Original Research
2019
June
Volume : 7
Issue : 2
Micro vascular decompression for trigeminal neuralgia: Preliminary experience
Raghavendra H, Varsha KS, Shivender Sobti
Pdf Page Numbers :- 32-35
Raghavendra H1,*, Varsha KS2 and Shivender Sobti3
1Department of Neurosurgery, ESIC Medical College and Super Speciality Hospital, Hyderabad-500038, Telangana, India
2Department of Anaesthesiology, ESIC Medical College and Super Speciality Hospital, Hyderabad-500038, Telangana, India
3Department of Neurosurgery, Christian Medical College & Hospital, Ludhiana, Punjab, India
*Corresponding author: Dr. Raghavendra H, Department of Neurosurgery, ESIC Medical College and Super Speciality Hospital, Hyderabad-500038, Telangana, India. Email: harpanahalli.raghavendra@gmail.com
Received 28 December 2018; Revised 25 February 2019; Accepted 7 March 2019; Published 18 March 2019
Citation: Raghavendra H, Varsha KS, Sobti S. Micro vascular decompression for trigeminal neuralgia: Preliminary experience. J Med Sci Res. 2019; 7(2):32-35. DOI: http://dx.doi.org/10.17727/JMSR.2019/7-7
Copyright: © 2019 Raghavendra H et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: To assess the outcome of micro vascular decompression (MVD) for trigeminal neuralgia (TN) in the initial experience.
Methods: Between March 2016 and March 2018, 16 patients who were affected, by trigeminal neuralgia and underwent micro vascular decompression in the Department of Neurosurgery at tertiary centre were enrolled in the study. A Barrow Neurological Institute pain score was calculated pre and post-operatively for all patients.
Results: During a 24-month period, 16 patients underwent MVD for TN. All patients were operated on by the author. The patients included 11 females and 5 males, with a mean age of 50 years. The mean time from diagnosis to surgery was 3.5 years. The mean time from first neurosurgical clinic review and operation was 204 days, all the patients had a vascular loop identified on pre-operative MRI, all patients underwent micro vascular decompression. There was an average follow up of 16.37 months. A post-operative Barrow score of ≤3 was considered a satisfactory outcome, out of 16 patients 15 had satisfactory outcome.
Conclusions: We consider MVD to be gold standard treatment option in patients with TN, refractory to medical management.
Keywords: Micro vascular decompression; trigeminal neuralgia; multiple sclerosis; medical management
Full Text
Introduction
Trigeminal neuralgia (TN) is a rare chronic pain disorder, characterised by paroxysms of severe, lancinating pain in the distribution of the trigeminal nerve. Most commonly, the second and third branches of the trigeminal nerve are affected. Paroxysms of pain may be related to tactile stimuli such as hair combing, shaving or a cold wind against the patients face. The pain associated with TN is so severe that reports of patients committing suicide have been published in the literature [1]. The estimated annual incidence of TN is 27 per 100,000 person years, with peak incidence between the ages of 50 and 60 [2]. The vast majority of TN cases are due to micro vascular compression of the root entry zone of the trigeminal nerve by vascular structures [3]. TN is seen with increased frequency in patients suffering from multiple sclerosis (MS), where it has an estimated prevalence of 1%-6.3%, and in MS patients the condition may be bilateral [4, 5]. TN may also occur secondary to space occupying lesions at the cerebello-pontine angle such as epidermoid cysts, meningiomas or vestibular schwannoma [6]. The diagnosis of TN is a clinical one, based on history and examination, However, 3D volumetric MRI studies may be used to investigate for micro vascular compression of the nerve, and for rarer, secondary causes of TN [7]. The first line treatment of TN involves medical management with carbamazepine or other anti-epileptic drugs, which have been demonstrated to be effective for pain reduction in patients with TN [8]. Although medical management has been demonstrated to be effective, 75% of TN patients ultimately undergo a surgical procedure for the relief of their pain [9]. The most commonly performed surgical procedure is microvascular decompression, where the vascular loop overlying the trigeminal nerve is displaced away from the root entry zone. Other surgical options for the treatment of TN include balloon compression of the nerve root, radiofrequency thermocoagulation, glycerol rhizolysis and stereotactic radiosurgery [10].
The aim of this paper is to report the outcomes of patients treated with microvascular decompression in a small volume regional neuroscience unit, at the ESIC Medical college & Super speciality Hospital, Hyderabad, between March 2016 and March 2018.
Materials and methods
We retrospectively reviewed electronic records and operation notes of patients who underwent micro vascular decompression (MVD) by the author for TN between March 2016 and March 2018. The procedure itself was performed under a general anaesthetic, with the trigeminal nerve ganglion accessed by means of a retro mastoid sub occipital craniectomy. Following this, the Dura mater was opened to allow access to the cerebellopontine angle. The cerebellum was retracted and CSF was released from cerebello medullary cistern, and the trigeminal nerve was identified with the use of a neurosurgical microscope. Following identification of the nerve, it was carefully inspected and any offending vessels are dissected off its surface: the superior cerebellar artery is most commonly implicated, although compression by the anterior inferior cerebellar artery, as well as the superior petrosal veins has also been reported [11]. Following dissection of the vascular structures from the trigeminal nerve ganglion, muscle graft is interposed between the vessel and the nerve, to maintain separation [12]. Follow up clinic reviews were used for assessment of outcome measures in this study. A Barrow Neurological Institute pain score was calculated pre and post-operatively for all patients.
Results
During a 24-month period, 16 patients underwent MVD for TN. All patients were operated on by the author. The patients included 11 females and 5 males, with a mean age of 50 years (range 25-71) (Figure 1). The mean time from diagnosis to surgery was 3.5 years (range 2.2-12 years). The mean time from first neurosurgical clinic review and operation was 204 days (range 51- 336 days).
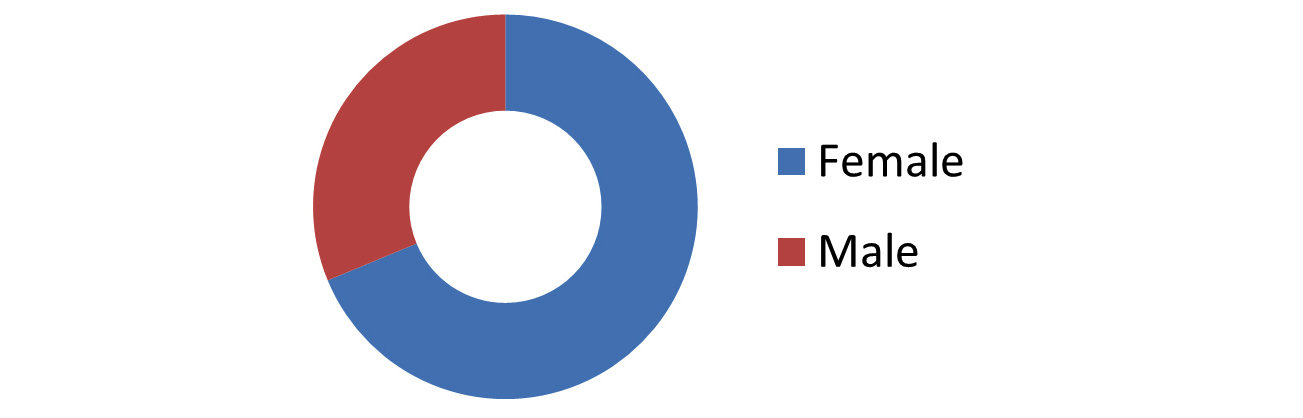
Figure 1: Showing sex distribution of trigeminal neuralgia.
All the patients had medical therapy alone prior to micro vascular decompression. All the patients had a vascular loop identified on pre-operative MRI (Figure 2). All patients underwent microvascular decompression by retromastoid suboccipital craniectomy (Figure 3). There was an average follow up of 16.37 months. A Barrow Neurological Institute pain score was calculated for all patients. Pre-operatively 16 patients had a score of 5, 4 patients had a score of 4. Postoperatively, at last clinic follow up (minimum one year), 11 patients had score of 1, two patients each in score 2 & 3. One patient had score 4. A post-operative Barrow score of ≤3 was considered a satisfactory outcome, out of 16 patients 15 had satisfactory outcome (Figure 4).
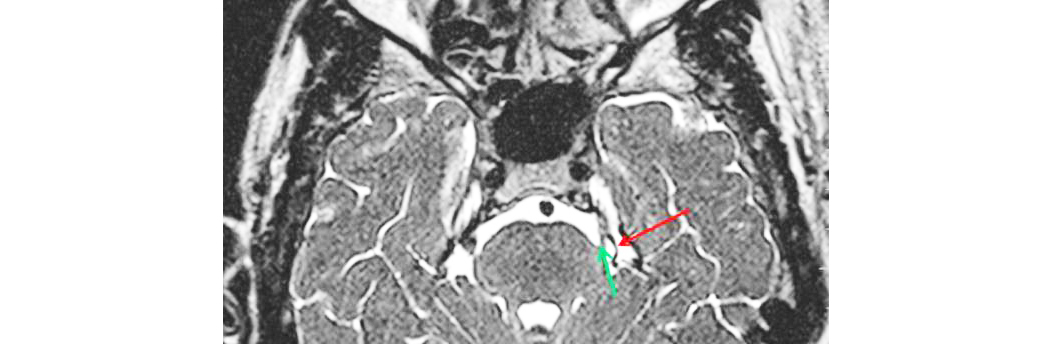
Figure 2: MRI showing neurovascular conflict (red arrow: vascular loop; green arrow: trigeminal nerve).
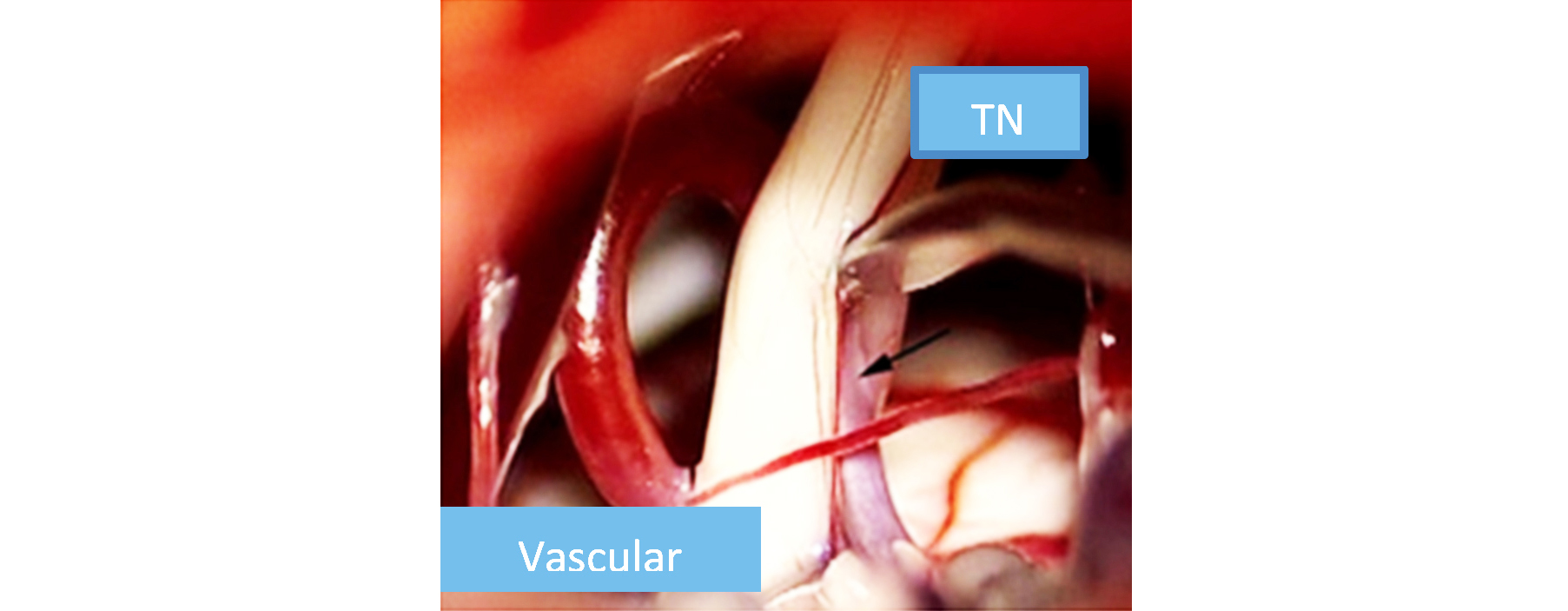
Figure 3: Intraoperative picture showing vascular loop abutting trigeminal nerve.
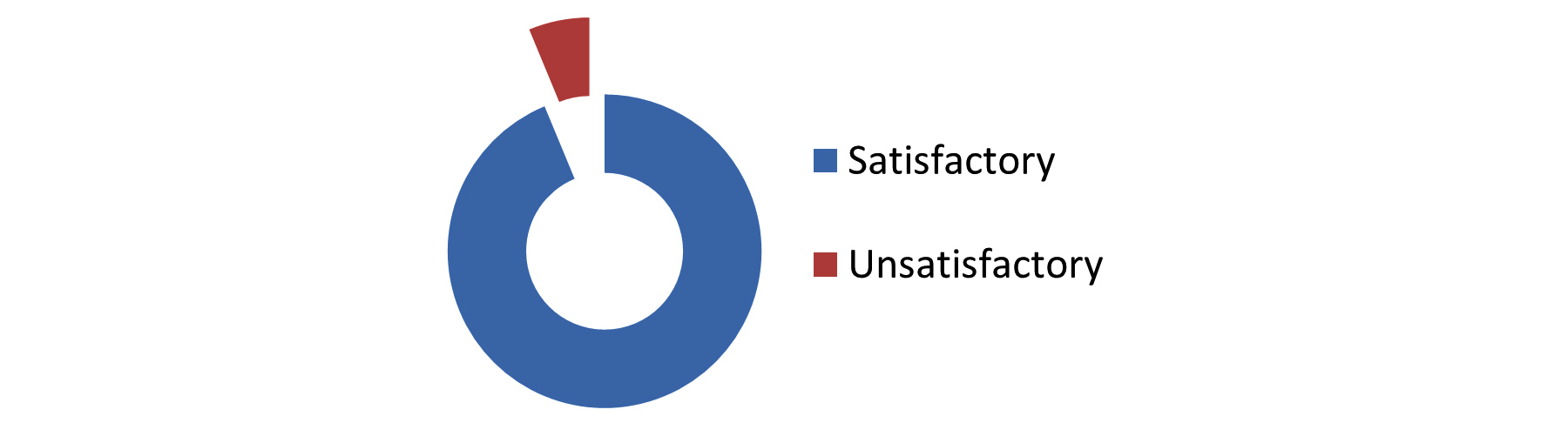
Figure 4: Outcome of micro vascular decompression.
In terms of other post-operative complications (Table 1), 2 patients developed minor wound infections treated with short course antibiotics, one patient developed transient hearing loss which resolved with time and one patient had cerebral spinal fluid (CSF) leak from nostril for which lumbar drain was placed and subsequently leak subsided.
Table 1: Post-operative complications.
|
Complication
|
Number
|
|
Death
|
00
|
|
Facial palsy
|
00
|
|
Hearing loss
|
01
|
|
CSF leak
|
01
|
|
Minor wound
|
02
|
|
Hematoma
|
00
|
|
Contralateral pain
|
00
|
Discussion
Micro vascular decompression is a surgical procedure, undertaken following failure of medical therapy, or when medical therapy has intolerable adverse effects, for TN. All of our patients have an MRI pre-operatively, to assess for the presence of a vascular loop abutting the trigeminal nerve ganglion: the identification of a vascular loop compressing the trigeminal nerve has been shown to be associated with an improved outcome following MVD [13]. In addition to the open approach, fully endoscopic micro vascular decompression has also been described allowing a less invasive approach to this procedure, without an increased risk of complications according to some published evidence [14]. Due to the proximity to cranial nerve VIII, post-operative hearing loss is a possibility, with a reported incidence in the literature of 1.1-1.3% [12, 15]. Brain-stem auditory evoked responses can be monitored intra-operatively in an effort to prevent hearing loss. Other potential complications include facial palsy, facial sensory loss, postoperative haemorrhage, CSF leak and meningitis [12]. In this study, at an average of 204 days post-operatively, 15 patients had a satisfactory outcome (Barrow score ≤3), while 1 reported an unsatisfactory outcome. A 2010 study of 372 patients treated with micro vascular decompression between 1982 and 2005 for TN refractive to medical therapy reported that 84% of patients were pain-free, without the need for medication, at one year, and that 71% were pain-free without the need for medication at 10 years post-operatively [13]. In terms of post-operative complications (Table 1), those most commonly encountered in this cohort of patients were; CSF leak (1 patient), wound infection (2 patients), hearing loss (1 patient). No patients developed a facial palsy following their operation. The limitations of this study are the small sample size, the retrospective nature of the study and the relatively short follow-up period. Although we consider MVD to be gold standard treatment option in patients with TN refractory to medical management or who have not responded to MVD, alternative, less invasive procedures are available, and can be considered in the elderly patient with significant co-morbidities or in patients with MS, who often have poor results following MVD [16]. Balloon micro-compressions is a procedure undertaken percutaneous, under fluoroscopic guidance, aiming to crush the nerve against the skull base, as it passes through the foramen ovale. Long term outcomes are not as favourable as those with MVD.
A further treatment modality utilised when MVD is not considered suitable is the use of stereotactic radiosurgery, delivering targeted radiation to the trigeminal nerve root entry zone. It is less effective than MVD, with rates of pain relief, without the use of medication, at ten years reported in a recently published series to be 51.5% [17]. There is also a delay in the onset of pain relief following the procedure, compared with MVD and balloon compression, that should lead to relief of pain immediately after the procedure [18].
Conclusion
In conclusion, we consider MVD to be gold standard treatment option in patients with TN refractory to medical management or who have not responded to MVD, alternative, less invasive procedures are available, and can be considered in the elderly patient with significant co-morbidities it is clear that micro vascular decompression is an effective treatment for TN refractory to medical management. Neurologists and other physicians involved in the management of TN should consider prompt referral to a neurosurgical unit following the failure of medical therapy.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Zakrzewska JM. Insights: facts and stories behind trigeminal neuralgia. Gainesville, Florida: Trigeminal Neuralgia Association; 2006.
[2] Hall GC, Carroll D, Parry D, McQuay HJ. Epidemiology and treatment of neuropathic pain: the UK primary care perspective. Pain. 2006; 122(1- 2):156–162.
[3] Zakrzewska JM, Coakham HB. Microvascular decompression for trigeminal neuralgia: update. Cur Open Neural 2012; 25(3):296–301.
[4] Putzki N, Pfriem A, Limmroth V, Yaldizli O, Tettenborn B, et al. Prevalence of migraine, tension-type headache and trigeminal neuralgia in multiple sclerosis. Eur J Neurol. 2009; 16(2):262–267.
[5] Nurmikko TJ, Eldridge PR. Trigeminal neuralgia--pathophysiology, diagnosis and current treatment. Br J Anaesth. 2001; 87(1):117–132.
[6] Cheng TM, Cascino TL, Onofrio BM. Comprehensive study of diagnosis and treatment of trigeminal neuralgia secondary to tumors. Neurology. 1993; 43(11):2298–2302.
[7] Zeng Q, Zhou Q, Liu Z, Li C, Ni S, et al. Preoperative detection of the neurovascular relationship in trigeminal neuralgia using three-dimensional fast imaging employing steady-state acquisition (FIESTA) and magnetic resonance angiography (MRA). J Clin Neurosci. 2013; 20(1):107–111.
[8] Wiffen PJ, Derry S, Moore RA, McQuay HJ. Carbamazepine for acute and chronic pain in adults. Cochrane Database Syst Rev. 2011; 19(1):CD005451.
[9] Broggi G, Ferroli P, Franzini A. Treatment strategy for trigeminal neuralgia: a thirty years’ experience. Neurol Sci. 2008; 29 Suppl 1:S79–S82.
[10] Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ. 2014; 348:g474.
[11] Thomas KL, Vilensky JA. The anatomy of vascular compression in trigeminal neuralgia. Clin Anat. 2014; 27(1):89–93.
[12] Greenberg MS, editor. Handbook of neurosurgery. 7th ed. Stuttgart: Thieme Publishers; 2010.
[13] Sarsam Z, Garcia-Fiñana M, Nurmikko TJ, Varma TR, Eldridge P. The long-term outcome of microvascular decompression for trigeminal neuralgia. Br J Neurosurg. 2010; 24(1):18–25.
[14] Bohman LE, Pierce J, Stephen JH, Sandhu S, Lee JY. Fully endoscopic micro vascular decompression for trigeminal neuralgia: technique review and early outcomes. Neurosurg Focus. 2014; 37(4):E18.
[15] Barker FG, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD. The long-term outcome of micro vascular decompression for trigeminal neuralgia. N Engl J Med. 1996; 334(17):1077–1083.
[16] Broggi G, Ferroli P, Franzini A, Nazzi V, Farina L, et al. Operative findings and outcomes of micro vascular decompression for trigeminal neuralgia in 35 patients affected by multiple sclerosis. Neurosurgery. 2004; 55(4):830–838.
[17] Régis J, Tuleasca C, Resseguier N, Carron R, Donnet A, et al. The very long-term outcome of radiosurgery for classical trigeminal neuralgia. Stereotact Funct Neurosurg. 2016; 94(1):24–32.
[18] Hannan C, Shoakazemi A, Quigley G. Microvascular decompression for trigeminal Neuralgia: A regional unit’s experience. Ulster Med J 2018; 87(1):30–33.