Full Text
Introduction
Sir James Paget (1814-1899) had eminently described Paget disease of bone and also Paget diseases of the nipple. He presented a paper to Royal Medico Chirurgical Society on 14 November 1878 on a form of chronic inflammation of bones” and said that is osteitis deformans. It is a chronic disease of skeleton, in people of Anglo-Saxon descent who live in certain geographic areas such as UK, USA, Australia, New Zealand and Western Europe and is not common in Scandinavia, China, Japan and India.
Historical background in India
In India, Vyagreswarudu C has published for the first time, “a case report” on Paget disease in Indian Journal of Surgery 15:239, 1953. Doctors Ramamurthi and Viswanathan, (1957) has published a case on Paget of Axis of Vertebra. Bharadwaj has published monostotic Paget disease of bone in Indian Journal of Medical Association (1964). Donaldson JR, Bond WM et al., have published on ‘Paget disease of bone” in Indian Journal of Surgery (1969). Shanmuga Sundaram TK has published an article on Paget disease in Indian Journal of Orthopedic surgery (1970). Subramanian MV, Subbarao K et al. have published on “Paget disease of bone” in Indian Journal of Radiology (1972). Krishna Murthy K, Mansharamani GG et al. have published on “Paget disease (case report)” in Indian Journal of Medical Sciences (1972). Gupta BB, Lamba GS, et al. have published on “Paget disease of bone” in Indian Journal of Radiology (1974). Ranga Chari P et al. have published on “Paget disease of bone” in Indian Journal of Orthopedics (1975). Pant HC, Sharma SP et al. have published on “osteogenic sarcoma (Paget)” in Indian Medical Gazette (1978). Mohan V has published on “Paget disease of bone in India”, The Clinician (1980). Kundu J has published on “monostotic Paget disease of tibia” in Indian Journal of Radiology & Imaging (1985). Virendra Mohan, Gupta SK et al. have published on “Paget disease of done” in Indian Journal of Radiology and Imaging (1986). Shah HR, Patwa PC et al. have published on Paget disease of calcaneum (Letter to Editor) in Indian Journal of Radiology and Imaging ( 1994). Subbarao Kakarla has published on “Paget disease” in CME Proceedings of Medwin Hospitals, Hyderabad (1994).
Hence, Paget disease of the skeleton is rare in India. During 12 years (1986-98), 78 cases of Paget were seen at Nizam’s Institute of Medical Sciences (NIMS), Hyderabad.
Etiology
About 40-50% of persons with the inherited version of Paget disease had a protein involved in regulating osteoclast functioning, called p62. About 10-15% of persons that develop the disease without any family history also have a mutation in the SQSTM1 gene. Etiological factors include racial, geographical, climatic, viral and hereditary.
Paget disease can affect any bone from head to toe. It is often encountered in axial skeleton and long bones. It may be monostotic or polyostotic. It can affect the entire bone or a part of the bone.
Pathophysiology
Three phases of Paget disease have been described. One lytic, two mixed lytic and sclerotic and three completely sclerotic. In the lytic phase, the normal bone is replaced by osteoclasts and bone turnover rates increased by 20 times of normal. In the second phase, besides lytic areas new bone formation occurs from osteoblasts. The sclerotic bone is abnormally laid down with heavy collegan formation. Fibers are displayed in a haphazard way rather than linearly as occurs in normal bone. A high degree of bone turnover occurs due to the osteoclastic and osteoblastic activities. Paget called this process as “metabolic madness”. In the third phase, bone formation dominates in a disorganized pattern. This new bone is weaker than normal bone. There is infiltration of excessive fibrous connected tissue with blood vessels extending into the bone marrow.
“The structure appears to have been almost entirely removed & laid down afresh in a different plane and in a different layer mould” stated Paget.
Laboratory findings
Alkaline phosphotase in the blood is increased. However, calcium, phosphate and amino transferees are normal. Serum and urinary hydroxyproline is increased. The markers of bone turnover in urine namely “Deoxypyridinoline” are increased.
Clinically, it may present as pain or swelling or deformity depending upon the bone involved. When it involves the vertebra, it may compress the spinal cord and neurological symptoms may appear. Most of the time Paget involving the bone is asymptomatic in early stages and is found incidentally on a radiograph taken for some other reasons.
Radiological findings
Radiological and imaging investigations include conventional radiography, C.T., M.R.I. and radio-nuclear studies. Radiographic changes are noted in all three phases and are parallel to pathological findings. The lytic phase in the skull is named as “osteoporosis circumscripta” (Figure 1a,b).
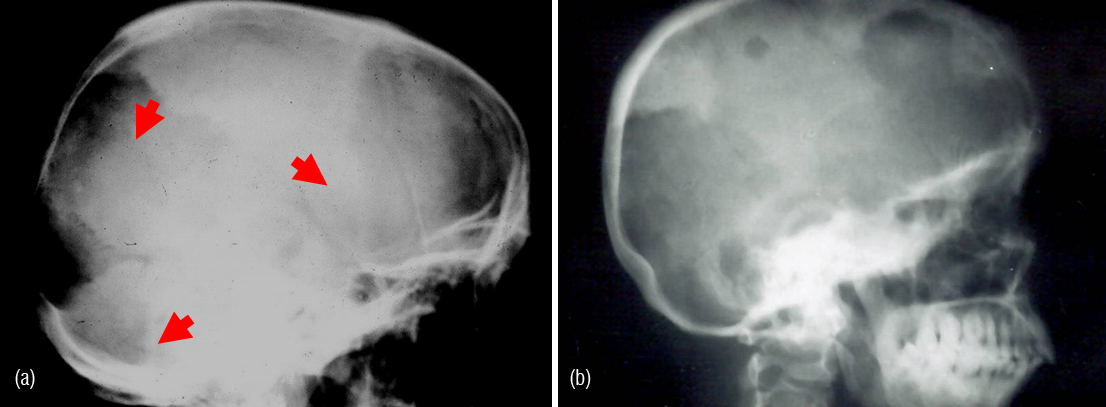
Figure 1: (a) Paget- lateral skull – lucent areas are called areas of “osteoporosis circumscripta”. (b) Paget – lateral skull - osteoporosis circumscripta.
The lucent areas are of “geographical pattern” with “cotton wool” appearance. Enlargement of involved bone is characteristic.
In the sclerotic phase, diffuse widening of the diploic space with thickening of the outer and inner tables of the skull is noted (Figure 2a,b).
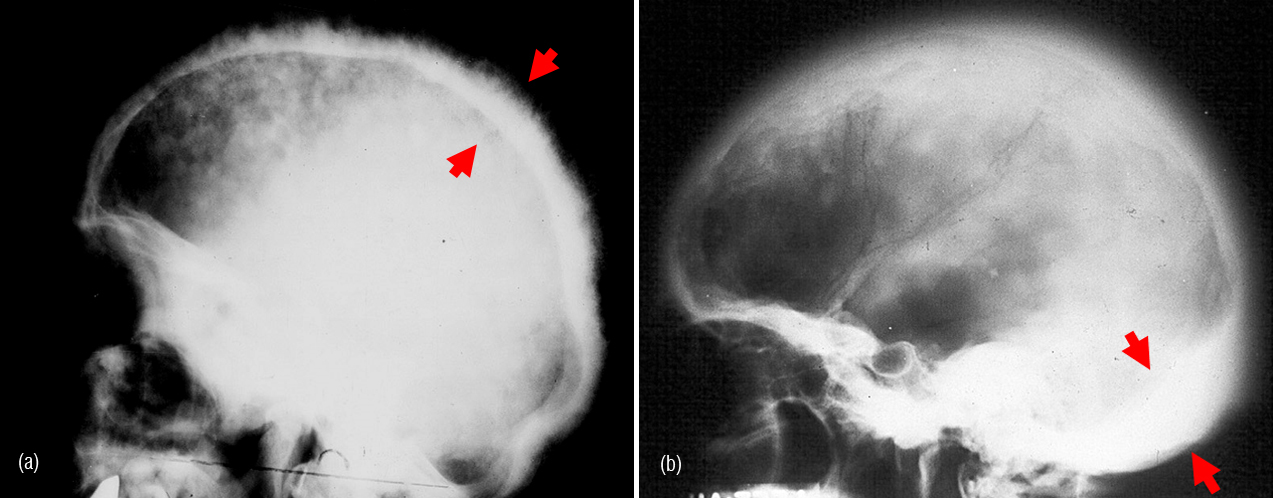
Figure 2: (a) Paget skull– diffuse sclerosis with wide diploic space. (b) Page’s skull with diffuse sclerosis and thickened occiput extending to the base.
The facial, nasal bones, maxilla and mandible are involved with sclerosis and expansion.
In the clavicles also the lytic phase is lucent and pathological fracture may occur. In the sclerotic phase, expansion of the clavicle occurs and the process may extend to either end of the clavicle (Figure 3a). In the scapula and long bones of the upper extremity all the three phases may be noted (Figure 3b). Whatever the phase may be, the process extends to one end of the long bones. Similar changes occur in the bones of the hands (Figure 3c,d).
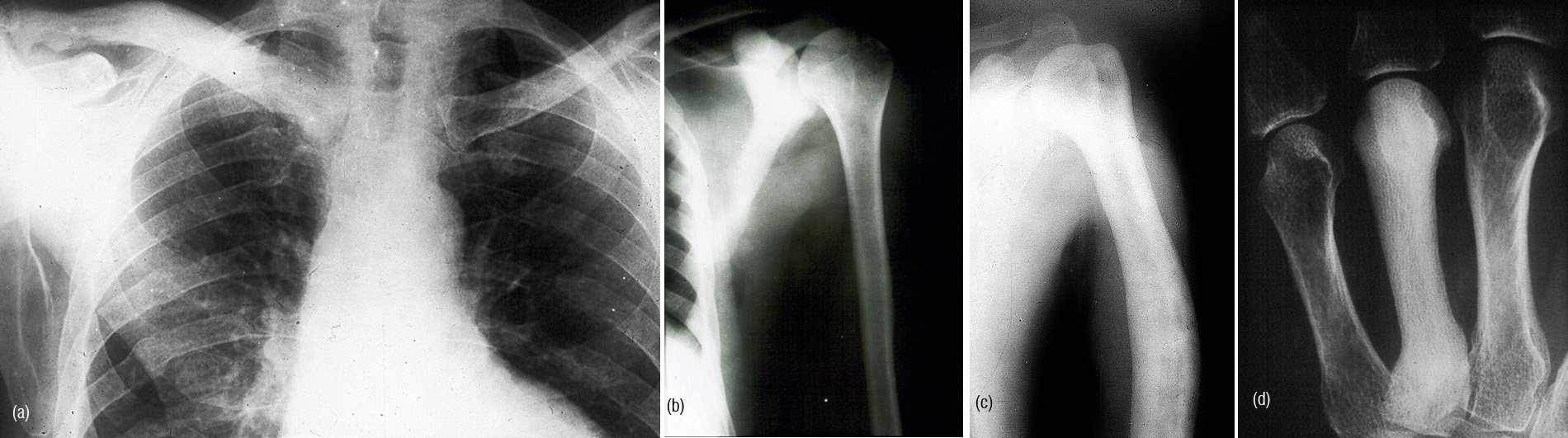
Figure 3a: Paget - sclerotic and deformed right clavicle. (b) Paget scapula - sclerotic phase- note the process extends to the articular end. (c) Paget of humerus. Sclerosis and lateral bowing is noted. (d) Paget – 4th metacarpal – sclerotic phase.
In the axial skeleton, in the lytic phase, compression fracture of the vertebra may be noted (Figure 4a). In the mixed phase, a picture frame appearance has been descried with a sclerotic outer border and lucent matrix of the vertebra (Figure 4b). The vertebra is larger and may show characteristic “Picture Frame Appearance” (Figure 4c). In the sclerotic phase, an ivory type of vertebrae is noted (Figure 4d).
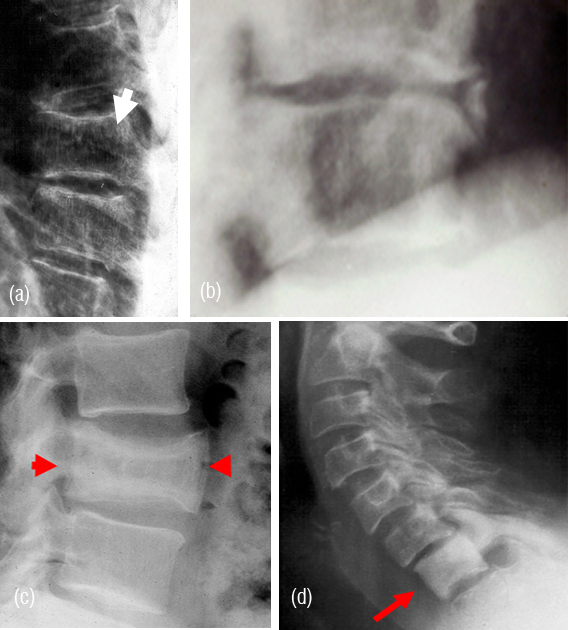
Figure 4: (a) Lytic type of Paget. Notice the body is larger (arrow). (b) Mixed & lytic type of Paget involving the vertebra. (c) Picture frame appearance of Paget. (d) Paget – C7 - ivory vertebra.
In all the phases the bones are expanded. Similar changes occur in the sacrum and coccyx. In the pelvis, the iliopectenial line is characteristically involved. Other changes are the same in iliac wings, acetabulae, pubic bones and ischia (Figure 5).

Figure 5: Paget involving all the bones of the pelvis and proximal femora.
In the lower extremities, in the lytic phase a blade of grass appearance has been described. This is more often seen in the femur and tibia (Figure 6a,b).
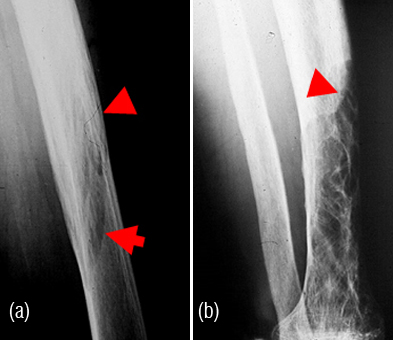
Figure 6a: Paget femoral shaft - “Blade of Grass Appearance”. (b) Paget tibia - “Blade of Grass Appearance” with an expanded bon.
The short bones of the hands and feet may be involved in all the phases (Figure 7).

Figure 7: Paget calcaneum with sclerosis.
The unusual features of Paget of bone include involvement of mid shaft of femur, tibia and humerus (Figure 8).

Figure 8: Paget involving tibial mid shaft – rare manifestations.
Fibula is rarely involved (Figure 9).

Figure 9: Paget fibula, an uncommon site.
Soft tissue involvement is known. Ankylosis of spine and sacroiliac joints has been descried. When the patient is immobilized the lytic phase of Paget is exaggerated and may advance.
In the differential diagnosis of monostotic Paget only involving the vertebral body may include round cell tumors, metastasis and myeloma. Other benign lesions such as sclerotic hemangioma, tuberous sclerosis and infections may be considered. In the differential diagnosis of polyostotic Paget include metastases, myeloma, lymphoma, hyperphostphatasia, mastocytosis, fluorosis and fibrous dysplasia.
Complications include soft tissue involvement (Figure 10a). Other complications include crystal deposition disease in cartilages, degenerative joint disease, deformities, ankylosis and neoplastic transformation (Figure 10b). Neoplasms such as cementoma, giant cell tumors, osteosarcoma, fibrosarcoma, malignant fibrous histiocytoma and chondrosarcoma in Paget disease have been reported (Figure 11a,b). Giant cell tumors are more common in the facial bones affected with Paget.
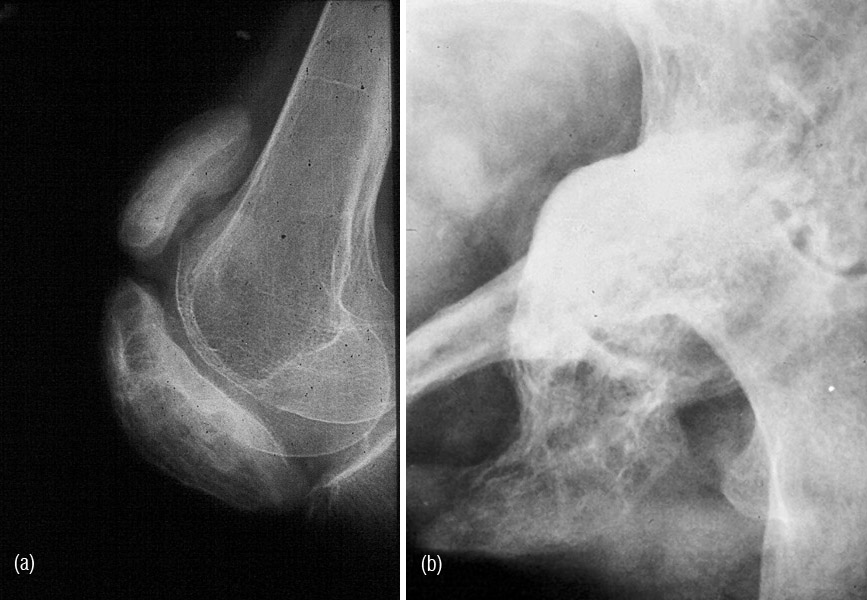
Figure 10: (a) Paget Patella with old avulsion injury with Pagetoid changes in the quadriceps tendon. (b) Paget iliac bone with protrusio acetabuli and degenerative changes in hip joint.
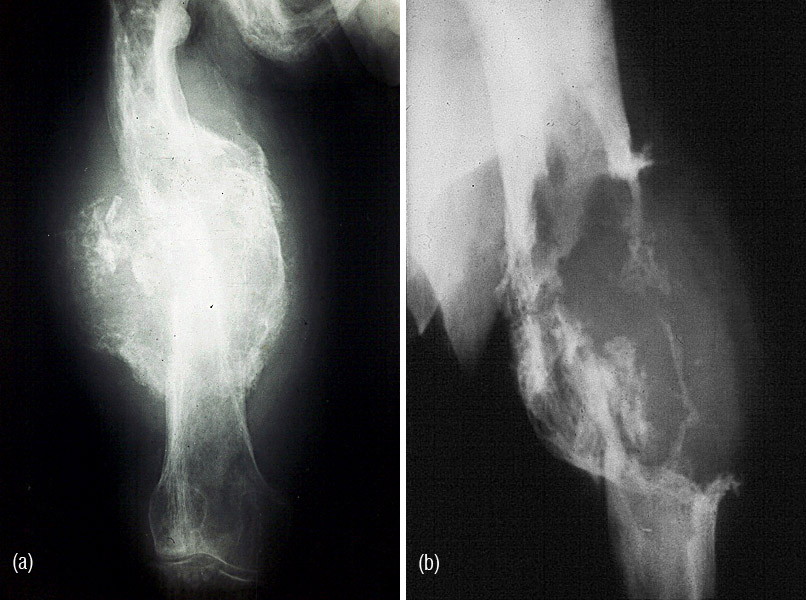
Figure 11a,b: Secondary osteosarcoma in Paget of femur.
Metastsis and myeloma may be associated with Paget. Fractures are typically of banana type. Stress fractures occur as well as increment fractures (Figure 12a,b).
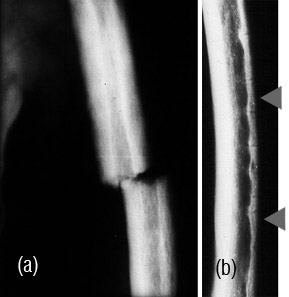
Figue 12: (a) Paget femur with banana type of fracture. (b) Paget femur with increment fractures.
Avulsion injuries of the musculoskeletal junctions are not uncommon. Compression fractures of the vertebral bodies may produce neurological symptoms (Figure 13ab).
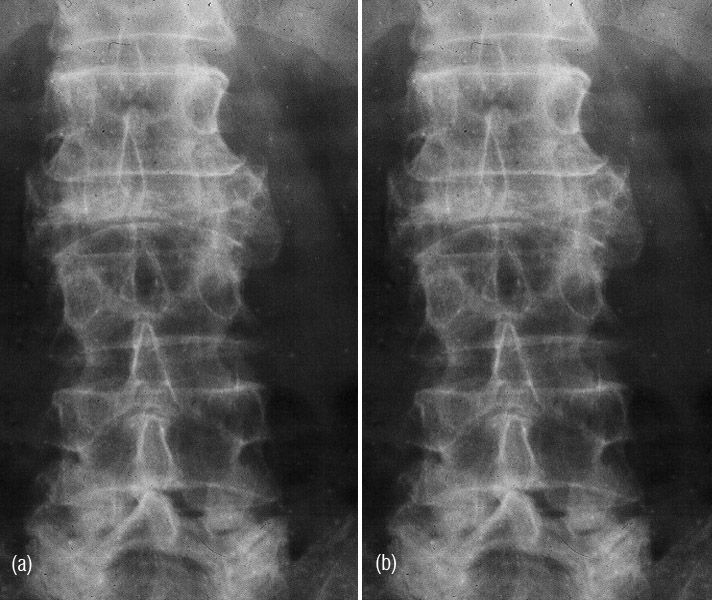
Figure 13a,b: Paget spine with compression fracture - wafer vertebra.
Non osseous complications include extramedullary hemopoiesis, congestive heart failure and enlarged kidneys. Cranial nerves and spinal cord may be involved.
CT may show cross sectional imaging of the bone (Figure 14ab).
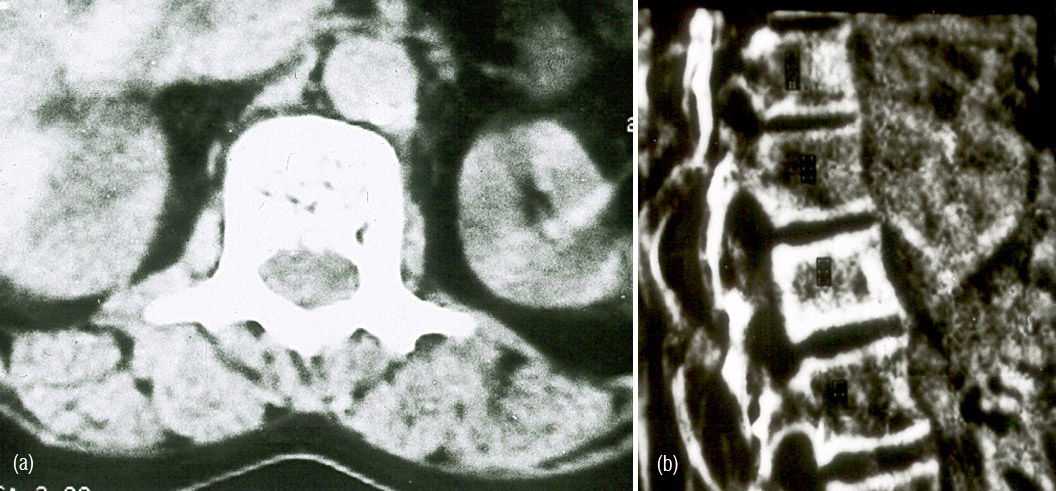
Figure 14a,b: Paget spine - C.T. Scan unnecessary: not very helpful.
In addition, it will show soft tissue changes as well as early calcifications. CT myelogram may show changes in the spinal cord.
MRI in Paget of bone is unnecessary except when the vertebral column is involved, as it may show compression of the spinal cord. MRI findings include marrow fat preservation, decreased signal intensity on short TR/TE and increased signal intensity on long TR/TE. The cortical and trabecular thickening with bowing of the bones as seen in MRI, may indicate early fractures of insufficiency fractures (Figure 15).
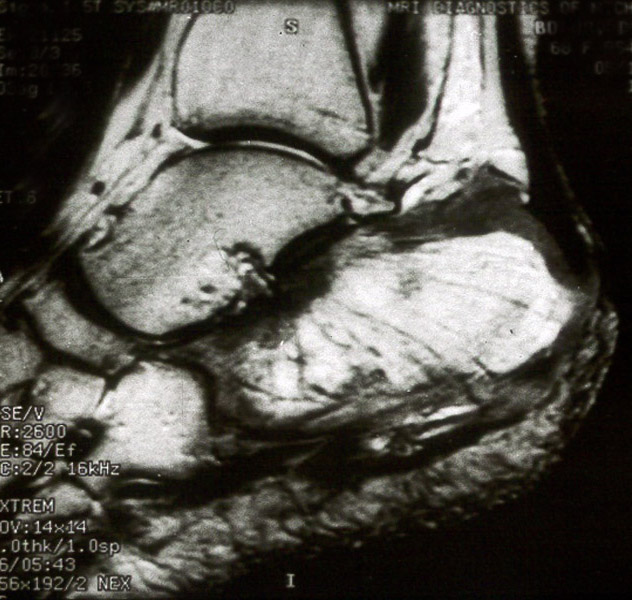
Figure 15: MRI - Paget calcaneum CT may not have much role except to study early calcifications, fractures and early malignancy.
Radionuclide bone scanning is quite useful in knowing the metabolic activity and identifying the number of bones involved. The mechanism involves chemical adsorption, increased vascularity, modeling of bone and bone turn over.
The scan findings include intense uptake and diffuse involvement. Anatomical land marks, expansion of bone, deformity are identified. The scan shows clear cut margins and extension to the end of long bones. The intense activity along the ilio pectineal line differentiates Paget from other processes (Figure 16a,b,c).
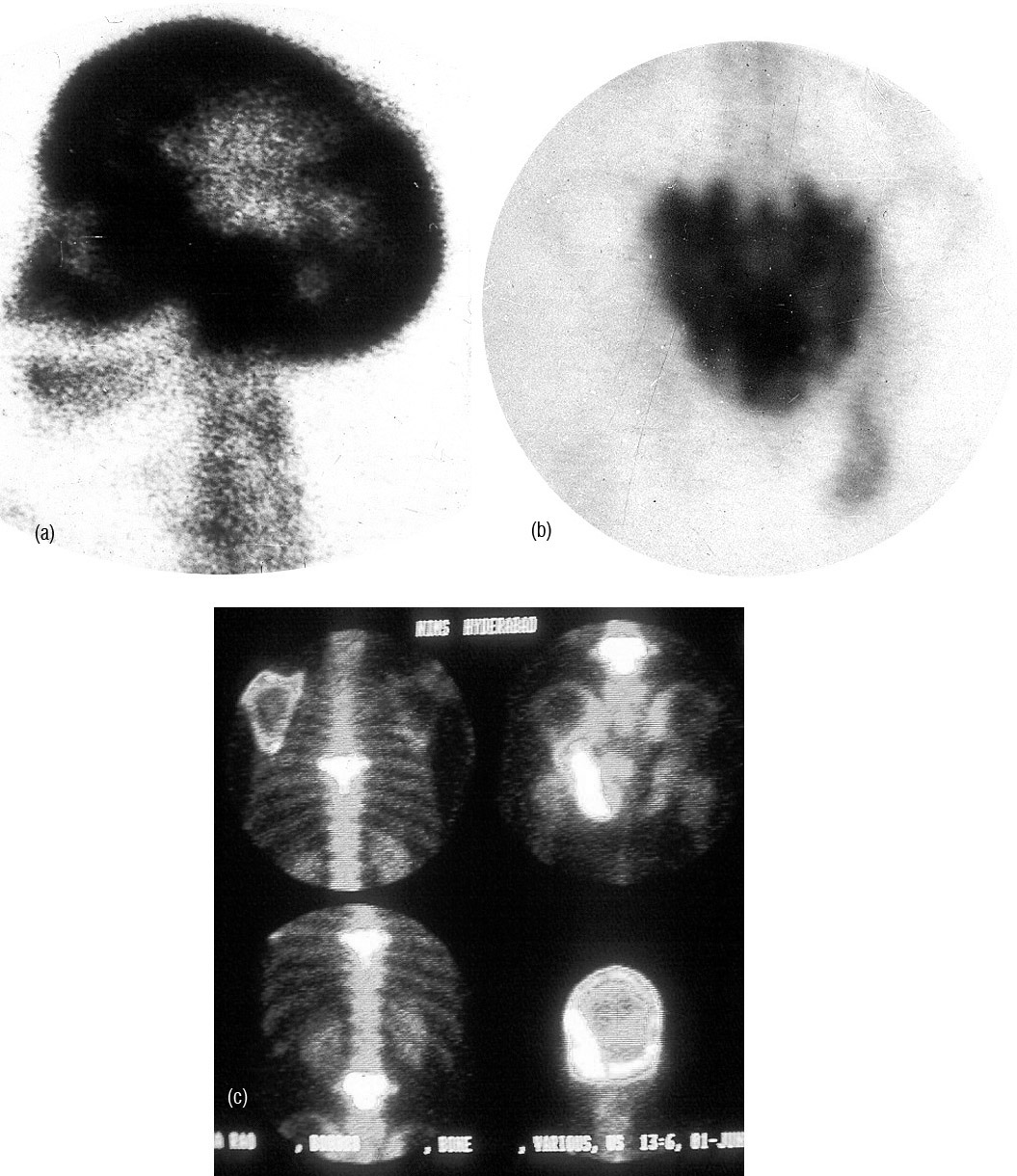
Figure 16: (a) Technetium 99 isotope scan in Paget skull. (b) Technetium whole body scan in Paget showing the polyostotic nature. The appearance at iliopectenial line is characteristic. (c) Technetium 99 scan showing Paget involving sacrum and left acetabulum.
Acknowledgements are due to managements of Osmania General Hospital, Hyderabad and Nizam’s Institute of Medical Sciences, Hyderabad.
Conclusion
Paget disease is rare in India (you see what you know!). It may involve any part of the skeleton from head to toe. Conventional Radiology is the best mode of investigation. Radiological features and complications are universal inpatients of any country. Look alikes such as lesions of fibrous dysplasia may mislead one unless careful studies are made. Bone scanning is the final word to find out whether one is dealing with monostotic or polyostotic disease. The exact etiology of Paget is still unknown, although a virus theory has been proposed since inclusion bodies are identified in Giant cell tumors of Paget bone. Complications include deformities, fractures, joint disease and malignant transformation.
Conflicts of interest
Author declares no conflicts of interest.
References
1. Bharadwaj OP. Monostotic Paget’s Disease of Bone. J Ind Med Assn. 1964; 43:341-342.
2. Donaldson JR, Bond WM et al. Paget’s Disease of Bone. Ind Journal of Surgery. 1969; 31:301-303
3. Gupta BB, Lamba GS, et al. Paget’s Disease of Bone. Ind Jour Radio. 1974; 28:131.
4. Kaufman GA, Sundaram M, McDonald DJ. Magnetic resonance imaging in symptomatic Paget’s disease. Skeletal Radiol. 1991; 20:413-418.
5. Krishna Murthy K, Mansharamani GG, et al. Paget Disease (Case report). Ind Jour. Med Sc. 1972; 26:739.
6. Kundu J. Monostotic Paget Disease of Tibia, IJRI. 1985; 39: 121-122.
7. Mohan V. Paget’s Disease of Bone in india (edi.), The Clinician. 1980; 44:1.
8. Pant HC, Sharma SP et al. Osteogenic sarcoma (Paget’s), Indian Medical Gazette Vol. C XII, 1978; 193 – 194.
9. Ramamurthi, Viswanathan et al. Paget’s of Axis of Vertebra. 1957
10. Ranga Chari P et al. Paget’s Disease of Bone. Ind Jour Ortho. 1975; 9:35.
11. Resnick D. Diagnosis of bone and joint disorders (3rd ed.) Vol. 4. Philadelphia, Pa: Saunders. 1995; 1396.
12. Schajowicz F, Santini Araujo E, Bernstein M. Sarcoma complicating Paget’s disease of bone: a clinicopathological study of 62 cases. Bone and Joint Surg Br 1983; 65:299-307.
13. Shah HR, Patwa PC, et al. Paget’s Disease of Calcaneum (Letter to Editor), IJRI. 1994; 4:3: 179-180.
14. Shanmuga Sundaram TK. Paget’s Disease. Ind J Ortho. 1970; pp.85.
15. Siris ED, et al. Paget’s disease of bone. In: Favus MJ, eds. Primer on metabolic bone diseases and disorders of mineral metabolism (3rd ed.). Philadelphia, Pa: Lippincot.
16. Stacy E. Smith et al. Radiologic Spectrum of Paget Disease of Bone and Its Complications with Pathologic Correlation from the Archives of the AFIP. Radiographics. 2002; 22:1191-1216.
17. Subbarao Kakarla, Paget Disease, CME Proceedings, Medwin Hospitals, 1994; pp.65-63.
18. Subramanian MV, Subbarao K et al. Paget’s Disease of Bone. Ind Journal of Radiology 1972; 26:63.
19. Virender Mohan, Gupta SK et al. Paget’s Disease of Done. IJRI. 1986; 40:39-43.
20. Vyagreswarudu C, Paget’s Disease: a case report. Ind Jour Surg. 1953; 15:239.