. Hence it is necessary to identify such inpatients missed by screening promptly by rapid testing to prevent the risk of transmission of infection between patients and doctors.
2. Standard precautions for all patients
They represent the basic level of infection control precautions that should be used at all times in the care of all patients.
Hand hygiene
Hand hygiene is one the most effective measures to prevent the spread of COVID-19. It includes either cleansing hands with an alcohol-based hand rub (ABHR) containing at least 70% alcohol when hands are not visibly dirty or with soap, water and disposable towels when hands are visibly soiled and dirty [14]. Hand hygiene practice must be optimized by performing appropriate steps, technique and duration of hand washing or hand rubbing [15]. Healthcare workers must follow “My 5 Moments for Hand Hygiene” approach by WHO [15]. One more key moment should be followed during COVID -19 scenario - after touching the face mask while using it.
Respiratory hygiene
Hand hygiene must be practiced after contact with respiratory secretions or objects that may be potentially contaminated with respiratory secretions. All patients must wear a mask.
Educational awareness through display of posters or graphic presentation should be encouraged in a view to aware everyone about the need to cover nose and mouth with a tissue or bent elbow while coughing or sneezing.
Use of personal protective equipment
The rational and appropriate use of personal protective equipment (PPE) reduces exposure to pathogens. PPE should be used based on the risk assessment. It may vary according to the setting and type of personnel and activity. The effectiveness of PPE strongly depends on: staff training on donning and doffing of PPE [16, 17], prompt access to sufficient supplies, appropriate hand hygiene, healthcare worker compliance and regular monitoring & feedback by IPC personnel.
NIOSH-approved N95 filtering facepiece respirator or higher (use a facemask if a respirator is not available) is recommended by CDC [16].
Don’ts about mask: (1) Do not touch/ hold front/ back part of mask (Figure 1), (2) Do not allow hanging of mask around neck, (3) Do not keep using mask for longer time/ days, (4) Do not wash mask and reuse and (5) Do not throw the mask here and there, should be disposed properly in yellow biomedical waste bin.

Figure 1: Touching the mask.
Overuse/ misuse of PPE will have a further impact on supply and availability of PPE (Shortage). The optimal availability of personal protective equipment (PPE) can be achieved by minimizing the need for PPE through- restriction of visitors to the COVID-19 ward, restriction of HCWs from entering the COVID-19 ward if they are not involved in direct care and considering bundle activities to minimize the number of times a room is entered (e.g., check vital signs during medication administration or have food delivered by HCWs while they are performing other care).
To combat the short supply of N95 mask, Centres for Disease Control and Prevention (CDC) recommended extended use of N95 mask, Limited reuse of N95 mask and reprocessing of N95 mask followed by reuse [18-20].
Environmental cleaning
Cleaning and disinfecting environmental surfaces are fundamental in reducing the infectious pathogen. It is important to practice the cleaning and disinfection procedure consistently and correctly. All surfaces in health-care facilities including floors, walls, high-touch surfaces, visibly soiled area or area contaminated by body fluid and ambulances should be routinely cleaned and disinfected using the products containing antimicrobial agents known to be effective against coronavirus. The areas, where suspected or confirmed COVID-19 patients are admitted (COVID ICU and Isolation ward) should be cleaned and disinfected more frequently depending on the nature of the surface and the degree of contamination.
The following disinfectants/chemicals are recommended for disinfection of various surfaces and areas [21-23]. Hands by hand sanitizer containing at least 70- 80% alcohol, surface disinfection such as floors & ambulances by Sodium hypochlorite at 0.1% (equivalent 1000 ppm) to 0.5% (equivalent 5000 ppm), Equipment like BP apparatus, stethoscope, thermometers, plastic folders and frequent contact surfaces like TV buttons can be disinfected by 70% - 90% ethanol (alcohol swab). Recommended contact time should be strictly followed [22].
For effective environmental cleaning
Housekeeping services play a major role: Well-trained housekeeping staffs for cleaning environmental surfaces must designate. They must be trained on proper use of PPE (including boots and heavy-duty gloves) and hand hygiene. They must wash their hands with soap and water immediately after removing the PPE and when cleaning and disinfection work is completed [14, 17]. A checklist should be maintained for accountability. In case of any adverse incident, housekeeping staffs must report to supervisor immediately.
Following measures should be followed during surface wiping: Surface wiping should be done from clean to unclean area and top to down. Zig-zag pattern of cleaning and re-dipping of cloth is not recommended [23].
Measures during mopping should be appropriate: Separate buckets and mops, disinfectants should be kept separately in an identified (clean) area in the ward. Gross soil should be removed prior to cleaning and disinfection. Brooms should not be used. Damp dusting and wet mopping is recommended to minimize dust. Mop should be washed under running water before doing wet mopping and it must be changed more frequently in heavily contaminated areas. Cleaning of the surfaces must be thorough with clean water and detergent. Use of 3-bucket system is preferable. A figure of eight stroke technique for mopping is recommended in open and wide spaces, overlapping each stroke with turning of mop head over every five or six strokes [23] (Figure 2).
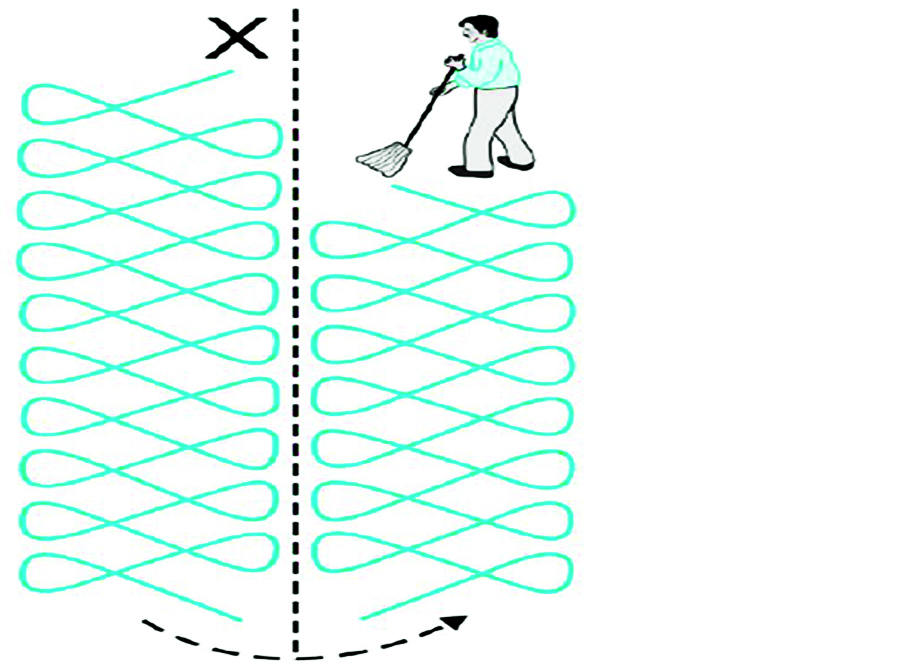
Figure 2: Eight stroke technique for mopping.
Cleaning should always be done from cleanest area to dirtiest area, such as higher area to lower area, outer side to inner side. Isolation areas should be cleaned last.
After cleaning, all equipment used for cleaning should be washed with soap and hot water followed by decontamination with 0.5% hypochlorite and then should be dried in sunlight [21].
Disinfection protocol of medical devices & equipment, ambulances and lifts should be formulated by Infection Control Committee of the institution. Standard Operative Procedures (SOP) should be there for infection control practice in laundry. Food services and utensils should be managed in accordance with safe routine procedures [21].
Biomedical waste management
Biomedical waste management should be followed stringently as health-care waste produced during the care of patients with suspected or confirmed COVID-19 is considered to be the most infectious. Therefore, these should be collected safely in clearly marked containers and sharp safe boxes following BMW management rules, 2016 and latest guidelines provided by Central Pollution Control Board [24]. Health-care facility should provide adequate human and material resources to segregate and disposal of waste. Appropriate PPE must be used while managing infectious waste and hand hygiene must be performed after donning off the PPE [10, 15, 16].
All laboratory waste from testing suspected or confirmed COVID-19 patient specimens should be regarded as potentially infectious. They should be segregated and discarded as all other biohazardous waste in the laboratory following standard guideline. Currently, there is no evidence to suggest that this laboratory waste needs any additional packaging or disinfection procedures [21].
3. Implementing additional precautions
Person-to-person transmission of SARS-CoV-2 virus (virus causing COVID-19) is primarily occurs via droplet and contact transmissions [25-27]. When the infected person coughs or sneezes, respiratory droplets (size >5µm) are produced, which can infect the other persons (by seeding on their mouths, noses or conjunctiva) who are in close contact (within one meter distance). Respiratory droplets may further settle down on floor, surfaces and inanimate objects (eg: door handles). Contact transmission occurs either by direct contact with infected people or by indirect contact with fomites [28] such as stethoscope or thermometer. Airborne transmission of the COVID-19 virus (respiratory droplets of size <5µm) is possible under certain circumstances such as during aerosol generating procedures (AGPs) [29].
Isolation and cohorting of COVID-19 suspected or confirmed patients
Suspected or confirmed patients must be isolated in single well-ventilated rooms [30]. In case of unavailability of the single room, cohorting of patients can be done. Specific cohorted area must be well ventilated with beds placed at least one metre apart.
A dedicated team of health care workers should be designated. Unnecessary entry of health care workers should be restricted by maintaining a record of all staff entering the cohorted area. Visitors must be restricted to those areas.
Patient’s movement out of the room should be restricted. Designated portable X-ray machine and other diagnostic equipment should be available. If transport of patient is required at all, patient should wear a surgical mask and predetermined dedicated transport route should be used. Healthcare worker must wear appropriate PPE [10]. Equipment should be either single use / disposable or dedicated equipment for each patient such as stethoscopes, blood pressure cuffs and thermometers. If equipment needs to be shared, it must be clean and disinfect with 70% ethyl alcohol [21].
Contact and droplet precautions
Healthcare workers, care givers and housekeeping staffs should follow contact and droplet precautions apart from standard precautions before entering the room, where suspected or confirmed COVID-19 patients are admitted. Hand hygiene [15] should be performed before donning and after doffing of PPE.
Healthcare workers should refrain from touching their eyes, nose or mouth with potentially contaminated gloved or bare hands. Appropriate PPE [10] must be used such as medical mask, eye protection (googles) or facial protection (face shield) to avoid contamination of mucous membranes.
Extended use of medical mask, gown and eye protection and reuse N95 mask can be applied during the care of COVID-19 patients during PPE shortage [18, 19].
Frequent cleaning and disinfection of surfaces (with which the patient is in contact) is needed [21].
Airborne precautions
Aerosol Generating Procedures (AGP) have been associated with an increased risk of transmission of SARS-CoV-2. The current WHO list of these AGPs include tracheal intubation, non-invasive ventilation (e.g., BiPAP, CPAP), tracheotomy, cardiopulmonary resuscitation, manual ventilation before intubation, bronchoscopy, sputum induction induced by using nebulized hypertonic saline, and autopsy procedures.
Healthcare workers performing AGPs among suspected or confirmed COVID-19 patients should use appropriate PPE, which should include particulate respirator at least as protective as a US National Institute for Occupational Safety and Health (NIOSH)-certified N95, European Union (EU) standard FFP2, or equivalent. Fit testing is needed prior to the use of a particulate respirator [16, 31].
Other PPE items include eye protection (i.e., goggles or a face shield), long-sleeved gown/ coverall and gloves. If gowns are not fluid resistant, waterproof apron can be the alternative option.
4. Implementing administrative controls
Administrative controls for the prevention and control of transmission of COVID-19 within the health-care facility include preventing overcrowding, especially in the emergency department: providing dedicated waiting areas for symptomatic patients: developing policies for early recognition of patients with suspected COVID-19: ensuring easy access to laboratory testing for COVID-19 detection: planning for isolating COVID-19 patients; ensuring adequate supplies of PPE: establishing sustainable IPC infrastructures & activities and ensuring adherence to IPC policies in all aspects of health care.
Administrative measures related to healthcare workers
This include providing adequate training for healthcare workers; monitoring of healthcare workers’ compliance with standard precautions and providing mechanisms for improvement (if needed); ensuring adequate patient-to-staff ratio; establishing an active syndromic surveillance of healthcare workers at the entrance when they arrive at work and ensuring that healthcare workers as well as the general public understand the importance of seeking medical care promptly.
Administrative measures to manage visitors
All health-care facilities should implement policies to restrict visitor access.
Health-care facilities should: introduce alternative measures for direct interaction between patients, family members and clinical staffs such as communications through telephone, internet connection, etc., encourage family members to assign a single caregiver to the patient, who are not at high risk for severe COVID-19; designate a separate entrance to access the health-care facility by the caregivers; maintain records of all visitors allowed in the health care facility; conduct active screening of all caregiver visitors before entering the healthcare facility; educate caregiver visitors on hand hygiene, respiratory etiquette, physical distancing, standard precautions and signs & symptoms of COVID-19; educate the caregivers of the patients about the droplet and contact precaution and the use of required PPE and relocate the outpatient pharmacy or other services to a location outside of the main health-care facility to reduce traffic to the health-care facility.
5. Implementing environmental and engineering controls
Environmental and engineering controls are an integral part of Infection Prevention and Control. It plays a key role in reducing the concentration of infectious respiratory aerosols (i.e. droplet nuclei) in the air and the contamination of surfaces and inanimate objects.
Ventilation
Ventilation is an integral part as SARS-CoV-2 virus spreads primarily via respiratory droplets, that may aerosolize under certain conditions. The three basic criteria for the ventilation are: (1) ventilation rate: the amount and quality of outdoor air provided into the space; (2) airflow direction: the overall airflow direction in a building as well as in the between area from clean-to-less clean zones and (3) airflow pattern: the supply of air that should be delivered to each area to improve dilution and removal of airborne pollutants generated in that area.
Ventilation of large amount of fresh and clean outdoor air is essential in health-care facilities. The method of ventilation further can be categorized as natural and mechanical ventilation. Each ventilation system has its advantages and disadvantages.
Naturally ventilated areas: Contaminated air exhaust directly outdoor, away from air-intake vents, clinical areas, and people. The application of natural ventilation depends on favourable climate conditions.
Mechanically ventilated areas: In health-care facilities where a mechanical ventilation system is available, negative pressure should be created to control the direction of airflow. Airflow direction can be assessed by measuring the pressure difference between clean to a less-clean area.
For health-care facilities without adequate natural or mechanical ventilation, the following approaches can be considered [32].
• Installation of exhaust fans: fans need to be installed so that the air is released directly outdoors
• Installation of high-efficiency particulate air (HEPA) filters: When appropriately selected, deployed and maintained, it can be effective in reducing concentrations of infectious aerosols in a single space [33, 34]. HEPA with a 99.97% efficiency for removing particles >0.3 µm in diameter must be used.
General guidance on how long it takes for aerosols to be removed by different ventilation conditions is suggested by CDC [35].
Ultraviolet germicidal irradiation (UVGI)
UVGI has been proposed as a supplemental air-cleaning measure. It is of limited use because of their potential adverse effects over outer surfaces of the eyes and skin, leading to keratoconjunctivitis and dermatosis.
Spatial separation and physical barriers
Spatial separation of at least 1 metre should be maintained between patients at all times. Both spatial separation and adequate ventilation can help to reduce the spread of many pathogens in the health-care facility [36]. Use of physical barriers such as glass or plastic windows can be implemented in the screening and triage areas, registration desk at the emergency department, or at the pharmacy window where medication is collected.
Environmental cleaning and disinfection
Environmental cleaning and disinfection is the most essential element among environmental controls. Cleaning and disinfection procedures must be performed consistently, appropriately and frequently. Cleaning environmental surfaces with water & detergent, and applying commonly used hospital disinfectants (such as sodium hypochlorite) is an effective procedure [21].
Collection and transport of laboratory specimens from patients with suspected COVID-19
All specimens collected for laboratory investigations should be regarded as potentially infectious.
Nasopharyngeal or oropharyngeal swabs should be collected from patients by trained healthcare worker following full infection control practices including use of appropriate PPE. If the specimen is collected with an AGP (e.g., sputum induction), healthcare worker conducting the procedure should wear a particulate respirator at least as protective as a NIOSH-certified N95, an EU standard FFP2, or equivalent [16]. All specimens should be safely packed (in Triple container packing) [37], labelled, marked, and documented as Category B, UN 3373 (Figure 3). All specimens should be delivered by hand whenever possible. Pneumatic-tube systems to transport specimens is not recommended at all. All personnel who transport specimens must be trained in safe handling practices and spill decontamination procedures. Specimen should be transported under cold chain to the reference laboratory with prior intimation. Laboratory request forms and ICMR information forms should be documented appropriately [38].
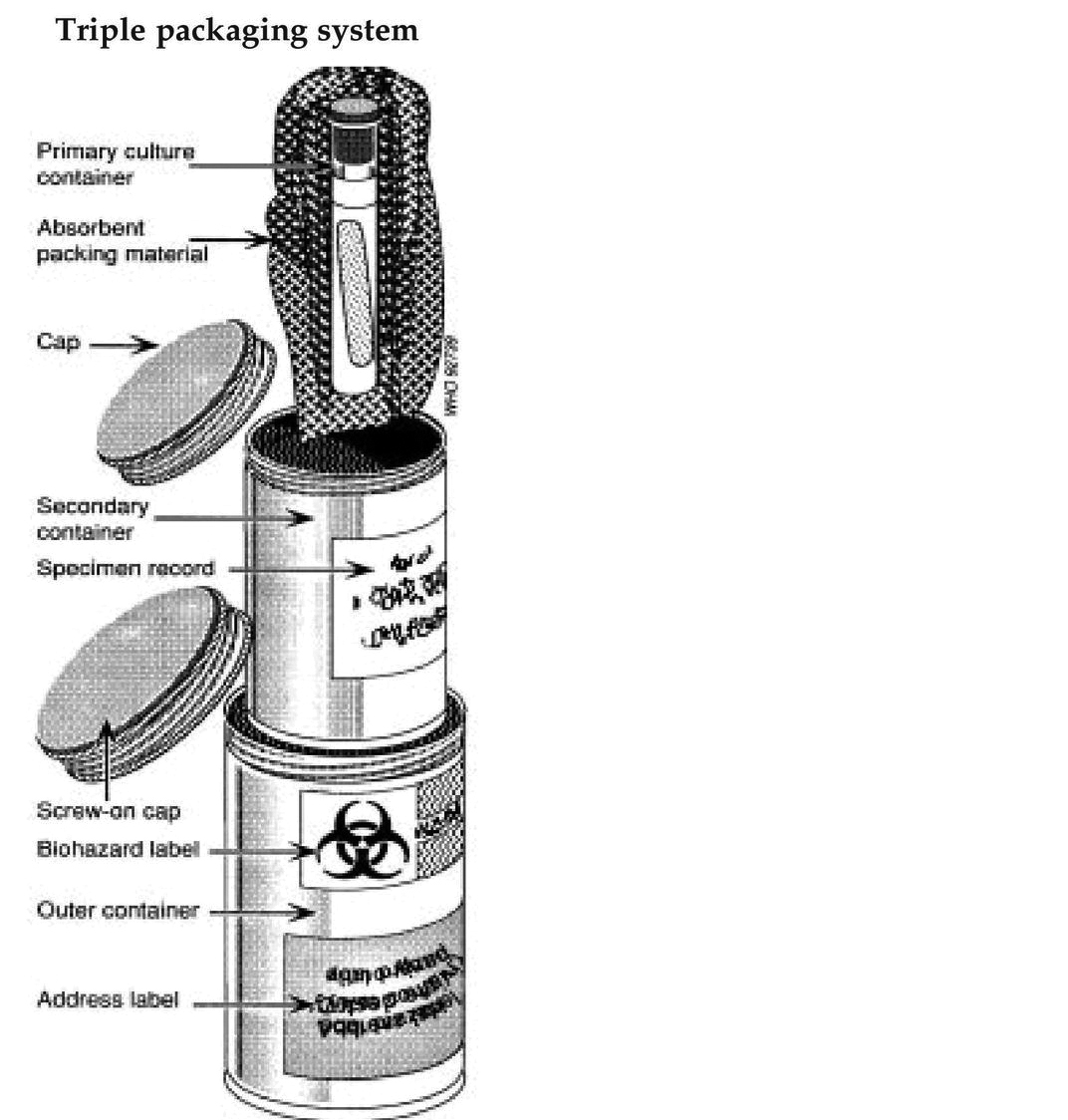
Figure 3: Triple packaging system.
Considerations for surgical procedures
In COVID-19 pandemic scenario, any decision on whether to operate on a patient should be based on need of surgery, the risks and benefits of surgery (e.g., life-threating outcomes or patient harm if surgery is delayed) and patient clinical conditions. During this pandemic, every surgical procedure may enhance the risk for both health workers and patients [39]. Hence as part of their routine clinical practice, healthcare workers should apply standard precautions and potential risks assessment. These precautions should include engineering controls, administrative controls, and use of proper PPE.
General considerations
Preference should be given to non-surgical interventions or alternative treatments. Elective surgery should be postponed. If surgical procedure cannot be postponed, a careful risk assessment should be done to screen patients for COVID-19 symptoms, signs and exposure history. Patients with sign and symptoms of COVID-19 should be tested for the virus using molecular assay on nasopharyngeal swab [40].
If the urgency of the surgical procedure does not allow sufficient time for molecular testing, rapid antigen detection assay for COVID-19 (Chromatographic immunoassay) can be in performed [41]. Patients with signs of COVID-19 should undergo chest-X-ray, chest computerized tomography (CT) or chest ultrasound, if available, as an early diagnostic tool and as a baseline to monitor patient [42]. Aerosol generating procedures should be avoided.
Surgical procedures in suspected or confirmed COVID-19 patients
During surgical procedures in COVID-19 patients, surgical staff in the operating room should use contact and droplet precautions. A particulate respirator (i.e., N95, FFP2 or equivalent) should be used, if there is potential for an anticipated or unanticipated AGP or if the procedure involves anatomic regions where viral loads of the virus may be higher such as nose, oropharynx and respiratory tract [43, 44].
Patients should wear a medical mask while being transported to the operating room. Transport staff should use contact and droplet precautions when transporting suspected or confirmed COVID-19 patients to the operating room.
A negative pressure room should be used for anaesthesia and intubation, if available. However, if a negative pressure room is not available, intubation should occur in the operating room where the surgical procedure will be performed [43].
One or more operating rooms for surgical procedures of COVID-19 patients could be identified in the far corner of the surgery floor. If it is not be dedicated to COVID-19 patients, can also be used for surgical procedures of other patients, after terminal cleaning. Surgical staff in the room should be limited to essential personnel. Operating rooms should be built with proper engineering control having a high ventilation rate (15-20 ACH) and their doors should always remain closed during procedures [45, 46]. Terminal cleaning must be performed after each surgical procedure [21].
All surgical instruments should undergo standard transport, cleaning and sterilization procedures. Medical masks, eye protection, gloves and gowns should be worn by personnel responsible for cleaning these instruments prior to sterilization.
Surgical procedures in patients whose COVID-19 status is unknown
Transport staff should wear a medical mask when transporting patients to the operating room. Contact and droplet precaution should be applied by surgical staff. In health-care facilities, who do not have COVID-19 test capacity or where testing could not be done due to the urgency of the procedure, a particulate respirator can be worn. Terminal cleaning of operating room should be performed using standard hospital cleaning.
Dead body management
Healthcare workers should do a preliminary evaluation and risk assessment before undertaking any activity related to the management of suspected or confirmed COVID-19 fatality.
COVID-19: Guidelines on dead body management (15.03.2020) formulated by Government of India Ministry of Health & Family Welfare Directorate General of Health Services (EMR Division) should be followed [47]. Operational guidelines for monitoring disposal/ confirmed cases of COVID-19 dead bodies provided by the state government also to be considered.
General recommendations: This include need of one robust leak-proof body bag and final treatment- either by cremation or burial depending up on the religious practice; however, cremation is more advisable. Autopsies on COVID-19 dead bodies should be avoided.
Standard infection and prevention control practices should be followed at all times which include:
Hand hygiene: Use of personal protective equipment; safe handling of sharps; disinfection of the bag housing dead body, instruments and devices used on the patient; disinfection of linen and disinfect ion of environmental surfaces.
Training in infection and prevention control practices: All staff identified to handle dead bodies in the isolation area, mortuary, ambulance and those workers in the crematorium/ burial ground should be trained in the infection prevention control practices.
Specific recommendations: These include the healthcare worker attending to the dead body should perform hand hygiene, proper use of PPE (water resistant apron, goggles, N95 mask, gloves, shoe cover) and appropriate steps of donning and doffing of PPE. Oral, nasal orifices of the dead body should be plugged to prevent leakage of body fluids. The dead body should be placed inside leak-proof plastic body bag and the exterior of the body bag to be decontaminated with 1% Sodium hypochlorite. All used/soiled linen should be handled with standard precautions, put in Yellow bio-hazard bag and the outer surface of the bag disinfected with 1% Sodium hypochlorite solution. Used equipment should be autoclaved or decontaminated with disinfectant solutions in accordance with established infection prevention control practices. Healthcare workers must be very cautious while handling sharps such as intravenous catheters and other sharp devices. All medical waste must be handled and disposed of in accordance with Bio- medical waste management rules. Environmental cleaning and disinfection procedures must be performed stringently. All surfaces of the isolation area (floors, bed, railings, side tables, IV stand, etc.) should be wiped with 1% Sodium hypochlorite solution, to allow a contact time of 30 minutes, and then allowed to air dry.
Recommendation for outpatient care
The basic principles of IPC and standard precautions should be applied in outpatient settings and primary care. The following measures can be adopted to prevent transmission of COVID-19.
Alternatives to face-to-face consultation- using telemedicine (e.g., telephone consultations or cell phone videoconference) can be provided for clinical support [48]. Prioritization can be done for care of symptomatic patients. Patients can sit at least 1-meter apart with masks in waiting area. The patients with suspected COVID-19 must be screened, recognized and isolated as early as possible.
The importance of hand hygiene and respiratory hygiene must be emphasized. Appropriate use of contact and droplet precautions must be taken while performing clinical exam on patients with suspected COVID-19. Education should be provided to patients and families about the early recognition of symptoms, basic precautions to be used and which health-care facility they should refer to if any family member shows signs of COVID-19.
As the number of COVID-19 patients is dramatically increasing worldwide and treatment has become a major challenge. Overcrowding in emergency rooms and contamination of the environment further contribute to viral spread. It has no definitive treatment and vaccination till date. The prevention of disease transmission is the most essential component at this scenario. Correct implementation of Infection Prevention and Control (lPC) measures will minimize the spread of the COVID-19 virus in health-care facilities. It should be performed continuously, consistently and correctly.
Conclusion
The increasing numbers of COVID-19 cases among healthcare professionals along with evidence of ongoing transmission in some healthcare settings suggest that some gaps must be there in IPC practices. Hence all of the guidelines should be revisited and implemented properly. A set of process, output and outcome key performance indicators (KPIs) are recommended to monitor and evaluate implementation of IPC measures. Several tools have been developed for health-care facilities and public health services such as (1) CDC facility readiness assessment for COVID-19 and (2) CDC checklist and monitoring tool for triage of suspected COVID-19 cases. All health-care facilities should use these tools for IPC assessment to identify IPC gaps and to monitor progress. WHO surveillance protocol for data collection among health workers infected with the COVID-19 virus and a case-control study to assess risk factors for COVID-19 among health workers are also available. Information, education and communication (IEC) messages should encourage self-deferral and self-containment for patients who are symptomatic. Simultaneously, appropriate implementation of Infection Prevention and Control (IPC) strategies should reduce the spread of infection. The combined effect of these two will definitely reduce COVID-19 disease transmission.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Seto WH, Tsang D, Yung RWH, Ching TY, Ng TK, et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet. 2003; 361(9368):1519–1520.
[2] Duan SM, Zhao XS, Wen RF, Huang JJ, Pi GH, et al. Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation. Biomed Environ Sci. 2003; 16(3):246–255.
[3] Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020; 104(3):246–251.
[4] World Health Organization. Guidelines on Core Components of Infection Prevention and Control Programmes at the National and Acute Health Care Facility Level. Geneva: WHO; 2016. Available from: https://www.who.int/gpsc/ipc-components/en/
[5] Centres for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Patients with Confirmed 2019 Novel Coronavirus (2019-nCoV) or Persons Under Investigation for 2019-nCoV in Healthcare Settings, in 2019 Novel Coronavirus. Altanta: CDC; 2020.
[6] Sharma SK, Mudgal SK, Panda PK, Gupta P, Aggarwal P. COVID–19: Guidance Outlines on Infection Prevention and Control for Health Care Workers. Indian J Commun Health. 2020; 32(1):8–14.
[7] Islam MS, Rahman KM, Sun Y, Qureshi MO, Abdi I, et al. Current knowledge of COVID-19 and infection prevention and control strategies in healthcare settings: A global analysis. Infect Control Hosp Epidemiol. 2020; 41(10):1196–1206.
[8] World Health Organization. Infection prevention and control during health care when coronavirus disease (COVID-19) is suspected or confirmed. Interim guidance. 29 June 2020. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-2020.4
[9] World Health Organization. Screening: refers to prompt identification of patients with signs and symptoms of COVID-19. Clinical management of COVID-19. Interim guidance. 27 May 2020. Available from: https://www.who.int/publications/i/item/clinical-management-of-covid-19
[10] World Health Organization. Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19). Geneva; 2020. Available from: https://apps.who.int/iris/handle/10665/331215
[11] World Health Organization. Triage: prioritization of care according to severity using validated tools (e.g., WHO/ICRC/MSF/IFRC Integrated Interagency Triage Tool). Clinical management of COVID-19 Interim guidance. 27 May 2020. Available from: https://apps.who.int/iris/rest/bitstreams/1284718/retrieve
[12] Clinical management protocol: COVID-19 (Govt of India, Ministry of Health and Family Welfare). Available from: https://www.mohfw.gov.in/pdf/UpdatedClinicalManagementProtocolforCOVID19dated03072020.pdf
[13] Abobaker A, Raba AA, Alzwi A. Extrapulmonary and atypical clinical presentations of COVID-19. J Med Virol. 2020; 92:2458–2464. [14] World Health Organization. WHO guidelines on hand hygiene in health care: first global patient safety challenge – clean care is safer care. Geneva, 2009. Available from: https://apps.who.int/iris/bitstream/handle/10665/44102/9789241597906_eng.pdf?sequence=1
[15] Hand Hygiene: Why, How & When? Geneva: World Health Organization; 2009.
[16] Using Personal Protective Equipment (PPE) by CDC. Available from: https://www.cdc.gov/coronavirus/2019-ncov/downloads/A_FS_HCP_COVID19_PPE.pdf
[17] World Health Organization. How to put on and take off personal protective equipment (PPE). Geneva, 2020. Available from: https://apps.who.int/iris/handle/10665/70066
[18] Recommended Guidance for Extended Use and Limited Reuse of N95 Filtering Facepiece Respirators in Healthcare Settings. CDC. Available from: https://www.cdc.gov/niosh/topics/hcwcontrols/recommendedguidanceextuse.html
[19] Implementing Filtering Facepiece Respirator (FFR) Reuse, Including Reuse after Decontamination, When There Are Known Shortages of N95 Respirators. Updated Aug. 4, 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care.html.
[20] Kobayashi LM, Marins BR, Costa PCDS, Perazzo H, Castro R. Extended use or reuse of N95 respirators during COVID-19 pandemic: An overview of national regulatory authority recommendations. Infect Control Hosp Epidemiol. 2020; 1–3.
[21] Environmental cleaning, disinfection and bio-medical waste management- guidelines on COVID-19 prepared by Ministry of Health and Family Welfare, Govt of India.
[22] COVID-19 Preparedness Document AIIMS, New Delhi Version 1.0, 27th March, 2020
[23] Infection Prevention and Control (IPC) SOP for COVID-19, JIPMER, Version-2, 9th April, 2020.
[24] Central Pollution Control Bord (Ministry of Environment, Forest & Climate change). Guidelines for handling, treatment and disposal of waste generated during treatment/diagnosis/ quarantine of COVID-19 patients. Available from: http://www.bspcb.bih.nic.in/Rev.4%20COVID%20Guidelines%20CPCB.pdf
[25] Liu J, Liao X, Qian S et al. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerg Infect Dis. 2020; 26(6):1320–1323.
[26] World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) 16-24 February 2020, Geneva, Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
[27] Ong SW, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020; 323(16):1610–1612.
[28] Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012; 7(4):e35797.
[29] Atkinson J, Chartier Y, Pessoa-Silva CK, Jensen P, Li Y, Seto WH, editors. Natural ventilation for infection control in health care settings. Geneva: World Health Organization; 2009. Available from: https://apps.who.int/iris/handle/10665/44167
[30] How to perform a particulate respirator seal check. Geneva: World Health Organization; 2008. Available from: http://www.who.int/csr/resources/publications/respiratorsealcheck/en/
[31] Guidelines for Environmental Control in Health care Facilities. Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC), 2003; updated July 2019. Available from: https://www.cdc.gov/infectioncontrol/pdf/guidelines/environmental-guidelines-P.pdf,
[32] Shaughnessy RJ, Levetin E, Blocker J, Sublette KL. Effectiveness of Portable Indoor Air Cleaners: Sensory Testing Results. Indoor Air 1994: 4(3):179–188.
[33] Wen Z, et al. Assessment of the risk of infectious aerosols leaking to the environment from BSL-3 laboratory HEPA air filtration systems using model bacterial aerosols. Particuology. 2014; 13:82–87.
[34] Guidelines for Environmental Infection Control in Health-Care Facilities (2003), Airborne Contaminant Removal, Table. B1 Available from: https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html#tableb1.
[35] Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, et al. COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020; 395(10242):1973–1987.
[36] Specimen Collection, Packaging and Transport Guidelines for 2019 novel Coronavirus (2019-nCoV). ICMR-NIV/2019-nCoV/Specimens_01. 20/01/2020, Available from: https://www.mohfw.gov.in/pdf/5Sample%20collection_packaging%20%202019-nCoV.pdf
[37] ICMR Specimen Referral Form for COVID-19 (SARS-CoV2). tmc.cov.in> Sample requisition Form (SRF)- ICMR. Available from: https://tmc.gov.in/pdf/covid-19%20test/Sample%20Requisition%20Form%20(SRF)-%20ICMR.pdf
[38] World Health Organization. Global surveillance for COVID-19 caused by human infection with COVID-19 virus: interim guidance. Geneva, 2020. Available from: https://apps.who.int/iris/handle/10665/331506
[39] Kucirka LM, Lauer SA, Laeyendecker O, Boon D, Lessler J. Variation in False-Negative Rate of Reverse Transcriptase Polymerase Chain Reaction–Based SARS-CoV-2 Tests by Time Since Exposure. Ann Intern Med. 2020; 13: M20–1495.
[40] STANDARD Q COVID-19 Ag (SD Biosensor)- literature.
[41] Bertsimas D, Dunn J, Velmahos GC, Kaafarani HMA. Surgical Risk Is Not Linear: Derivation and Validation of a Novel, User-friendly, and Machine-learning-based Predictive OpTimal Trees in Emergency Surgery Risk (POTTER) Calculator. Ann Surg. 2018; 268(4):574–583.
[42] Judson SD, Munster VJ. Nosocomial Transmission of Emerging Viruses via Aerosol-Generating Medical Procedures. Viruses. 2019; 11(10):940.
[43] Community-based health care, including outreach and campaigns, in the context of the COVID-19 pandemic. WHO and UNICEF. Available from: https://www.unicef.org/documents/community-based-health-care-outreach-campaigns-covid-19-pandemic
[44] ASHRAE 170-2017. Ventilation of Health Care Facilities. Available from: https://www.techstreet.com/ashrae/standards/ashrae-170-2017?product_id=1999079&ashrae_auth_token=12ce7b1d-2e2e-472b-b689-8065208f2e36
[45] Guidelines for Environmental Control in Health care Facilities. Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC), 2003; updated July 2019. Available from: https://www.cdc.gov/infectioncontrol/pdf/guidelines/environmental-guidelines-P.pdf