Case Report
2016
December
Volume : 4
Issue : 4
Systemic sclerosis, secondary Sjogrens syndrome with corneal oedema: A case report
Sridhar Mittanamalli
Pdf Page Numbers :- 160-163
1Department of Ophthalmology, Krishna Institute of Medical Sciences, Minister Road, Hyderabad, Telangana, India
*Corresponding author: Dr. MS. Sridhar, MD., Department of Ophthalmology, Krishna Institute of Medical Sciences, Minister road, Hyderabad, Telangana, India. Tel.: 040-44885050; Fax: 04027840980; Mobile: 91-9849744286; Email: sri.vision@yahoo.co.in
Received 01 August 2016; Revised 08 September 2016; Accepted 15 September 2016; Published 29 September 2016
Citation: Sridhar MS. Systemic sclerosis, secondary Sjogren’s syndrome with corneal oedema: A case report. J Med Sci Res. 2016; 4(4):160-163. DOI: http://dx.doi.org/10.17727/JMSR.2016/4-035
Copyright: © 2016 Sridhar MS. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: To present a case of systemic sclerosis with asymmetrical skin involvement, decreased tear production not responding to topical cyclosporine therapy and corneal edema in one eye.
Methods: An 84 years old female diagnosed with scleroderma two years ago presented with history of decreased vision in the left eye of 10 days duration.
Results: She had generalised tight skin which was more on the left side. The skin of the face including the eyelids was tight. Her best corrected visual acuity was 20/30, N6 in the right eye and in the left eye, it was 20/200. The Schirmer’s test without anaesthesia revealed a value of 3 mm in the right eye and 1 mm in the left eye. Anterior segment evaluation showed clear cornea with no guttata in the right eye. In the left eye, there was stromal oedema involving inferior half of the cornea with superficial blood vessels inferiorly. Both the corneas showed central superficial punctuate keratopathy. Anterior segment optical coherence tomography showed normal cornea in the right eye, whereas in the left eye there was hyper-reflectivity at the level of Descemet’s membrane suggestive of increased fibrosis and the corneal thickness was more.
Conclusions: Systemic sclerosis can present with asymmetrical skin involvement, decreased tear production not responding to topical cyclosporine therapy and corneal edema in one eye. Further studies are warranted to develop treatment strategies of managing corneal edema in systemic sclerosis.
Keywords: systemic sclerosis (SSc); scleroderma; secondary Sjogren’s syndrome; corneal oedema; anterior segment optical coherence tomography
Full Text
Systemic sclerosis (SSc) or Scleroderma is a chronic multi-system autoimmune disorder of unknown aetiology affecting the skin, musculoskeletal, gastrointestinal, pulmonary and renal systems [1]. Women are more frequently affected. Three principle features of the disease which are believed to occur in the following sequence in SSc: immune activation, vasculopathy and extensive fibrosis [1]. Tightness of lids, diminished tear secretion, keratoconjuntivitis sicca and conjunctival changes are commonly reported ophthalmic manifestations of this disease [2, 3].
I present a rare case of SSc who had asymmetrical skin tightness along with decreased tear secretion and corneal oedema in one eye.
Case report
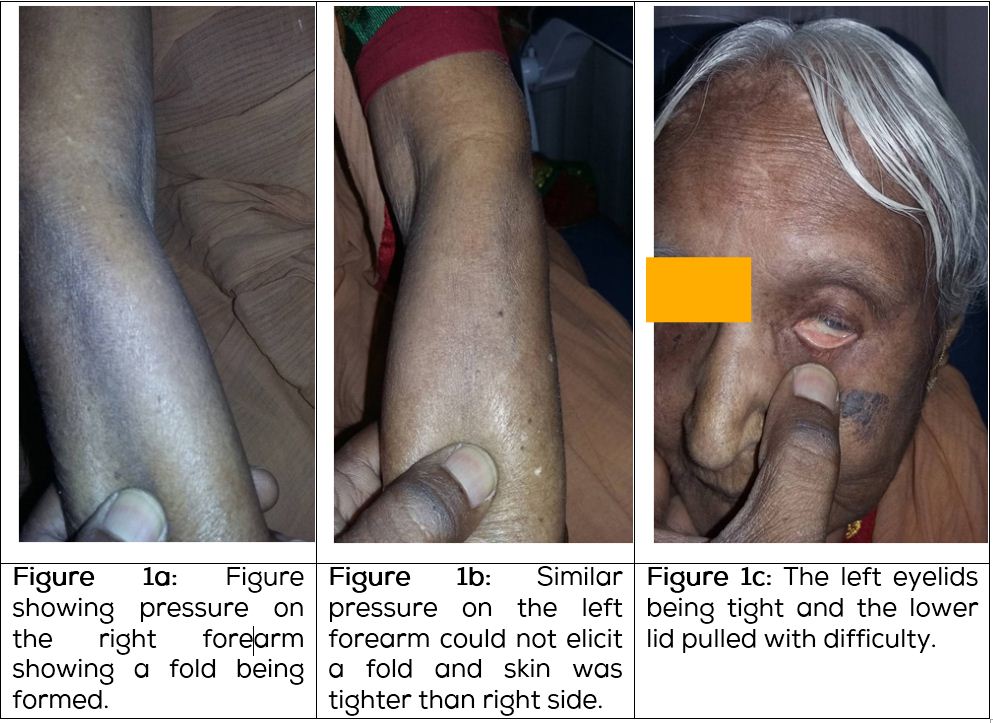
An 84-years-old female diagnosed with SSc two years ago, presented with a history of decreased vision in the left eye for the previous 10 days duration. This was associated with pain and foreign body sensation in the left eye. She gave history of grittiness of eyes. On examination, it was observed that she had generalised tight skin which was more on the left side. On the right forearm, the skin was less tight (Figure 1a) compared to the left forearm (Figure 1b). The skin of the face including the eyelids was tight. On the right side, it was relatively less tight compared to the left side. Her best corrected visual acuity was 20/30, N6 with a distance correction of +2 Ds/-3Dcyl at100 degrees, near vision was N6 with an addition of +2.5Ds in the right eye. In the left eye, the visual acuity was 20/200 which could not be improved further. The Schirmer’s test without anaesthesia revealed a value of 3 mm in the right eye and 1mm in the left eye. Anterior segment evaluation showed clear cornea with no endothelial guttata in the right eye. There was crocodile shagreen in the periphery. In the left eye, there was stromal oedema involving the inferior half of the cornea with superficial blood vessels inferiorly. The superior half of the cornea was observed to be clear with no endothelial guttata. Both the corneas showed central superficial punctate keratopathy. Both eyes were pseudophakic. Intraocular pressure was normal and the fundus examination in the right eye did not show anything remarkable.
The anterior segment optical coherence tomography (OCT) showed normal cornea in the right eye (Figure 2a), whereas in the left eye there was hyper-reflectivity at the level of Descemet’s membrane suggestive of increased fibrosis (Figure 2b) and the corneal thickness was observed to be more. Her previous blood examination had revealed strongly positivity (+++) for anti-centromere B antibody. She was started on lubricating gen teal eye drops (0.3% Hydroxy propyl methyl cellulose) along with ointment at bedtime and 0.05% Cyclosporine eye drops two times a day for both the eyes and 0.1% Flurometholone eye drops four times a day which was tapered over four weeks for the left eye. After the treatment was followed for four months, the Schirmer’s test in the right eye was 15 mm and in the left eye it was 1mm.The patient was comfortable in the left eye, yet the oedema was observed to be same.
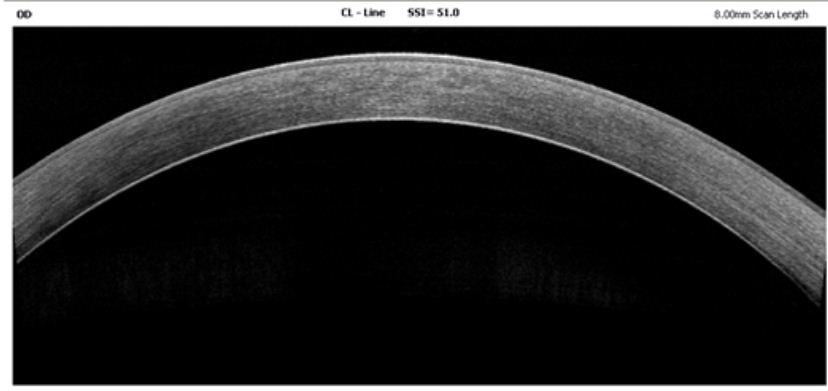
Figure 2a: Anterior segment OCT of right cornea which was normal with no edema or fibrosis.
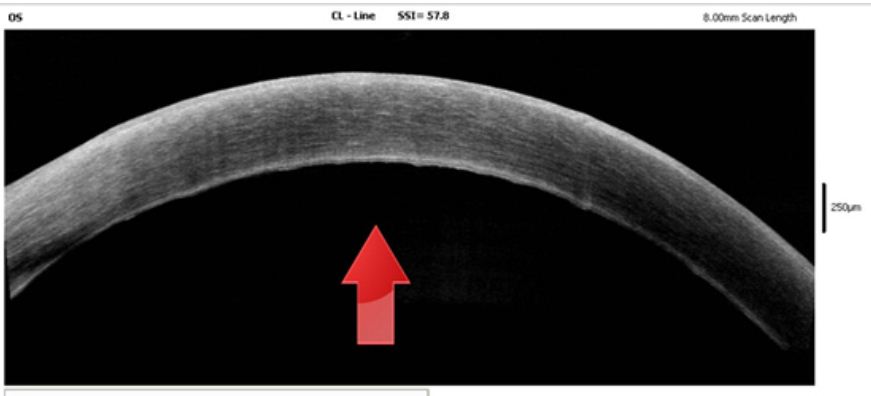
Figure 2b: Anterior segment OCT of left cornea showing fibrosis of descemet’s membrane and increase in corneal thickness.
Discussion
The various reported manifestations of SSc in eyelids include tightness of eyelids, blepharophimosis, telangiectasia, ectropion of lids and lagophthalmos. In the conjunctiva, shallow fornix, telangiectasia, conjunctival vascularization, varicosities of blood vessels, congestion, intravascular sledging and loss of fine vessels may be seen [1-3].
The most frequent ocular manifestation of SSc is keratoconjunctivitis sicca [1, 4]. Keratoconjunctivitis sicca is seen in 1/3 to 2/3 of patients and depending on the severity can present with mucous strands in pre-corneal tear film, superficial punctate keratopathy or filamentary keratitis. The presence of keratoconjunctivitis sicca in association with xerostomia (dry mouth) and a connective tissue disorder like SSc is known as secondary Sjogren’s syndrome. Salivary gland involvement appears to be more frequent than lacrimal gland involvement in patients with SSc. Inflammatory changes and prominent collagen deposition are found in minor salivary gland biopsy of patients with scleroderma [5].
Corneal involvement in SSc is a rare phenomenon. Rich collagen composition and the relation to the rich vascular supply of the conjunctiva and episclera make the cornea vulnerable to collagen vascular disease [1]. Filamentary keratitis, exposure keratitis, (secondary to lid changes) and peripheral ulcerative keratitis have all been reported to be associated with scleroderma [1, 6]. Case reports of keratoconus and pellucid marginal corneal degeneration have been reported in patients with SSc [1, 7]. Bilateral keratomalacia secondary to Vitamin A deficiency related to esophageal involvement in an SSc patient has also been reported [8]. Serup et al have shown increased central corneal thickness in patients with SSc [9]. The increased central corneal thickness with no impairment of vision during the first eight years of SSc was found by them. During the treatment period, no further increase in central corneal thickness was demonstrated by these authors.
The interesting features of our case include asymmetrical skin involvement including the eyelids skin, tear production not increasing despite topical cyclosporine A eye drops and corneal oedema involving the inferior half of the cornea in the left eye.
In SSc, when the lids are involved by the sclerodermatous process, a degree of symmetrical blepharophimosis is seen [4]. But in the case presented here, the skin tightness was observed to be asymmetrical, worse in the left side. Even the eyelids of the left eye were tight. Interestingly on topical cyclosporine-A therapy, the Schirmer’s value of the right eye improved to normal whereas, in the left eye the value remained low despite therapy for four months.
In this patient, corneal edema in the left eye was thought to be because of fibrosis of Descemet’s membrane as seen by anterior segment OCT. No endothelial gutatta were seen in the other eye and also in the superior half of the cornea in the affected eye. Cataract surgery might not be the probable cause as the edema was localized only to the inferior half of cornea.
Corneal edema in SSc has not been reported before in patients with SSc and a literature review using PubMed showed no references to this phenomenon. The other issue as shown in this case is management of corneal edema in patients with SSc. The treatment strategies currently used in patients with SSc for skin disease address mainly two aspects of SSc pathogenesis, inflammation and fibrosis. The link between the processes is evidenced by histological examination of SSc skin. Distinguishing potential immunologic or anti-inflammatory mechanisms from anti- fibrotic strategies is often difficult because of complex biologic networks interlocking these processes. Cyclophosphamide, azathioprine, mycophenolate mofetil (MMF), methotrexate, rapamycin, cyclosporine, rituximab and anti-fibrotic agents like nintedanib have been found to be useful in the treatment of established skin fibrosis [10]. Novel anti-fibrotic treatment approaches include high dose immunosuppressive therapy with stem cell transplantation, modifiers of TGF-B 1 signaling, intravenous immunoglobulins, tyrosinase kinase inhibitors and histone deacetylase inhibitors [11]. With the availability of these various modalities, management of corneal edema should be contemplated early if seen in patients with SSc. It is suggested that all patients with SSc should have serial pachometry measurement of central corneal thickness and anterior segment OCT. If the pachometry shows progressive increase in corneal thickness and anterior segment OCT reveals early fibrosis of Descemet’s membrane, early aggressive immunosuppressive therapy along with topical steroids and systemic steroids may be the needed to reduce inflammation and prevent progression of Descemet’s membrane fibrosis which may result in refractory corneal edema. In non-resolving edema, Descemet’s stripping endokeratoplasty or Descemet’s membrane endokeratoplasty may be needed for visual rehabilitation with appropriate immunosuppressive therapy.
Conclusion
To conclude, I present a case of SSc with asymmetrical skin involvement, decreased tear production not responding to topical cyclosporine therapy and corneal edema in one eye. Further studies are warranted to develop treatment strategies of managing corneal edema in SSc.
Conflicts of interest
The author declares no conflicts of interest.
References
[1] Tailor R, Gupta A, Herrick A, Kwartz J. Ocular manifestation of scleroderma. Surv Ophthalmol. 2009; 54(2):292-304.
[2] West RH, Barnett AJ. Ocular involvement in scleroderma. Br J Ophthalmol.1979; 63(12):845-847.
[3] Horan EC. Ophthalmic manifestations of progressive systemic sclerosis. Br J Ophthalmol. 1969; 53(6):388-392.
[4] Kirkham TH. Scleroderma and Sjogren’s syndrome. Br J Ophthalmol.1969; 53(2):131-133.
[5] Alarcon-Segovia D, Ibanez G, Hernandez-Ortiz J, Velázquez-Forero F, González-Jiménez Y. Sjogren’s syndrome in progressive systemic sclerosis (scleroderma). Am J Med. 1974; 57(1):78-85.
[6] Horie K, Nishi M, Sawa M, Mochizuki M. A case of peripheral corneal ulcer accompanied by progressive systemic sclerosis. Nippon Ganka Gakkai Zasshi. 1992; 96(7):922-929.
[7] Sii F, Lee GA, Sanfilippo P, Stephenson DC. Pellucid marginal degeneration and scleroderma. Clin Exp Optom. 2004; 87(3):180-184.
[8] al-Husainy S, Deane J. Bilateral keratomalacia in a cachetic scleroderma patient. Eye. 1999; 13(Pt4):586-588.
[9] Serup L, Serup J, Hagdrup HK. Increased central cornea thickness in systemic sclerosis. Acta Ophthalmol. 1984; 62(1):69-74.
[10] Nintyanova SI, Denton CP. Current approaches to the management of early active diffuse scleroderma skin disease. Rheum Dis Clin N Am. 2008; 34(1):161-179.
[11] Distler J, Distler O. Novel treatment approaches to fibrosis in scleroderma. Rheum Dis Clin N Am. 2008; 34(1):145-159.