Abstract
Background: Ectopic pregnancy is one of the life-threatening conditions that can be managed expectantly, medically or surgically but a timely diagnosis is of prime importance. A tubal ectopic pregnancy occurs, when a fertilised ovum implants in the fallopian tube instead of normal uterine cavity.
Methodology: It is a prospective observational study of 60 women diagnosed with tubal ectopic pregnancy at KIMS Hospital, Secunderabad. Intrauterine pregnancy, molar pregnancy, pregnancies of unknown location, ectopic other than tubal, patients on methotrexate for any other indication or methotrexate hypersensitivity or contraindications to its administration, non-compliant patient or living far away from hospital were excluded. All the patients were managed on outpatient basis, except when the patient was haemodynamically unstable or there were signs of ruptured ectopic pregnancy clinically or on transvaginal scan (TVS). Patients with unruptured tubal pregnancy irrespective of β-hCG levels who were haemodynamically stable, with normal complete blood count (CBC), liver function test (LFT), renal function test (RFT), complied with regular follow up were selected for medical management. Patients were referred for surgical management in cases of tubal rupture and in patients whose β-hCG levels decrease is by ≤15% or a plateau was reached in serum β-hCG after two repeat doses of methotrexate.
Results: In our study success rate was 95.24% (n=40). Two patients (4.76%) with methotrexate administration, had to be taken up for surgery due to poor response, even after 2 doses. Whereas 25% of subjects required surgical management. Surgery was the ultimate option in 25%(n=15). 8.33%(n=5) who underwent laparoscopy on an elective basis, while 11.67%(n=7) underwent emergency surgery (Total =12, 20%). 18. 5%(n=3) underwent laparotomy, one of them being converted from laparoscopy to open surgery. Type of surgery done, in any case was Salpingectomy.
Conclusion: Intramuscular methotrexate has the advantage of tubal conservation and saves patients from surgical intervention. It is less invasive, does not need expertise like laparoscopy and less expensive, with the potential for considerable savings in treatment costs.
Keywords: tubal ectopic pregnancy; β-hCG; methotrexate; medical management
Full Text
Introduction
An ectopic pregnancy occurs when a fertilised ovum implants outside the normal uterine cavity [1], a common cause of morbidity and occasionally of mortality in women of reproductive age group. A tubal ectopic pregnancy occurs, when a fertilised ovum implants in the fallopian tube instead of normal uterine cavity. The diagnosis relies on a combination of ultrasound scanning and serial serum beta-human chorionic gonadotrophin (β-hCG) measurements. In India, the incidence of ectopic pregnancy is 1 in 161 (0.6%) deliveries [2]. Ectopic pregnancy is one of the few medical conditions that can be managed expectantly, medically or surgically.
Objective: To evaluate the success rate of medical management of tubal ectopic pregnancy with methotrexate and conversion rate to surgical management.
Clinical presentation
Patients with an ectopic pregnancy commonly present with pain and vaginal bleeding between 6 and 10 weeks gestation and 9% have no symptoms. Ruptured ectopic pregnancy should be strongly suspected if a woman has a positive pregnancy test and presents with syncope and signs of shock including tachycardia, pallor and collapse. A bimanual examination may reveal tenderness on cervical excitation and an adnexal mass.
Diagnosis
1. Trans vaginal ultrasonography in the absence of intrauterine pregnancy (IUP) with non homogenous adnexal mass, adnexal sac containing yolk sac or fetal pole, & free fluid is suggestive of ectopic pregnancy (Figure 1). 2. In a normal pregnancy, serum β-hCG value a minimum acceptable increase for 48-hours is between 50% and 66%. Absence of this expected rise suggests early pregnancy failure. 3. Diagnostic laparoscopy is the ‘gold standard’ investigation in ectopic pregnancy (Figure 2). 4. Endometrial biopsy in selected cases of pregnancy of un known location with absence of chorionic villi in E.B, in the presence of a static β-hCG is suggestive of an ectopic pregnancy.
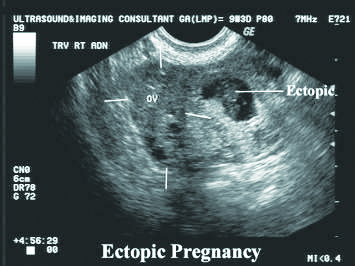
Figure 1: Transvaginal ultrasound showing right tubal ectopic pregnancy.
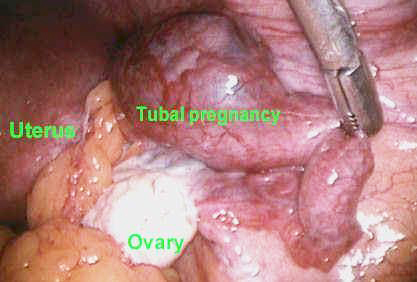
Figure 2: Laparoscopic view of tubal ectopic pregnancy.
Materials and methods
It is a prospective observational study. Women between 15-49 years of age with diagnosis of tubal ectopic pregnancy presented to KIMS hospital, Secunderabad were included. Intrauterine pregnancy, molar pregnancy, pregnancies of unknown location, ectopic other than tubal pregnancy, patients on methotrexate for any other indication or methotrexate hypersensitivity and contraindications to its administration, non-compliant patient/ patient living far away from hospital were excluded. All the patients were managed on outpatient basis, except when the patient was hemodynamically unstable or there was suggestion of rupture of ectopic pregnancy clinically or on transvaginal ultrasonography. All the patients were advised not to travel, to avoid sexual intercourse and to return to the hospital if they experience a significant increase in abdominal pain. After diagnosing patients with unruptured tubal pregnancy irrespective of β-hCG levels who were hemodynamically stable, normal complete blood count, liver function test, renal function test, compliance for regular follow ups were selected for medical management.
Patients fit for medical management received a single dose of intramuscular methotrexate with a dose of 50 mg/m2 surface area. Serum β-hCG concentrations were measured by radioimmunoassay (RIA) on days 1, 4 and 7, after the methotrexate injection. If the β-hCG level declined by at least 15% between days 4 and 7, the treatment was deemed successful, and weekly β-hCG and ultrasonography done until the β-hCG levels were below 5 mIU/ml.
The woman was referred for surgical treatment in cases of tubal rupture and in patients whose serum β-hCG levels decreased by ≤15% or a plateau was reached without any decrease after two repeat doses of methotrexate. Patients not fit for medical management were managed surgically either by laparoscopy or by laparotomy. Follow up was done by sonography in both expectant and medical management modalities.
Statistical analysis
Data analysis was carried out using the Statistical Package for Social Science 16.0 (SPSS, Chicago, IL). Normally distributed data were evaluated with t-test and ANOVA test. Non parametric tests Mann Whitney, Kruskal Wallis H test were used for data which were not normally distributed. Categorical data were evaluated with chi square tests. p≤0.05 was statistically significant.
Results
A total of 60 patients were enrolled into the study. Among all the variables, β-hCG was the only variable, statistically different among the three groups. Majority of the patients were distributed in age group of 26-30 years, but statistically could not be of any importance in between the groups. Patients were equally distributed among nulliparous or monoparous groups. Amenorrhea duration was almost equally distributed on either side of 6 weeks (Table 1).
Table 1: Comparison of age, gravidity, parity, amenorrhea (in weeks), BMI, β-hCG-day 0 (IU/l) for determining mode of management.
In our study, a total of 60 patients were enrolled into various modalities: Expectant (15%;n=9), medical (63.33%;n=38), surgical (21.67%;n=13). After completion of the study, the percentage in each modality with successful outcome were 8.33%, 66.67% and 25% respectively. Pretreatment level of serum hCG varied from 438- 28842 IU/l with a mean of 5791.78±6389.82. Patients were equally distributed (38.33%;n= 23) between β-hCG values of 1001-5000 IU /l and >5000 IU/l. Expectant management was applied to 15% of patients, but only 8.3% could be managed successfully. 4(6.66%) patients with expectant management, had to be converted to methotrexate group due to increasing trend of β-hCG. None of the patients proposed for expectant line of management had to undergo surgery.
Comparison of three groups of β-hCG among the three modalities of management was statistically significant (Table 2). As the β-hCG values increases, need for surgical management increases. But, even then the medically managed group is significant statistically.
Table 2: Comparison of β-hCG values in different modalities of treatment.
Diameter of the mass was not different in the single dose vs double dose received groups (3.29±0.92 cm vs 4.03±1.18 cm; p=0.09). Previous history of ectopic (p=0.053) or past use of methotrexate (p=0.95) could not decide the number of doses. No difference in the number of doses required noted when compared between two groups having diameter of sac ≤4 cm and >4cm (Table 3).
Table 3: Comparing size of ectopic mass in determining the number of inj.methotrexate doses required for medical management.
10% patient had history of prior one dose of methotrexate and 0.16% patient had history of two doses of methotrexate. with p value -0.95, signifies that the use of methotrexate in past did not reduce the need for administration of second dose (Table 4).
Table 4: To asses previous history of methotrexate use in determining no of required in medical management.
In our study we found that day 1 β-hCG variation was not the determining factor for assessing the number of doses. Number of doses required were assessed by subsequent day-4 and day-7 β-hCG levels (Table 5).
Table 5: To determine initial (day -1) β-hCG values in determining no of inj. methotrexate doses required in medical management.
Discussion
According to studies, expectant management can be applied successfully in 9-26% of all ectopic pregnancies after careful selection of cases [3-5]. In our study, expectant management was applied to 15% of patients, but only 8.3% could be managed successfully. 4(6.66%) of patients with expectancy as line of management, had to be converted to methotrexate group due to increasing trend of β-hCG. None of the patients proposed for expectant line of management had to undergo surgery. The mean duration for resolution of ectopic with expectant management is under 3 weeks [6], comparable to that noted in our study (2.2 weeks).
In medical management group with successful outcome, 85%(n=34) received one dose whereas 15%(n=6) received 2 doses, similar to observation made by Lipscomb et al. [7] in his study [81%(n=283), 17%(n=60) respectively]. In another study [8] 45(75%) cases, a single-dose methotrexate was applied and in 15(25%) cases a double-dose methotrexate was applied.
Mean β-hCG - day 1 in patients treated with methotrexate in our study is 4900.6 IU/l(450-15006), which is far higher when compared to other studies (844.1,1414.7,1293.9) [9-10]. Mean β-hCG -Day 4, β-hCG -Day 7 were 4285.23(399-14121), 3414.28(290-15382) IU/l respectively which were also higher when a similar study [8] was taken into consideration [1129.6(37-5460), 594.5(6-4075)IU/l respectively].
Previous history of ectopic (p=0.053) or past use of methotrexate (p=0.95) could not decide the number of doses. Side effects noted in 23.8% of patients using methotrexate which is far lower compared to study from Singapore [10] (78.2%). Pain abdomen (16.66%), mucositis (9.52%) appeared to be most common but lesser than observed in the latter (28.2%, 19.1% respectively) [11].
The success rate using methotrexate for treatment of ectopic pregnancy has been reported to be between 75% and 96% in properly selected patients [4, 5]. In our study success rate was 95.24%(n=40) only 2 patients (4.76%) with methotrexate administration had to be taken up for surgery due to poor response (the decrease in β-hCG values by ≤15% or a plateau was reached in serum β-hCG after two doses of methotrexate). Whereas 25% required surgical management following poor medical management in an Indian study [12] and 14.5% in a Singapore based study [10].
Ruptured ectopic is noted in 11.67%(n=7) of our patients which is far less than mentioned in various works (30.77%-66%) [13]. Surgery was the ultimate option in 25%(n=15). 8.33%(n=5) underwent laparoscopic surgery on an elective basis while 11.67%(n=7) underwent emergence basis (Total =12,20%). 5%(n=3) underwent laparotomy, one of them being converted from laparoscopy to open surgery. Surgery done, in any case, was Salpingectomy.
Conclusions
Medical management of tubal ectopic pregnancy with intramuscular methotrexate has the advantage of tubal conservation with success rate of 95.24% with very few side effects and saves patients from surgical intervention. It is less invasive, does not need expertise like laparoscopy and less expensive with a potential for considerable savings in treatment costs, and avoid hospitalization.
Acknowledgement
The Departments of Obstetrics & Gynaecology, Radiology & Imageology, Krishna Institute of Medical Sciences, Secunderabad, India.
Conflicts of interest
There are no conflicts of interest and all the authors were in tone of study.
References
[1] Vanitha NS, Duncan WC, Emma Kirk, Shephard LA, Horne AW. Diagnosis and management of ectopic pregnancy. J Fam Plann Reprod Health Care. 2011; 37(4): 231–240.
[2] Majhi AK, Roy N, Karmakar KS, Banerjee PK. Ectopic Pregnancy: An analysis of 180 cases. J Indian Med Assoc. 2007; 105(6):308–314.
[3] Makinen JI, Kivijarvi AK, Irjala KMA. Success of nonsurgical management of ectopic pregnancy. Lancet. 1990; 335(8697):1099.
[4] Ylöstalo P, Cacciatore B, Sjöberg J, Kääriäinen M, Tenhunen A, et al. Expectant management of ectopic pregnancy. Obstet Gynecol. 1992; 80(3 Pt 1):345–348.
[5] Shalev E, Peleg D, Tsabari A, Romano S, Bustan M. Spontaneous resolution of ectopic pregnancy: natural history. Fertil Steril. 1995; 63(1):15–19.
[6] Marvelos D, Memtsa M, Helmy S, Derdelis G, Jauniaux E, et al. β-hCG resolution times during expectant management of tubal ectopic pregnancies. BMC Womens Health. 2015; 15:43.
[7] Lipscomb GH, McCord ML, Stovall TG, Huff G, Portera SG, et al. Predictors of success of methotrexate treatment in women with tubal ectopic pregnancies. N Engl J Med. 1999; 341(26):1974–1978.
[8] Aybatl A, Kaplan PB, Alicik M, Sayın NC, Yüce MA. Single dose methotrexate in treatment of ectopic pregnancy: Review of 32 cases. Balkan Med J. 2011; 28:10–13.
[9] Aydogmus S, Eris S, Aydogmus H, Tanrısever GG, Halime Sen Selim, et al. Management and results of ectopic pregnancy adapted by clinical guidelines: Two years experience of University Hospital in Turkey. Open J Obstet Gynecol. 2014; 4:766–770.
[10] Thia EW, Loi K, Wang JJ, Siow A. Methotrexate treatment for ectopic pregnancy at the KK Women’s and Children’s Hospital, Singapore. Singapore Med J. 2009; 50(11):1058–1063.
[11] Shah SR, Sonara S, Patel B, Patel N. Medical management of ectopic pregnancy with methotrexate. Indian Journal of Clinical Practice. 2014; 24(11):1048–1052.
[12] Talwar P, Sandeep K, Naredi N, Duggal BS, Jose T. Systemic methotrexate: An effective alternative to surgery for management of unruptured ectopic pregnancy. Med J Armed Forces India. 2013; 69(2):130–133.
[13] Gaddagi RA, Chandrashekhar AP. A clinical study of ectopic pregnancy. J Clin Diagn Res. 2012; 6(5):867–869.