Full Text
Introduction
Acute mesenteric ischemia (AMI) is a major abdominal crisis, characterized by abrupt depletion in the blood inflow to the small bowel, resulting in ischemic lesions and necrosis of small bowel, if left untreated, may lead to death by peritonitis and septic shock. Clinical presentation is nonspecific in utmost cases and can be characterized by disparity between severe abdominal symptoms and no specific signs. In non-COVID cases, the etiology may be mesenteric arterial embolism (in 50), mesenteric arterial thrombosis (15–25), venous thrombosis (5–15), or lower frequent, from non-occlusive causes associated with low blood inflow [1]. Several systemic conditions, similar as atrial fibrillation, atherosclerosis, arterial hypertension, heart failure, or valve disease are risk factors for AMI.
COVID-19 is a serious respiratory disease caused by SARS-CoV-2, and the ongoing outbreak of this disease was declared a global pandemic by the World Health Organization on March, 2020. The majority of COVID-19 cases experience fairly mild complaint, some experience critical illness associated with high rates of vascular events that frequently prove fatal. Numerous COVID-19 cases have been set up to present in a largely hypercoagulable state which causes complications like venous and arterial thromboembolism. Apart from the respiratory system, the gastrointestinal system is the most common secondary site of SARS-COV-2 infection. This might be because enterocyte and vascular endothelial membranes have large numbers of angiotensin- converting enzyme receptor 2 (ACE- 2), a membrane integral protein. As a result, the COVID virus induces direct enterocyte irruption as well as indirect endothelial injury-induced thrombosis/ intestinal ischemia in the bowel [2].
The study aimed to assess relation between COVID and ischemic bowel disease by analysing length of Hospital stay and mortality rates between COVID and non-COVID groups.
Materials and methods
The study was conducted retrospectively in Seth GS Medical College and KEM Hospital, Mumbai, India. 40 patients presented to emergency room with acute abdomen which diagnosed as acute ischemic bowel disease in a period of 18 months were included from June 2020 to November 2021. Study procedures includes going through all records of patients admitted with mesenteric ischemia in that admission period i.e., Detailed history, laboratory, radiological investigations and operative notes of surgical procedures. The study included patients who willing to participate in study and above 18 years of age.
Results
COVID19 infection: Out of 40 patients, 16 patients never had history of exposure to COVID whereas 24 patients had history of exposure to COVID, 4 patients had active infection and remaining 20 had past history of COVID as shown in Table 1.
Table 1: Gender distribution.
|
COVID infection
|
Male
|
Female
|
Total
|
|
No infection
|
10
|
6
|
16
|
|
Past infection
|
13
|
7
|
20
|
|
Active infection
|
2
|
2
|
4
|
|
Total
|
25
|
15
|
40
|
Demographics: Median age was 54 years (34–79) in non-COVID patients and 57 years (31-75) in COVID patients (active + past). In both COVID and non-COVID population, distribution of comorbidities were almost equal exception being stroke, where both the cases had previous history of COVID. Diabetes was the most common comorbidity in both the groups followed by hypertension as shown in Figure 1.
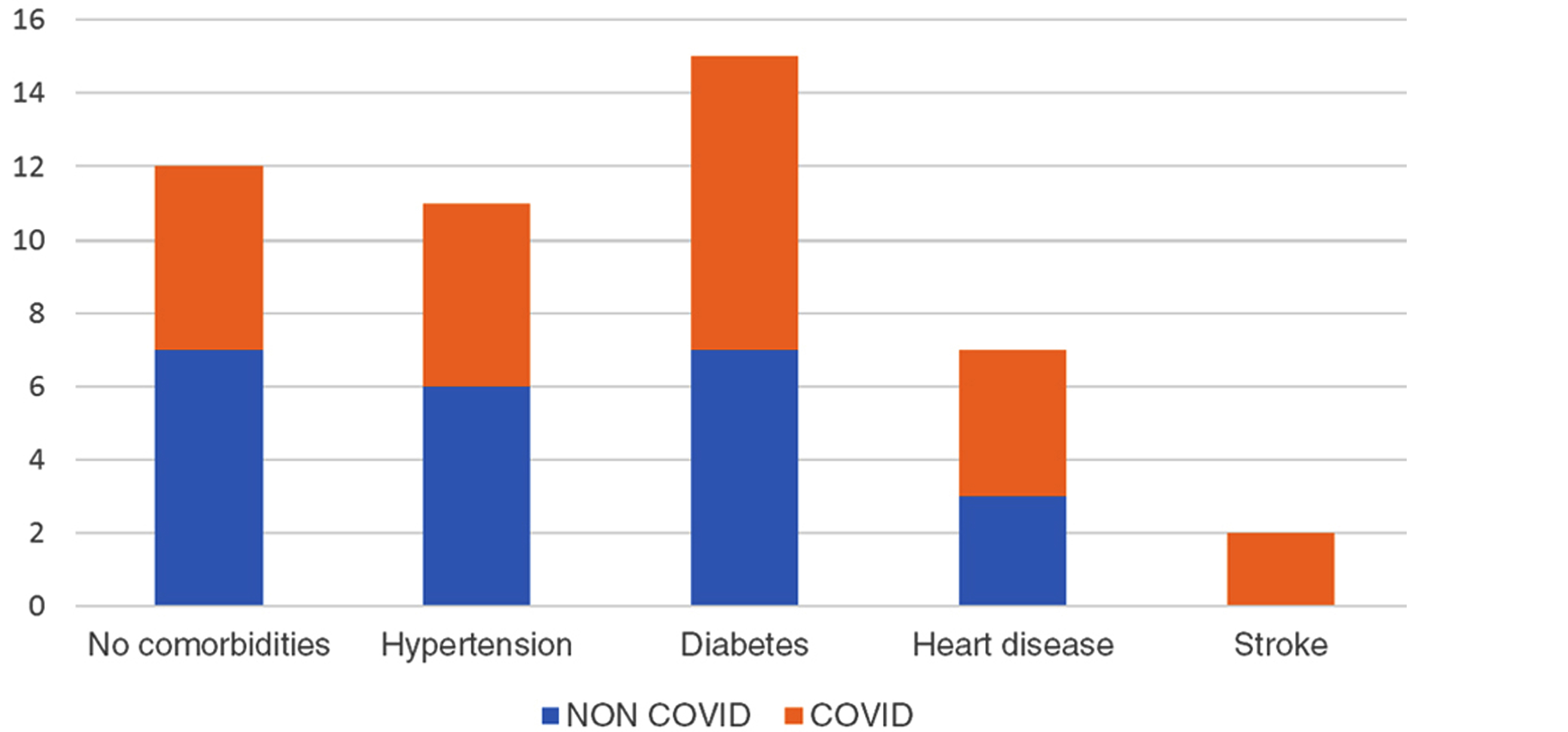
Figure 1: Distribution of comorbidities.
Clinical characteristics: Most of the patients presented to ER late (>24hr) from the time of onset of symptoms (abdominal pain, malena, vomiting) as shown in Figure 2. Out of 40 patients, 24 (60%) presented after 24 hrs of onset of symptoms.
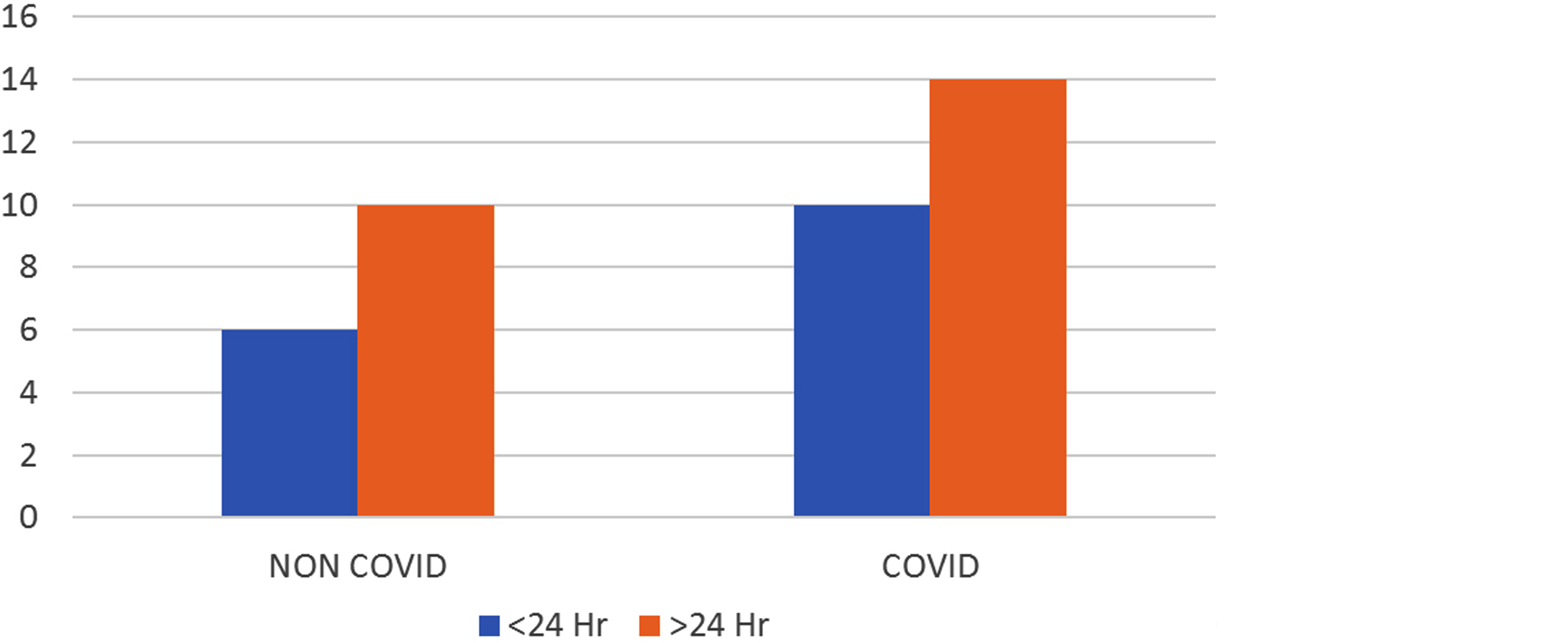
Figure 2: Time of presentation.
Intraoperative findings: In majority cases small bowel was involved as a part of bowel in both COVID (50%) and non-COVID (62.5%) (Figure 3). Resection and ostomy creation is done in all cases (double barrel ostomy) (Table 2).
Table 2: Surgical management.
|
Variables
|
COVID patients (24)
|
non-COVID patients (16)
|
|
Ischemia involved small bowel, n (%)
|
12 (50%)
|
10 (62.5%)
|
|
Ischemia involved large bowel, n (%)
|
8 (33%)
|
4 (25%)
|
|
Ischemia involved both small and large bowel, n (%)
|
4 (16.6%)
|
2 (12.5%)
|
|
Bowel resection during initial laparotomy, n (%)
|
24 (100%)
|
16 (100%)
|
|
Small bowel resection, n (%)
|
12 (50%)
|
10 (62.5%)
|
|
Large bowel resection, n (%)
|
8 (33.3%)
|
4 (25%)
|
|
Small and large bowel resection, n (%)
|
4 (16.6%)
|
2 (12.5%)
|
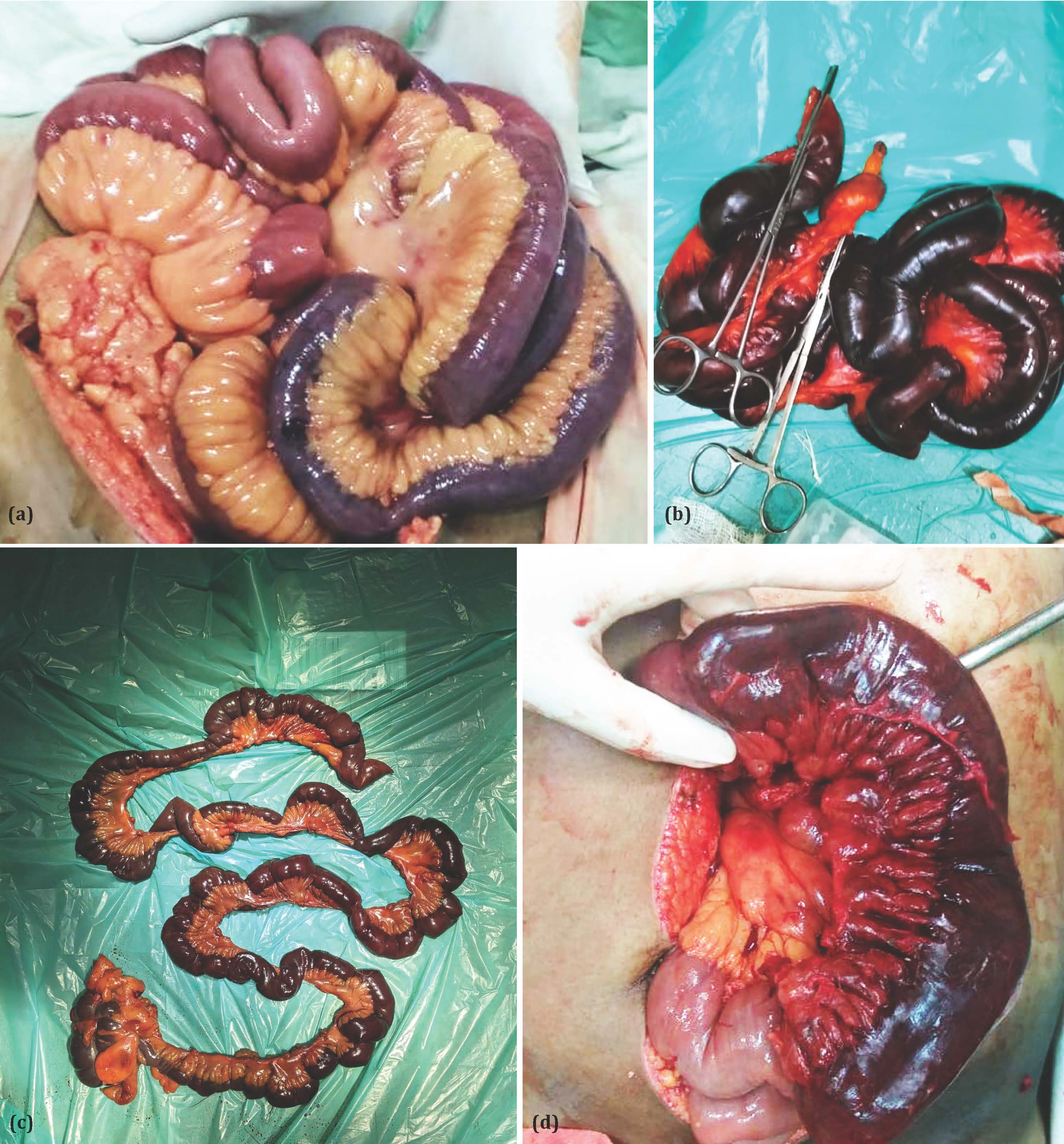
Figure 3: Intraoperative findings (a) Gangrenous small bowel with proximal viable bowel, (b) Resected gangrenous small bowel, (c) Extensive resection of small bowel, Ileo ceacal junction, part of ascending colon, and (d) Intra operative finding of gangrenous small bowel and viable bowel.
Outcomes (Mortality and length of hospital stay)
In distribution of mortality, we observed patients with active COVID infection had higher mortality of 75% (3 out of 4) followed by patients with past history of infection with mortality rate of 65% (13 out of 20) whereas the mortality rate in non-COVID patients being 37.5% (6 out of 16) which is less when compared to other groups as shown in figure 4. Using chi-square test, on comparing the mortality rates between COVID (active + past) and non-COVID groups p value was 0.069 which is insignificant (Figure 4).
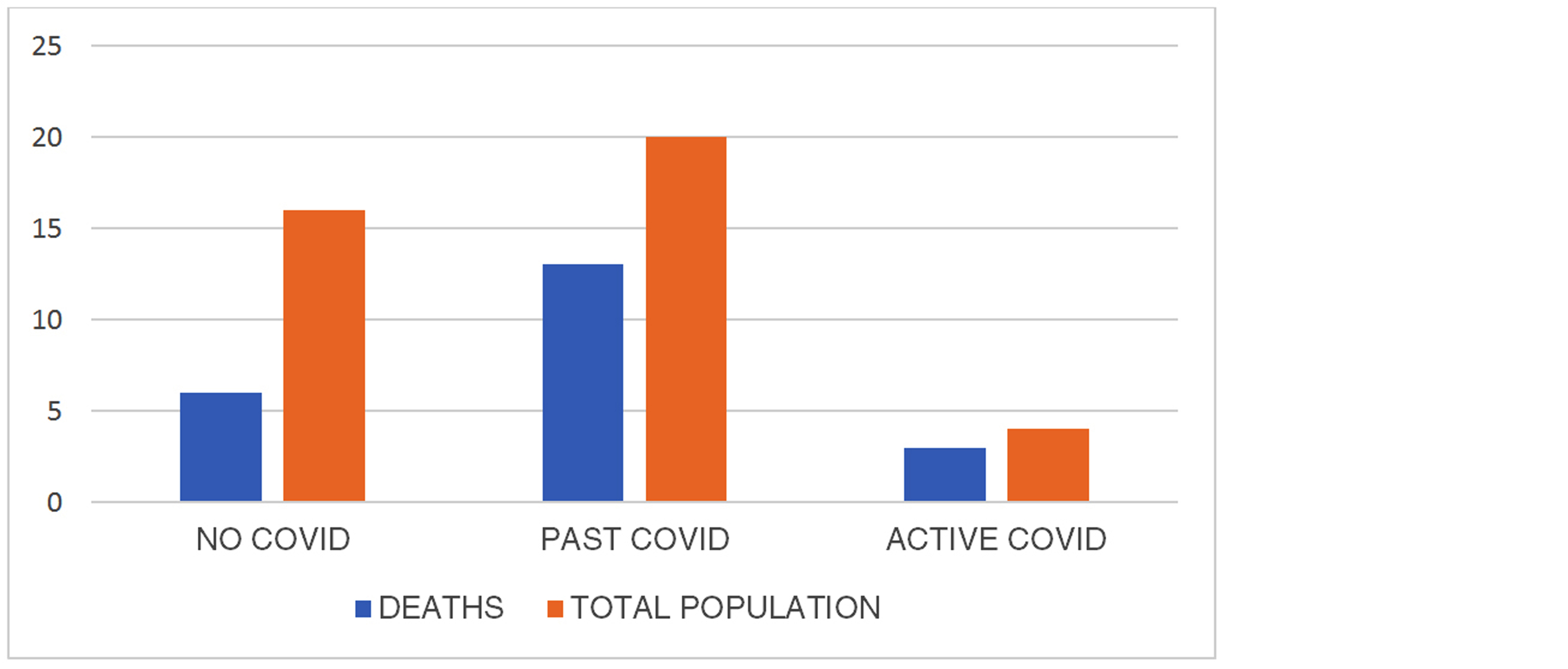
Figure 4: Distribution of mortality.
Average length of hospital stay in COVID (active +past) infection patients was 24.6 days whereas in non-COVID patient it was 18.4 days, using unpaired T test, P value was less than 0.001 which was significant (Table 3).
Table 3: length of stay.
|
COVID infection
|
Average length of stay
|
|
Past + active
|
24.6 days
|
|
No history
|
18.4 days
|
Discussion
The present study highlights a possible association between COVID-19 and intestinal ischemia. In the current environment of the COVID-19 pandemic, mesenteric ischemia should be suspected in any case presenting in an emergency with acute abdominal pain, and associated conditions.
Pathophysiology of association between COVID-19 and ischemic bowel is due to the high enterocytic attention of the ACE2 receptor, the receptor through which SARS-CoV- 2 invades the cells, could dispose the intestinal tract to direct viral incursion and damage. ACE2 receptors are substantially concentrated in the ileum and colon [3], the two common places of involvement in our cases. SARS-CoV-2 infects the host cells using angiotensin converting enzyme 2 which is a zinc-dependent metallopeptidase expressed by the cells of numerous organs including the lung, heart, intestine, and kidney [4]. In other words, ACE- 2 acts as a functional receptor of the virus. This means that endothelial dysfunction leading to hypercoagulability exists specifically in the bowel and is a direct cause of mesenteric thrombosis in COVID-19 cases.
Acute mesenteric ischemia (AMI) is a potentially life- threatening condition that has been described as a cause of disastrous abdominal events since the nineteenth century. Investigators have sought to identify factors that might indicate an poor prognosis and justify aggressive nature and need early intervention for the same [5].
In our study we've chose all the cases presented with acute abdomen to emergency room. They were originally assessed clinically and resuscitated with fluids and farther investigated biochemically and radiologically in which they were diagnosed to have acute ischemic bowel disease. After thorough resuscitation all cases were explored in emergency and preoperatively COVID-19 testing was done for every case as routine standard of care at our medical centre.
4 cases who came COVID positive were explored in COVID operation theatre by following proper safety guidelines and rest were explored in routine emergency operation theatre. Post operatively COVID positive cases were shifted to COVID wards and were managed as per COVID-19 guidelines concomitantly with routine post-operative care being antibiotic, fluid administration. All cases were started on anticoagulants post operatively. On detailed history, 15 out of 20 cases with history of COVID infection took anticoagulants and were needed oxygen in previous COVID infection.
In our study, males constituted 62.5% of the study population. Men might be at a higher threat of ischemic bowel complaint because they've more prevalence of atherosclerosis compared to ladies. With each year increase in age, the odds of mortality rose 1.09 times. Advanced age was significantly associated with mortality. A analogous finding is also reported by Aliosmanoglu et al [6].
Time of presentation to ER has been classically described as one of the most important determinants of mortality, no significant association was seen in the present study. Kassahun et al had reported survival rate of 50% when diagnosed within 24 hours which decreased to 30% when the diagnosis was made after 24 hours [7].
Extensive bowel involvement as shown in picture 3 was seen associated with COVID patients leading to resection of longer segments i.e., large bowel, ileo ceacal junction along with small bowel.
Acosta-Merida et al observed that colonic involvement with ischemia and especially colonic plus small intestinal involvement were negative prognostic factors [8].
Ischemic bowel disease has a poor prognosis. Numerous large clinical studies have reported mortality rates ranging from 30% to 85% [6, 9]. In our study, we observed patients with active COVID infection had higher mortality of 75% (3 out of 4) followed by patients with past history of infection with mortality rate of 65% (13 out of 20) whereas the mortality rate in non-COVID patients being 37.5% (6 out of 16) which is less when compared to other groups.
Early admission to hospital and advancement in surgical techniques along with newer modalities of treatment has led to a steady decrease in mortality in AMI over the last few decades.
However, despite the reduction in mortality, there is still significant morbidity present in patients with ischemic bowel disease and effect of COVID-19 infection further increases the mortality and morbidity as described in the study. Hence the high mortality and prolonged length of stay necessitate clinicians’ suspicion and attention to intestinal ischemia to prevent morbidity and mortality.
The limitations of the study is area and population from a tertiary care medical center in a specified geographical region, hence the findings in multicentre study and larger population studies are required to confirm the results.
Conclusion
Intestinal ischemia is one of the rare complications of COVID-19 infection. Intestinal ischemia could be secondarily to the infection or due to its complications. Although bowel necrosis among COVID-19 cases is rare, its association with high mortality rates and extended length of stay necessitates clinical suspicion and prompt intervention.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Bala M, Kashuk J, Moore EE, Kluger Y, Biffl W, et al. Acute mesenteric ischemia: Guidelines of the World Society of Emergency Surgery. World J Emerg Surg. 2017; 12:38.
[2] Jin B, Singh R, Ha SE, Zogg H, Park PJ, et al. Pathophysiological mechanisms underlying gastrointestinal symptoms in patients with COVID-19. World J Gastroenterol. 2021; 27:2341–2352.
[3] Nakhli RE, Shanker A, Sarosiek I, Boschman J, Espino K, et al. Gastrointestinal symptoms and the severity of COVID-19: disorders of gut–brain interaction are an outcome. Neurogastroenterol Motil. 2022; 5:e14368.
[4] Abufool LK, Al-Ozaibi LS. Intestinal ischemia as a complication of COVID-19. Dubai Med J. 2022; 5:58–61.
[5] Menges AL, Reutersberg B, Busch A, Salvermoser M, Feith M, et al. Early and Midterm Outcomes of Open and Endovascular Revascularization of Chronic Mesenteric Ischemia. World J Surg. 2020; 44:2804–2812.
[6] Aliosmanoglu I, Gul M, Kapan M, Arikanoglu Z, Taskesen F, et al. Risk factors effecting mortality in acute mesenteric ischemia and mortality rates: A single center experience. Int Surg. 2013; 98:76–81.
[7] Kassahun WT, Schulz T, Richter O, Hauss J. Unchanged high mortality rates from acute occlusive intestinal ischemia: Six year review. Langenbecks Arch Surg. 2008; 393:163–171.
[8] Acosta-Merida MA, Marchena-Gomez J, Hemmersbach-Miller M, Roque-Castellano C, Hernandez-Romero JM. Identification of risk factors for perioperative mortality in acute mesenteric ischemia. World J Surg. 2006; 30:1579–1585.
[9] Dhamnaskar S, Sawarkar P, Mandal S, Vijaykumaran P. Predictors of mortality in acute mesenteric vascular ischemia with bowel gangrene. Int Surg J. 2016; 3:1996–2002.