Case Report
2021
June
Volume : 9
Issue : 2
Unusual presentations of ‘‘left ventricular non compaction’’- A rare form of cardiomyopathy
Maheen S, Srikala MJ
Pdf Page Numbers :- 119-124
Sania Maheen1,* and Jwala Srikala M1
1Department of Radiology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India
*Corresponding author: Sania Maheen, Department of Radiology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India. Email: sania.maheen1992@gmail.com
Received 2 December 2020; Revised 15 February 2021; Accepted 29 February 2021; Published 9 March 2021
Citation: Maheen S, Srikala MJ. Unusual presentations of ‘‘left ventricular non compaction’’- A rare form of cardiomyopathy. J Med Sci Res. 2021; 9(2):119-124. DOI: http://dx.doi.org/10.17727/JMSR.2021/9-18
Copyright: © 2021 Maheen S et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Left ventricular non-compaction is an overall rare form of non-ischemic cardiomyopathy. The true prevalence of left ventricular non compaction (LVNC) is unclear, but it has been reported in 0.014–0.05% of adults and even less in paediatric population [1]. We present the case series of the patients who presented with varied clinical presentation and diagnosed to have left ventricular non-compaction on imaging. We have reviewed the literature regarding diagnostic imaging criteria and imaging pitfalls of this condition.
Keywords: left ventricular non compaction; cardiac MRI; non ischemic cardiomyopathy; late gadolinium enhancement
Full Text
Case report
Case 1
57-years-old male presented with sudden onset of shortness of breath. transesophageal echocardiography (TEE) revealed dilated left atrial (LA)/ left ventricular (LV), regional wall motion abnormalities (RWMA) in coronary artery disease (CAD) and left circumflex artery (LCX) territory. Coronary angiography (CAG) revealed triple vessel disease and was advised cardiac MRI for viability assessment. Cardiac magnetic resonance (MR) revealed thickened myocardium of left ventricle with increased trabeculations and deep intertrabecular recess. The non-compacted trabeculated myocardium measured 1.74cms and compacted myocardium measured 8mm in thickness with ratio of non-compacted to compacted myocardium (>2:1) in the end diastole consistent with left ventricular non compaction (LVNC). On post contrast study, transmural late gadolinium enhancement noted along the left anterior descending (LAD) and LCX territory suggesting non-viable myocardium (Figure 1). Ejection fraction - 34.5%.
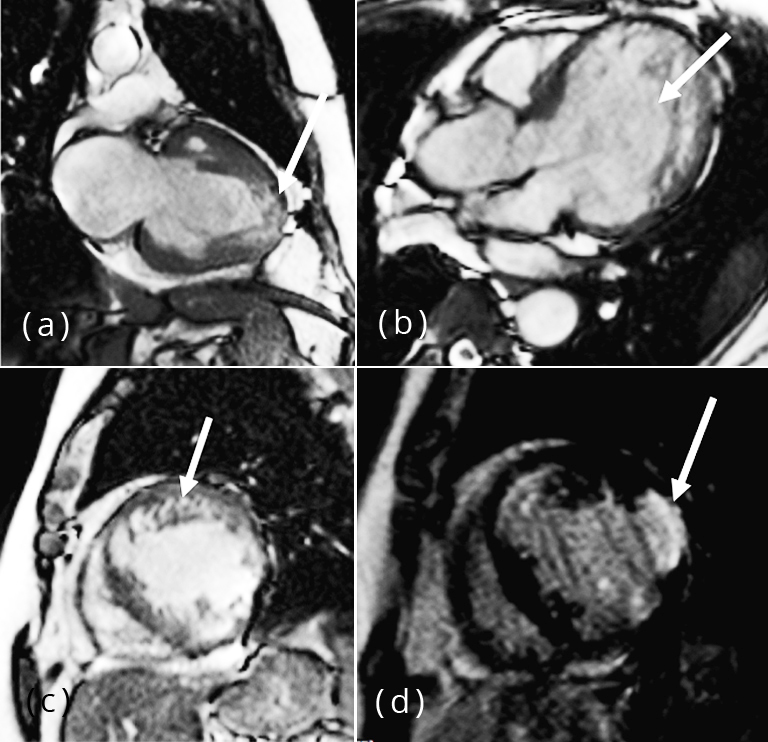
Figure 1: (a) Two chamber long axis SSFP image showing left atrium and left ventricle. Note the presence of non-compacted heavily trabeculated myocardium in the apex (arrow) and extending into mid cavity, (b) Four chamber SSFP image showing deep intertrabecular recess (arrow) communicating with LV cavity, (c) Short axis view shows trabeculated myocardium, (d) Short axis two chamber post contrast PSIR image shows transmural late gadolinium enhancement (arrow) representing non viable myocardium involving LCX territory.
Case 2
67-years-old male presented with low back ache with lumbar disc herniation. Pre-operative TEE revealed RWMA in LAD territory with apical non compaction. Cardiac MRI was done to confirm the diagnosis of non compaction. Cardiovascular magnetic resonance (CMR) of this patient showed hyper trabeculated left ventricular myocardium along the anterolateral and lateral wall with thinned out compacted myocardium. Noncompacted to compacted ratio was 2:3 (Figure 2). Ejection fraction- 37.7%.
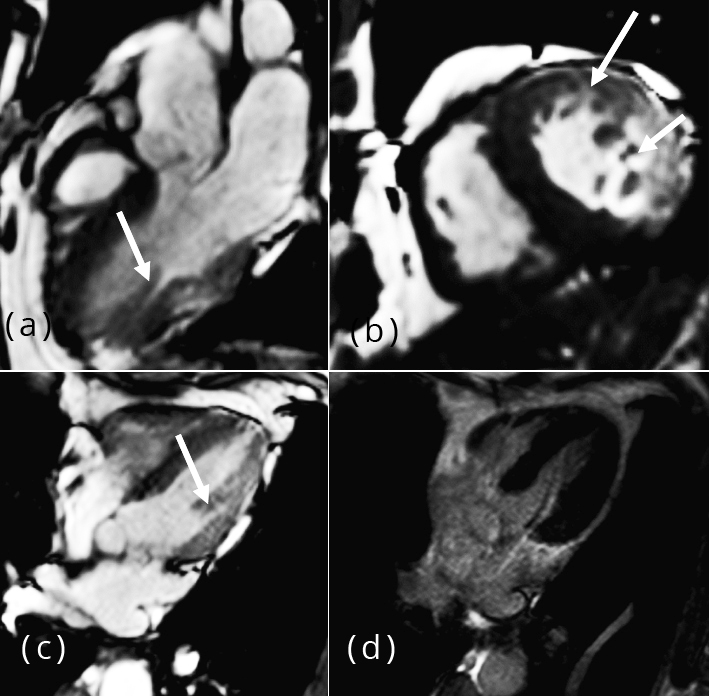
Figure 2: (a) Two chamber long axis SSFP image showing trabeculated myocardium (arrow) involving lateral wall of LV, (b) Two chamber short axis image showing trabeculated myocardium along the anterolateral and lateral wall, (c) Four chamber short axis SSFP image showing deep intertrabecular recess (arrow), (d) Four chamber short axis post contrast PSIR image reveals no abnormal areas of enhancement.
Case 3
31-years-old male presented with sudden onset of shortness of breath with global hypokinesia and severe LV dysfunction on TEE. Cardiac markers were negative. Cardiac MRI was advised to rule out myocarditis. CMR findings included dilated left atrium and ventricle with global hypokinesia. LV showed thickened and trabeculated myocardium involving apex, mid cavity with non-compaction to compacted myocardial ratio 3:1 at apex. On post contrast, there were no areas of abnormal late gadolinium enhancement. Ejection fraction -21.8%.
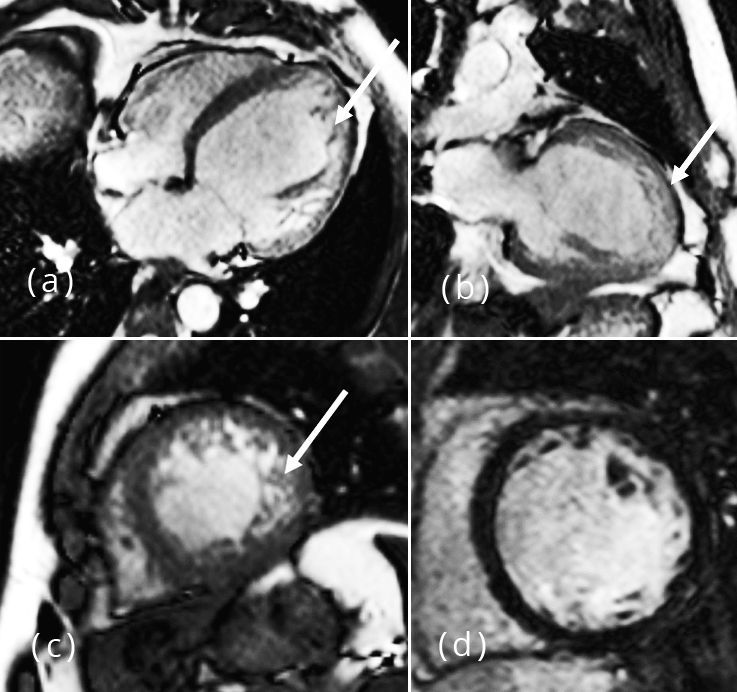
Figure 3: (a-c) Four chamber short axis, two chamber long axis and two chamber short axis SSFP images showing dilated left ventricle with hypertrabeculated myocardium of left ventricle (arrows). (d) Post contrast PSIR image show no abnormal areas of enhancement.
Discussion
LVNC is a relatively rare entity characterized by prominent left ventricular trabeculae, deep intertrabecular recesses, and thin compacted layer [2]. Two patterns have been recognised. Isolated LVNC occurs in the absence of other cardiac anomalies. In non-isolated LVNC, noncompaction is associated with the congenital heart diseases.
All of our cases belong to isolated category with no congenital heart diseases [3]. In our case series, cardiac MRI was superior in diagnosing and assessing the extent of non-compaction. Cardiac MR of our patients showed noncompacted to compacted myocardial thickness ratio of > 2.3 at end diastole. This ratio is 99% specific for LVNC and confirms the diagnosis of LVNC [4].
Etiology
The principal mechanism of LVNC is a defect in the normal process of myocardial morphogenesis that leads to arrest of the normal compaction process of the developing myocardium [5]. The ventricular apex is always involved because it is the last region to undergo compaction [2].
Clinical aspects
Clinical presentations are wide and nonspecific. The initial presentation may vary from no symptoms to chest pain or discomfort, heart failure, or arrhythmias [1]. Imaging The diagnosis of LVNC is based on the finding of thickened myocardium with a two layered structure consisting of a thin, compacted epicardial layer and a much thicker, non-compacted endocardial layer [6].
Echocardiography is the most frequently used first-line diagnostic tool for LVNC. However, myocardial trabeculations can be difficult to visualize with echocardiography with apical portion most frequently affected [1].
Cardiac MRI should be performed to confirm the diagnosis of LVNC and to evaluate for associated congenital heart disease. The most widely accepted MRI diagnostic criteria proposed by Petersen et al. is an end-diastolic ratio between noncompacted and compacted layers greater than 2.3 and is considered diagnostic of myocardial noncompaction [4]. In LVNC, areas of trabeculated myocardium showed delayed contrast enhancement on post contrast study due to the presence of trabecular fibrosis [7]. These fibrotic foci serve as the substrate for potentially lethal arrhythmias leading to sudden cardiac death in these patients [8]. Right ventricular involvement in LVNC is poorly studied due to difficulty in differentiating the normal RV trabeculations from the pathological trabeculations [9]. However, dilatation of the right ventricle in addition to the hypertrabeculation can be considered for the diagnosis [10].
LVNC can lead to fatal complications, such as embolic events, arrhythmias, and sudden death. These complications can be avoided with early diagnosis and timely treatment of patients at high risk [1].
Table 1: Imaging pitfalls [12].
|
The apical form of hypertrophic cardiomyopathy
|
Increased trabeculations, low systolic function, thinner rather than thicker walls favours LVNC.
|
|
Dilated cardiomyopathy
|
Misinterpreted because LV of more than 50% of patients with LVNC are dilated and have poor systolic function.
|
|
Endocardial fibroelastosis
|
Obliterative process often begin in the apex and can be mistaken for LVNC.
|
|
Abnormal chords
|
Fibromuscular structures of varying length and thickness that connect the LV free wall or papillary muscle to the ventricular septum without a relation to the mitral valve apparatus. They are predominantly located in the apical zone mimic trabeculations.
|
|
Apical thrombus
|
Misinterpreted owing to its apical position, mostly in the echocardiography.
|
Treatment
As there are no specific therapies or guidelines for LVNC, treatment is focused on management and prevention of complications. These include heart failure, sudden cardiac death, arrhythmia, and thromboembolic events. LVNC patients are at increased risk of sudden cardiac death and few studies indicate placement of Implantable cardioverter defibrillator (ICD) devices in patients with reduced ejection fraction [11].
Abbreviations
LVNC: Left ventricular non compaction; MRI: Magnetic resonance imaging; TEE: Transthoracic echocardiography; SSFP: Steady state free precession; PSIR: Phase sensitive inversion recovery; LGE: Late gadolinium enhancement; ICD: Intra cardiac defibrillator and LV: Left ventricle.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Oechslin E, Jenni R. Left ventricular non-compaction revisited: a distinct phenotype with genetic heterogeneity? Eur Heart J. 2011; 32(12):1446–14561.
[2] Weiford BC, Subbarao VD, Mulhern KM. Non-compaction of the ventricular myocardium. Circulation. 2004; 109(24):2965–2971.
[3] Ichida F. Left ventricular noncompaction. Circ J. 2009; 73(1):19–26.
[4] Petersen SE, Selvanayagam JB, Wiesmann F, Robson MD, Francis JM, et al. Left ventricular non-compaction: insights from cardiovascular magnetic resonance imaging. J Am Coll Cardiol. 2005; 46(1):101–105.
[5] Oechslin EN, Jost CHA, Rojas JR, Kaufmann PA, Jenni R. Long-term follow-up of 34 adults with isolated left ventricular noncompaction: a distinct cardiomyopathy with poor prognosis. J Am Coll Cardiol. 2000; 36(2):493–500.
[6] Zuccarino F, Vollmer I, Sanchez G, Navalla M, Pugliese F, et al. Left ventricular noncompaction: Imaging findings and diagnostic criteria. AJR Am J Roentgenol. 2015; 204(5):W519-W530.
[7] Jassal DS, Nomura CH, Neilan TG, Holmvang G, Fatima U, et al. Delayed enhancement cardiac MR imaging in noncompaction of left ventricular myocardium. J Cardiovasc Magn Reson. 2006; 8(3):489–491.
[8] Jenni R, Wyss CA, Oechslin EN, Kaufmann PA. Isolated ventricular noncompaction is associated with coronary microcirculatory dysfunction. J Am Coll Cardiol. 2002; 39(3):450–454.
[9] Yun H, Zeng M, Jin H, Yang S. Isolated noncompaction of ventricular myocardium: a magneticresonance imaging study of 11 patients. Korean J Radiol. 2011; 12(6):686–692.
[10] Fazio G, Lunetta M, Grassedonio E, Gullotti A, Ferro G, et al. Noncompaction of the right ventricle. Pediatr Cardiol. 2010; 31(4):576–578.
[11] Caliskan K, Szili-Torok T, Theuns DA, Kardos A, Geleijnse ML, et al. Indications and outcome of implantable cardioverter-defibrillators for primary and secondary prophylaxis in patients with noncompaction cardiomyopathy. J Cardiovasc Electrophysiol. 2011; 22(8):898–904.
[12] Stöllberger C, Finsterer J. Pitfalls in the diagnosis of left ventricular hypertrabeculation/non-compaction. Postgrad Med J. 2006; 82(972):679–683.
[13] Hershberger RE, Lindenfeld J, Mestroni L, Seidman CE, Taylor MR, et al. Genetic evaluation of cardiomyopathy--a Heart Failure Society of America practice guideline. J Card Fail. 2009; 15(2):83–97.