Case Report
2020
June
Volume : 8
Issue : 2
Papillary carcinoma thyroid presenting as hemoptysis
Subhramanyam C, Padiki S, Parvataneni N, Satishrao I
Pdf Page Numbers :- 82-85
Subhramanyam C1,*, Snehalatha Padiki1, Nagendra Parvataneni2, and Satish Rao I3
1Department of Otorhinolaryngology, Krishna Institute of Medical Sciences, Secunderabad-500003, Telangana, India
2Department of Surgical Oncology, Krishna Institute of Medical Sciences, Secunderabad-500003, Telangana, India
3Department of Pathology, Krishna Institute of Medical Sciences, Secunderabad-500003, Telangana, India
*Corresponding author: Dr. C. Subhramanyam, MS., ENT (PGI, Chandigarh), Consultant surgeon, Department of Oto Rhino Laryngology, Krishna Institute of Medical Sciences (KIMS), Secunderabad-500003, Telangana, India. Email: drcsubrahmanyam@gmail.com
Received 13 December 2019; Revised 6 March 2020; Accepted 21 March 2020; Published 30 March 2020
Citation: Subhramanyam C, Padiki S, Parvataneni N, Satishrao I. Papillary carcinoma thyroid presenting as hemoptysis. J Med Sci Res. 2020; 8(2):82-85. DOI: http://dx.doi.org/10.17727/JMSR.2020/8-11
Copyright: © 2020 Subhramanyam C et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Papillary carcinoma (PCT) is a common thyroid malignancy all over the world. It is commonly seen in elderly females in 5th, 6th decades. The usual presentation is painless mass in the anterior neck. Patient may have the pressure symptoms like difficulty in swallowing, hoarseness of voice, if the mass is large. Patients with metastatic deposit may manifest with headache and backache. Huge swellings with compression over trachea may cause stridor also. We report a case of elderly female presenting with occasional history of hemoptysis since one year. Computerized tomographic scan revealed a mass in the thyroid region with invasion into the trachea. USG guided fine needle aspiration cytology reported as papillary carcinoma. Fiber optic bronchoscopy confirmed the tracheal invasion.
Keywords: Papillary carcinoma thyroid; CT; invasion; hemoptysis
Full Text
Introduction
A thyroid tumour usually presents as a slow growing painless anterior neck mass. The readily appreciated presence of the mass in the neck usually makes the patient present early for medical attention. Not uncommonly, lymph node metastasis can be the sole presentation. But more commonly it occurs together with the thyroid mass. Without these symptoms, thyroid pathology is usually not suspected. Haemoptysis in PCT is a misleading presentation. It is a rare but important symptom of thyroid cancer [1].
Case summary
A 60-years-old female patient presented with occasional history of haemoptysis since one year initially very small in quantity. Later she had two episodes of significant amount and was managed with some medication by local physician. She presented to our department with another episode of haemoptysis. There was no history of hoarseness of voice, shortness of breath, dysphagia. She was not a known hypertensive and not on any blood thinners.
Clinical examination revealed no external abnormality, no visible neck mass or dilated veins. Laryngoscopy with 70-degree scope showed normal laryngeal inlet. There was no obvious mass lesion visible (Figure 1).
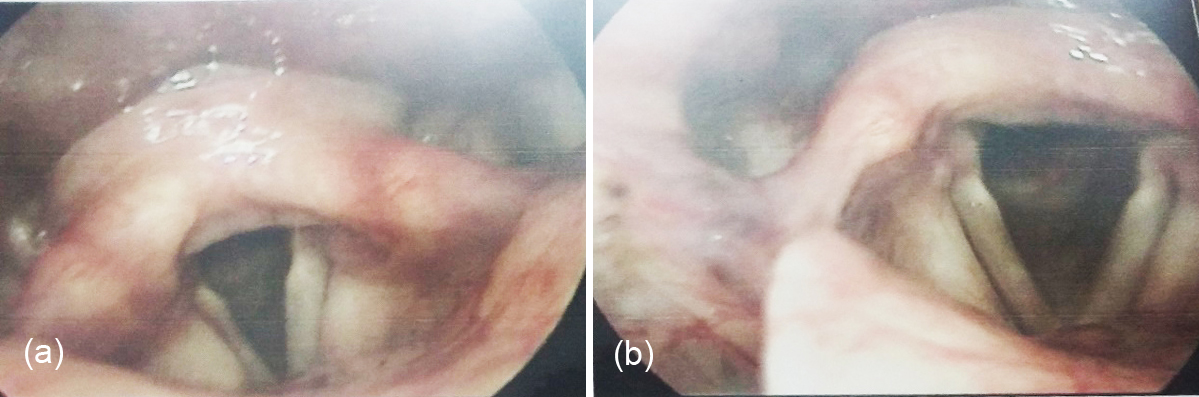
Figure 1a, b: Laryngoscopy- normal, mobile vocal cords.
Contrast enhanced tomographic scan of neck and thorax was done which revealed moderately enhancing soft tissue density lesion measuring 1.5×1.2 cm seen to arise from the anterior wall of proximal trachea extending into its lumen causing moderate luminal occlusion (Figure 2). Anteriorly there is an exophytic component in the left thyroid lobe with loss of fat planes measuring approximately 1.8×1.0 cm. It is seen eroding the tracheal ring. Rest of the trachea and bronchi are normal.
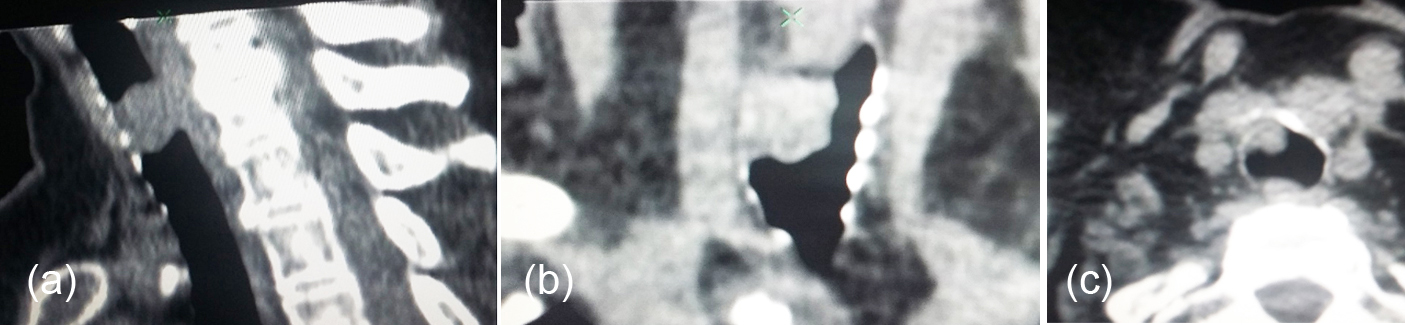
Figure 2: (a) CT scan showing the growth in the trachea, (b) Coronal view showing the mass eroding the anterior wall of the proximal trachea (c) Axial view CT neck shows mass within the lumen.
Ultrasound guided fine needle aspiration cytology was done from lesion projecting from the anterior wall into the lumen in proximal trachea, under all aseptic precautions under local anaesthesia. Cytopathlogical features suggestive of papillary carcinoma thyroid Bethesda category.
The 18F FDG positron emission tomographic scan with Intravenous contrast (ultravist) and diluted oral contrast showed an intense FDG uptake and revealed hyper-metabolic well defined enhancing lesion in left lobe of thyroid. Small volume bilateral level 2 cervical lymph nodes with minimal activity were seen. There were no metastatic deposits elsewhere.
Fibre-optic bronchoscopy revealed intra tracheal growth below the vocal cords with near total luminal obstruction (Figure 3).
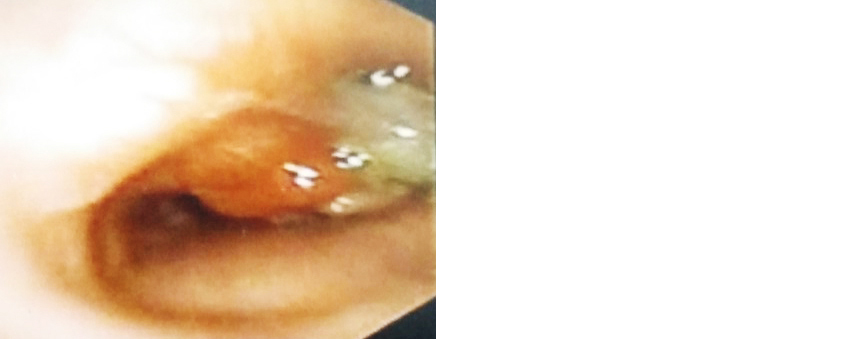
Figure 3: Smooth fleshy mass in the trachea anterior wall seen with slough- near total occlusion.
Patient and attenders were counselled for surgery-total thyroidectomy with regional nodal clearance with tracheotomy with excision of intra tracheal growth and tracheal end to end anastomosis (Figure 4). This was followed by post-operative radio iodine therapy. The total treatment was uneventfully.
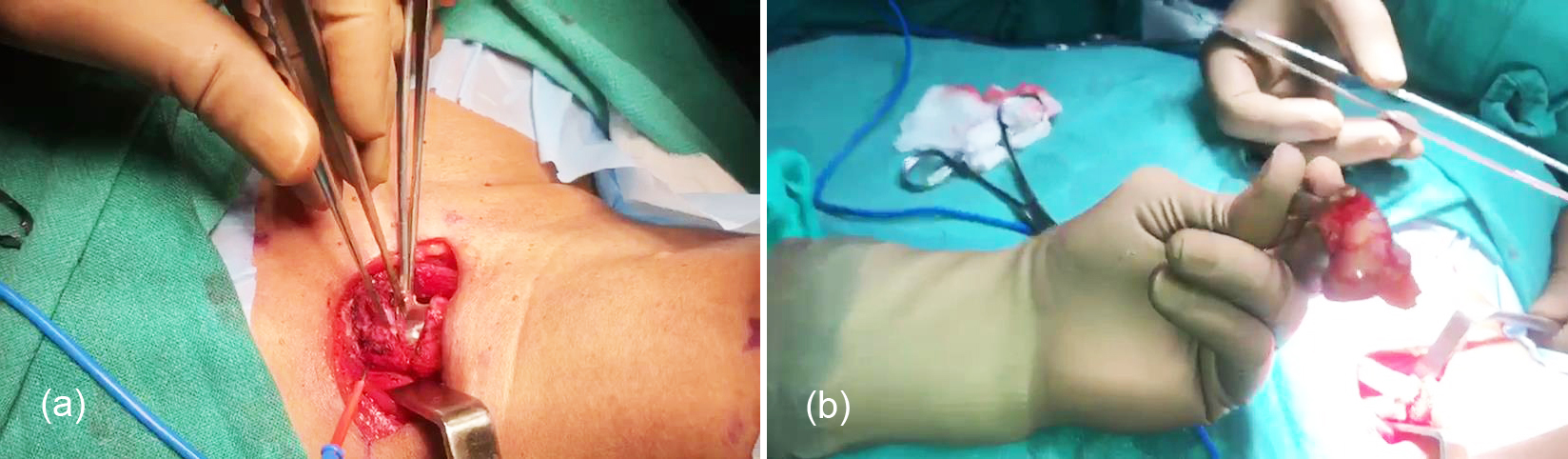
Figure 4: Thyroidectomy (a) Tracheal tumour delineation, (b) Tumour excised.
Post operatively patient had retained her voice. Histopathological examination of the specimen confirmed the diagnosis (Figure 5).

Figure 5a, b: Histopathological examination of the specimen confirmed the diagnosis.
Discussion
Papillary thyroid carcinoma (PTC) is the commonest form of thyroid malignancy. It accounts for 88% of all thyroid tumours [2]. The follicular variant accounts for 9% and poorly differentiated 3%. The female to male ratio was 5.7:1. In some patients we can see mixed papillary- follicular patterns also [3].
PCT carries a good prognosis. Common presentation includes a painless neck mass in the anterior neck with normal overlying skin [4]. PCT presenting as Haemoptysis (like in our case), a fungating mass on the skin, airway symptoms with normal external neck appearance is extremely rare [5].
PCT is characterised by slow growth, frequently indolent clinical course, with a 10-year survival rate of over 80% [6]. Approximately 40% of PCT are metastatic to local lymph nodes at the time of presentation. Pulmonary metastasis is relatively rare. Less than 1% reported in four cases of PCT that was stable clinically for longer periods (14 to 25 years) after the diagnosis of pulmonary metastasis [7]. A report that ablation of 131 Iodine uptake with therapeutic use of radio iodine was associated with higher survival rate than those in the uptake was not ablated. Pulmonary metastasis from PCT has been shown to regress following 131I (Iodine 131) treatment [8].
Direct invasion of the tumour to the tracheal wall can easily affect the recurrent laryngeal nerve which is located in the trachea oesophageal groove (Table 1). Further deeper extension in to the tracheal lumen will produce space- occupying lesion effecting the airway which includes shortness of breath, noisy breathing. Ulceration of the tumour either because of vascularity of the tumour or because of high pressure cough reflex can result in haemoptysis [9].
Table 1: Shin’s staging of tracheal invasion.
|
Stage 0 - When there is no ETE.
Stage I - For extra thyroidal disease abutting the airway.
Stage II - When invasion of the cartilage rings is present.
Stage III - When disease invades the submucosa of the trachea.
Stage IV - When disease involves the mucosa of the trachea.
|
Conclusion
The treatment of an operable PCT is surgery followed by radio iodine ablation. If tracheal invasion is present, the treatment must include tracheal resection and end to end anastomosis. If the tracheal invasion is limited with no involvement of mucosal surface, then tracheal shaving can be recommended. Palliative treatment can be considered if the patient is aged, any comorbidities and the stage is advanced. We have presented an unusual clinical variant of PCT with haemoptysis as the presenting manifestation. The exact reason for the haemoptysis was not established, but it can be due to pulmonary arterio venous fistula in metastatic carcinoma or maybe due to ulceration of tracheal lesion
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] McCaffrey TV, Lipton RJ. Thyroid carcinoma invading the upper aerodigestive system. The Laryngoscope, 1990; 100(8):824–830.
[2] Cody HS, Shah JP. Locally invasive, well-differentiated thyroid cancer. 22 years' experience at Memorial Sloan-Kettering Cancer Center. Am J Surg. 1981; 142(4):480–483.
[3] Ortiz S, Rodríguez JM, Soria T, Pérez-Flores D, Piñero A, et al. Extrathyroid spread in papillary carcinoma of the thyroid: clinicopathological and prognostic study. Otolaryngol Head Neck Surg. 2001; 124(3):261–265.
[4] Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM. AJCC Cancer Staging Manual – Thyroid. New York, Springer, 2002; pp. 77–87.
[5] Shin DH, Mark EJ, Suen HC, Grillo HC. Pathologic staging of papillary carcinoma of the thyroid with airway invasion based on the anatomic manner of extension to the trachea: a clinicopathologic study based on 22 patients who underwent thyroidectomy and airway resection. Hum Pathol. 1993; 24(8):866–870.
[6] Sobin LH, Wittekind Ch. TNM Classification of Malignant Tumours. New York: Wiley-Liss, Inc., 2002.
[7] Gaissert HA, Honings J, Grillo HC, Donahue DM, Wain JC, et al. Segmental laryngotracheal and tracheal resection for invasive thyroid carcinoma. Ann Thorac Surg. 2007; 83(6):1952–1959.
[8] Djalilian M, Beahrs OH, Devine KD, Weiland LH, DeSanto LW. Intraluminal involvement of the larynx and trachea by thyroid cancer. Am J Surg. 1974; 128(4):500–504.
[9] Mellière DJ, Yahia NEB, Becquemin JP, Lange F, Boulahdour H. Thyroid carcinoma with tracheal or esophageal involvement: limited or maximal surgery? Surgery. 1993; 113(2):166–172.