Case Report
2025
March
Volume : 13
Issue : 1
Acremonium infection in a patient of polytrauma
Velamuri A, Fatima R, Navya K, Eswaran SP, Madigubba S
Pdf Page Numbers :- 88-89
Abhishek Velamuri1,*, Rafath Fatima1, Navya K1, Shiva Priya Eswaran1 and Shailaja Madigubba2
1Department of Microbiology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India
2Department of Pathology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India
*Corresponding author: Dr. Velamuri Abhishek, Department of Microbiology, Krishna Institute of Medical Sciences, Minister Road, Secunderabad-500003, Telangana, India. Email: avelamuri@yahoo.com.
Received 15 November 2024; Revised 2 December 2024; Accepted 10 December 2024; Published 17 December 2024
Citation: Velamuri A, Fatima R, Navya K, Eswaran SP, Madigubba S. Acremonium infection in a patient of polytrauma. J Med Sci Res. 2025; 13(1):88-89. DOI: http://dx.doi.org/10.17727/JMSR.2024/13-15
Copyright: © 2025 Velamuri A et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Acremonium species, a potential pathogen of hyalohyphomycosis group is saprophytic and ubiquitous in nature causing superficial and deep infections in both immunocompetent and immunocompromised patients. A case report of a 39-year-old man with polytrauma and possible disseminated infection due to Acremonium species is discussed. Acremonium species can cause serious potential life threatening infections. Multidisciplinary approach and timely instituted therapy result in positive outcomes.
Keywords: Acremonium species; disseminated fungal infection; non-dermatophytic molds; opportunistic fungus; systemic infection
Full Text
Introduction
Acremonium is a fungal species which is present in the soil, air and decayed vegetation. This fungus can cause multisystem disseminated infections through hematogenous spread and is resistant to routinely used antifungals [1]. A case report of Indian male who presented with polytrauma with probable disseminated infection and the causative agent as Acremonium species is discussed.
Case presentation
A 39-year-old male, with no previous comorbidities reported to hospital with polytrauma due to road traffic accident with blunt injury to chest and penetrating injury to abdomen, bilateral lower limb weakness, bowel and bladder incontinence. He was admitted to the ICU, KIMS Hospital, Secunderabad. Chest X ray AP view suggested patchy consolidation in the right lung. Computed Tomography (CT) whole abdomen suggested patchy sub capsular non enhancing area in the IV a segment of the liver (Figure 1).
Figure 1: CT ABDOMEN suggestive of mixed echogenic lesion.
Patient had fever, malaise and his Glasgow Coma Scale (GCS) deteriorated with increased drowsiness. CT and Magnetic Resonance Imaging (MRI) brain were done which suggested a ring enhancing lesion. Pus from the right liver lobe was evacuated and was sent to microbiology for gram staining, Ziehl-Neelsen staining, modified Ziehl-Neelsen staining, 10% KOH mount, culture and sensitivity and to pathology for histopathology examination. The specimen was processed as per the standard laboratory practices.
Gram stain showed moderate pus cells. Ziehl-Neelsen stain was negative for Acid fast bacilli. Modified Ziehl-Neelsen was negative for Nocardia species. 10% KOH mount showed thin filamentous hyphae with cylindrical, one-celled conidia arising from short unbranched single phialide.
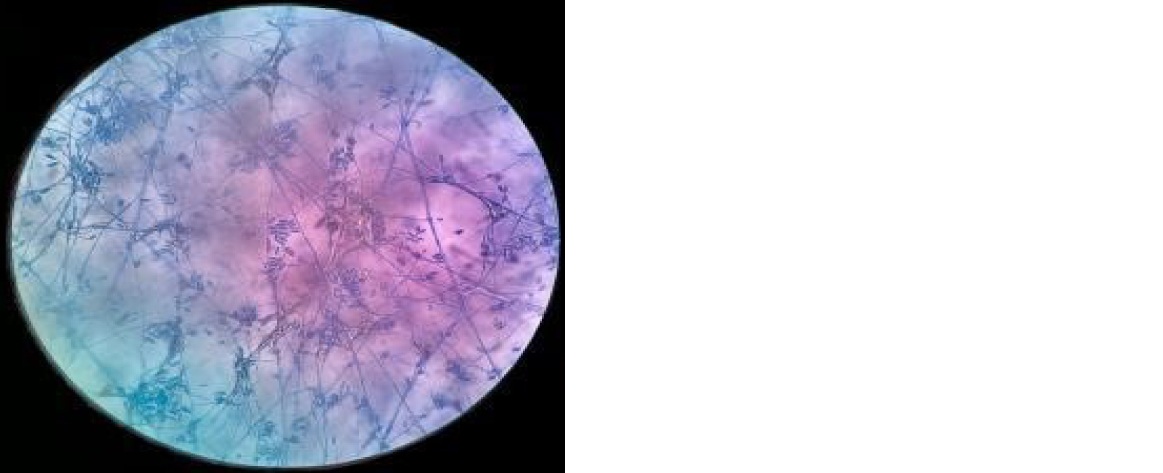
Figure 2: Photomicrograph (40x) showing septate filamentous hyphae with ellipsoidal conidia arising from short unbranched single phialide.
Under strict aseptic conditions, specimen was inoculated onto Sabouraud Dextrose Agar (SDA) with antibiotics which were incubated at room temperature and at 37°C. Gross morphology of culture after 96 hours of incubation had a white-gray with a velvety to cottony appearance on the obverse and grey-black on the reverse (Figure 3).
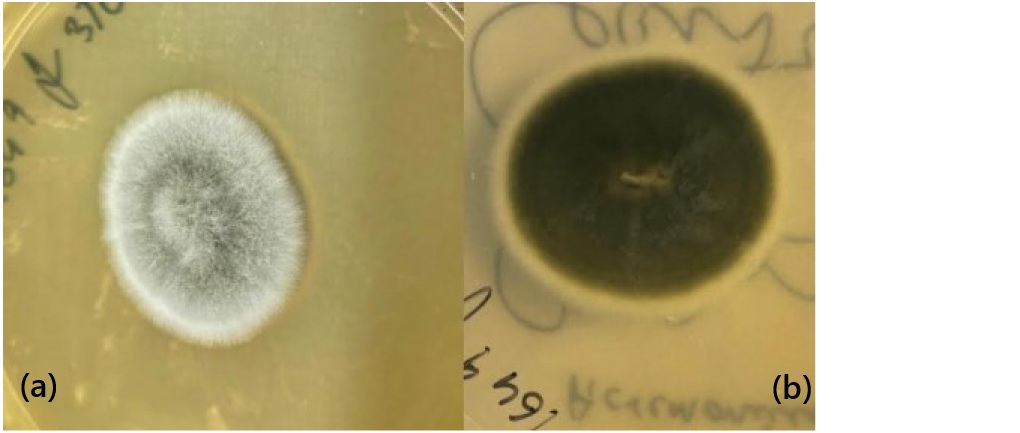
Figure 3a,b: Obverse and reverse of SDA at 37 °C.
Microscopic examination using lactophenol cotton blue (LPCB) mount revealed thin, septate, and hyaline hyphae. The conidia were single-celled, originating from short, unbranched, tapered, awl-shaped phialides and forming clusters at their apex. Macroscopic analysis showed colonies characteristic of Acremonium species, displaying a cottony, white to grayish appearance with a velvety or powdery texture, features typical of this opportunistic fungal pathogen.
Patient was initiated on IV amphotericin B 30mg once daily and voriconazole 4mg/kg for four days. His neurological status improved in due course and was discharged on oral voriconazole 200 mg twice a day for 2 months and IV amphotericin B 30mg once daily for next two months with stable hemodynamics. Patient was asymptomatic at review after two months.
Discussion
The non-dermatophytic molds (NDMs) or yeasts have a worldwide prevalence of 5.5% [1]. Acremonium, opportunistic fungus being one among them belongs to the genus cephalosporium which is a saprophytic hyaline fungal mold causing infections. Acremonium is ubiquitous in nature and an environmental contaminant. Acremonium species are being reported in both systemic and localised infections. Acremonium infections are well recognized as aetiologic agents in causing subcutaneous infections followed by penetrating trauma [2]. Majority of the reports on diseases caused by this fungus were reported from tropical and subtropical areas [3]. Acremonium can cause disseminated and multiple organ involvement causing a variety of clinical manifestations like mycetoma, mycotic keratitis, onychomycosis, arthritis, osteomyelitis, endocarditis, peritonitis and meningitis [4-7].
Conclusion
Acremonium species are opportunistic fungal pathogens capable of causing severe, life-threatening infections, especially in immunocompromised individuals, leading to high morbidity and mortality if not promptly diagnosed and treated. A multidisciplinary team, including infectious disease specialists, and microbiologists, is crucial for effective management. Timely antifungal therapy, surgical intervention when required, and vigilant monitoring significantly improve recovery outcomes and reduce complications.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Jangla SM. Onychomycosis caused by Acremonium species: A case report. Indian J Case Reports. 2024; 10:1–3.
[2] Richardson M, Lass-Flörl C. Changing epidemiology of systemic fungal infections. Clin Microbiol Infect. 2008; 4:5–24.
[3] Fincher RM, Fisher JF, Lovell RD, Newman CL, Espinel–Ingroff A, et al. Infection due to the fungus Acremonium (cephalosporium). Medicine. 1991; 70:398–409.
[4] Khan K, Qureshi S. Invasive Acremonium infection with gastrointestinal dissemination: A case report. J Infect Dis Ther. 2019; 7:395.
[5] Tuon FF, Pozzi C, Penteado–Filho SR, Benvenutti R, Contieri FL. Recurrent Acremonium infection in a kidney transplant patient treated with voriconazole: a case report. Rev Soc Bras Med Trop. 2010; 43:467–468.
[6] Neeli HV, Lakshmi N, Krishna BP. Subcutaneous hyalohyphomycosis caused by Acremonium kiliense in a diabetic: A case report. Int J Curr Microbiol Appl Sci. 2015; 4:62–65.
[7] Klimko NN, Khostelidi SN, Melekhina YE, Gornostaev DA, Semelev VN, et al. Acremonium pneumonia successfully treated in patient with acute myeloid leukemia: a case report. J Bacteriol Mycol Open Access. 2016; 2:116–119.