Case Report
2013
March
Volume : 1
Issue : 1
Malignant struma ovarii-A rare ovarian tumor
Jagdishwar GG, Neelima, Sathish Rao I, Vikas B, Sagar S, Arun K
Pdf Page Numbers :- 9-12
Jagdishwar GG1,*, Neelima2, Sathish Rao I3, Vikas B4, Sagar S5 and Arun K6
1Department of Surgical Oncology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad - 500003, AP, India
2Department of Obstetrics and Gynaecology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad - 500003, AP, India
3Department of Pathology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad - 500003, AP, India
4Department of General Surgery, Krishna Institute of Medical Sciences, Minister Road, Secunderabad - 500003, AP, India
5Department of General Surgery, Krishna Institute of Medical Sciences, Minister Road, Secunderabad - 500003, AP, India
6Department of General Surgery, Krishna Institute of Medical Sciences, Minister Road, Secunderabad - 500003, AP, India
*Corresponding author: Dr. Jagdishwar Goud Gajagowni, M.S, M.Ch., Department of Surgical Oncology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad - 500003, AP, India, E-mail: jagadishgdr@yahoo.com
Received 2 January 2012; Revised 8 February 2013; Accepted 20 February 2013
Citation: Jagdishwar GG, Neelima, Sathish Rao I, Vikas B, Sagar S and Arun K. Malignant Struma Ovarii- A Rare Ovarian Tumor. J Med Sci Res 2013; 1(1): 9-12. http://dx.doi.org/10.17727/JMSR.2013/1-002
Copyright: © 2013 Jagdishwar GG et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
We describe a case of 48yr old woman with malignant struma ovarii involving one ovary. Total abdominal hysterectomy and bilateral salpingo-oopherectomy was performed with histopatholgy revealing malignant struma ovary, follicular variant of papillary carcinoma.
Keywords: malignant struma; ovarian tumor; abdominal hysterectomy
Full Text
Introduction
Struma ovarii is a rare ovarian tumor observed in approximately 1% of all ovarian tumors and 2.7% of all dermoid tumors [2]. It is a highly specialized form of mature ovarian teratoma defined by the presence of thyroid tissue comprising more than 50% of the overall mass [8, 9, 10]. The vast majority of struma ovarii are benign and malignant disease is found in small percentage of cases. We report a case of malignant struma ovarii involving one ovary.
Case report
A 48-year-old woman , gravida 2, para 2 came with complaints of diarrhoea and abdomen and evaluated for the same. Upon abdomen examination, vague mobile mass was felt in lower obdomen. However, pelvic examiniation revealed no abnormality. CT abdomen revealed a large abdomino pelvic lobulated complex cystic lesion with multiple thick enhancing separations measuring approximately 10.5*11.6*7.3 cms in the midline and right paramedian region, superior to the urinary bladder with vascular supply to the lesion from left adnexa, suggesting left ovarian origin (Figure 1). It has multiple thick enhancing septations. Colonoscopy and Upper Gastro Intestinal (UGI) endoscopy are within normal limits.
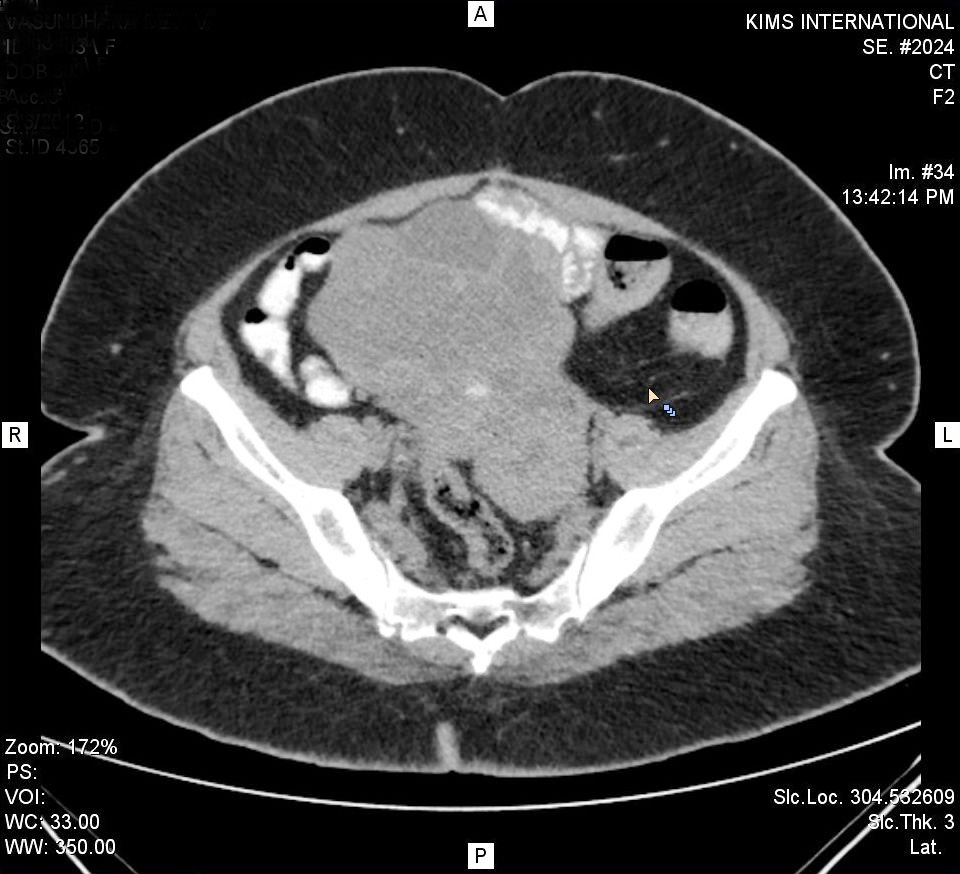
Figure 1: Superior to the lesion from left adnexa.
The patient underwent staging laparotomy including total abdominal hysterectomy and bilateral oopherectomy. Intraoperative findings are -large mass arising from left ovary mobile without any other spread. Post operatively patient developed pulmonary thromboembolism on 4th post operative day. 2D ECHO showing large mobile clot in RA/RV and CT pulmonary angio revealing extensive pulmonary thromboembolism.
Macroscopic examination showed left ovarian mass measuring 11*10*5 cms with cut section showing multilobulated cyst. Cystic areas showing colloid like material and also grey white solid areas [Figure 2] there is no breach in the capsule. Uterus, right ovary, bilateral fallopian tubes are within normal limits. Examination for ovarian tumor markers CA -125 were measured at 23.5 IU/ ml.

Figure 2: Colloidal like material and also grey white solid Areas.
Discussion
Struma ovarii is a slow growing ovarian neoplasm,with thyroid tissue as its only or the predominant (>50%) constituent. The ovarian thyroid is histologically and functionally identical to cervical thyroid [7]. This type of tumor is a highly specialised subclass of benign cystic teratoma with 95% of them remain benign while the remainder undergo malignant transformation. Struma ovarii typically presents during the fifth and sixth decades of life. The left ovary is more frequently involved than right and in 6% of instances struma ovarii are bilateral [6].
Symptoms of struma ovarii are similar to other ovarian tumors and are nonspecific in nature.They include abdiminal pain,palpable abdominal mass, abnormal vaginal bleeding,ascites (reported in one third of cases) [4], pseudo meigs syndrome ascites in the setting of hydrothorax (reported in fewer than 10% of cases). Rarely, hyperthyroidism is the presenting symptom seen in 5-8% of patients with struma ovarii [1].
Struma ovarii has no uniform diagnostic criteria. Preoperatively, the clinical diagnosis of struma ovarii is possible in patients having hyperthyroidism, but only 8% of patient with struma ovarii present with clinical hyperthyroidism [9]. Although CA-125 level was seen generally in normal range, in some patients with struma ovarii, level was elevated which may lead to suspicion of an ovarian malignancy [11]. It is difficult to distinguish between struma ovarii and dermoid cysts on the basis of their sonographic appearance. Struma ovarii has some characteristic magnetic resonance appearance of a multilobulated complex mass with thickened septa, multiple cysts of variable signal intensities and enhancing solid components [12].
Pathological examination reveals thyroid tissue as the major component of the mass,and is most commonly found in a teratoma.thyroid tisuue may be papillary,follicular,or mixed pattern and it can include elements of mucinous cystadenocarcinoma,brenner tumor,carcinoid or melanoma.birefringent crystals of calcium monohydrate are present (Figure 3) in most patients,which is considered specific for tumors of thyroid origin. Immunohistochemical staining for thyroglobulin,triiodotyronine (T3) and throxine (T4) can confirm the diagnosis.
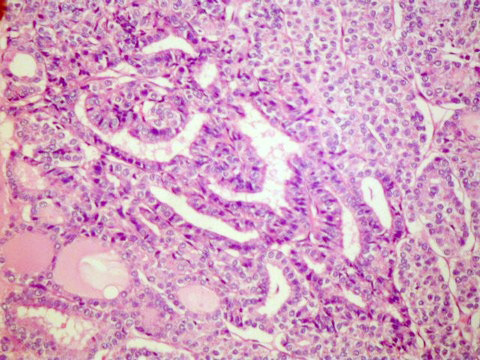
Figure 3: Birefringent crystals of calcium monohydrate are present.
Cellular atypia and hyperplasia,nuclear pleomorphism,mitotic activity and invasion into surrounding vessels or the ovarian capsule are definite clues for malignant transformation of struma ovarii.Currently,the pathological criteria used in diagnosing thyroid carcinoma are widely accepted as the standard in diagnosing malignant struma ovarii [3]. However,there is still controversy over the defining characteristics of a malignant struma ovarii. A blinded analysis of 19 histologic characteristics of thyroid tumors in 60 clinically benign and 26 clinically malignant struma ovarii cases found the majority of characteristics to be similar in both types of tumors.the clincal outcome of struma ovarii is unpredictable and cannot be predicted based on histologic features [5].
Malignant struma ovarii is divided into 3 different categories by histology.
- Papillary type is the most common and identified by "ground glass" or overlapping nuclei.
- The follicular variant of papillary carcinoma shares the same nuclear characteristics as the papillary type but has a follicular architecture.
- Follicular carcinoma is identified by follicules of mitosis around vascular and capsular structures [6].
Because of rarity of the malignant struma ovarii the optimal surgical and postoperative management has not been well defined. Main modality of treatment is surgery with total removal of tumor and staging to know extent of spread. In younger patients with tumor size less than 4 cm, cosnervative fertility preserving procedure can be done.
For patients with malignant disease on surgical pathological,postoperative adjuvant therapy with radioablative Iodine-131 is recommended. After surgical staging, a thyroidectomy is suggested before adjuvant treatment to potentiate the effects of radioablation. As normal thyroid cells preferntially uptake I-131, thyroidectomy would ensure delivery to the malignant cells. Additionally,a thyroidectomy would provide pathological confirmation that the struma is indeed ovarian origin.
The recurrence rate in patients with malignant struma ovarii who undergo surgery without subsequent radioablation has been cited as high as 50%. Thyroglobulin is the preferred tumor marker followed in patients with malignant struma ovarii and should be followed sequentially after surgery and ablation. Increase in serum thyroglobulin should be followed up with total body scanning to detect recurrence,which is treated with subsquent radioablation.Since these are rare tumors, there is no universal protocol for the treatment and follow up of patients with malignant struma ovarii,therefore more data needed to determine the prognosis and management.
Conflicts of interest
Authors declare no conflicts of interest.
References
1. Yoo SC, Chang KH, Lyu MO, Chang SJ, Ryu HS, Kim HS. Clinical characteristics of struma ovarii. J gynecol oncol. Jun 2008, 19(2):135-138.
2. Roth LM, Talerman A. The enigma of struma ovarii. Pathology. Feb 2007, 39(1):139-146.
3. Bal A, Mohan H, Singh SB, Sehgal A. Malignant transformation in mature cystic teratoma of the ovary: report of five cases and review of the literature. Arch gynecol obstet. Mar 2007, 275(3):179-182.
4. Mui MP, Tam KF, Tam FK, Ngan HY. Coexistence of struma ovarii with marked ascites and elevated ca-125 levels: case report and literature review. Arch gynecol obstet. May 2009, 279(5):753-757.
5. Shaco-levy R, Peng RY, Snyder MJ, Osmond GW, Veras E, Bean SM, et al. Malignant struma ovarii: a blinded study of 86 cases assessing which histologic features correlate with aggressive clinical behavior.arch pathol lab med. Feb 2012, 136(2):172-178.
6. Rosenblum NG, Livolsi VA, Edmonds PR, Mikuta JJ malignant struma ovarii. Gynecol oncol 1989, 32:224–227.
7. Devaney K, Snyder R, Norris HJ, Tavassoli FA proliferative and histologically malignant struma ovarii: a clinicopathologic study of 54 cases. Int j gynecol pathol1993, 12:333–343.
8. Makhija P, Rameshkumar K, Nirmala V. Histologic spectrum of struma ovarii. Indian j cancer 2000, 37:79-84.
9. Dardik RB, Dardik M, Westra W, Montz FJ. Malignant struma ovarii; two case reports and review of the literature. Gynecol oncol 1999, 73:447-51
10. Rose PG, Arafah B, Abdul-karim FW. Malignant struma ovarii: recurrence and response to treatment monitored by thyroglobulin levels. Gynecol oncol 1998, 70:425-437.
11. Mancuso a, Triolo O, Leonardi I, De vivo A. Struma ovarii: a rare benign pathology which may erroneously suggest malignancy. Acta obstet gynecol scand 2001, 80:1075-1086.
12. Kim JC, Kim SS, Park JY. MR findings of struma ovarii. Clin imaging 2000, 24:28-33
13. Volpi E, Ferrero A, Nasi PG, Sismondi P. Malignant struma ovarii: a case report of laparoscopic management. Gynecol oncol 2003, 90:191-194.