Full Text
Introduction
Fractures of the clavicle represent 2.6–4% of all fractures and is common in young males and elderly individuals often resulting from direct trauma to the shoulder. Most of the operative procedure performed under general anaesthesia give successful outcome, hence it’s the better option for clavicle fractures [1]. Advantages of General Anesthesia (GA) being completely relaxed and unaware patient, there are some disadvantages like post operative nausea, vomiting, headache, hemodynamic stress response and airway complications, which makes regional anesthesia techniques preferable [2]. Regional nerve blocks have the advantage as they avoid the side effects of general anesthesia. The suprascapular, subclavian, supraclavicular and long thoracic nerves, alone or in combination are responsible for cutaneous nerve supply in clavicular region.
Various regional blocks alone or in combination have been used for clavicle surgeries. These blocks are interscalene brachial plexus block (ISB), superficial cervical plexus block (SCPB), isolated C5 root block or suprascapular / supraclavicular nerve block (SCB) [2]. The sensory innervation of clavicle is controversial, receiving sensory branches from supraclavicular, subclavian and/or suprascapular nerves, which leads to unsatisfactory surgical anesthesia with interscalene blocks (ISB) [1].
The clavipectoral plane block (CPB) was first described in 2017 by Valdés as a simple and highly safe procedure for anesthesia and analgesia for clavicle surgeries. CPB is known to provide better pain relief for clavicular procedures in comparison to ISB [3].
CPB is given under ultrasound guidance or using a simple landmark technique. CBP seeks to establish field block surrounding the clavicle and encompasses all neural components that supply the clavicle. To achieve this, the local anesthetic must be applied to the medial and lateral thirds of the clavicle, situated amidst the fascia (clavipectoral fascia) and the clavicle's periosteum (periosteal collar) [3, 4]. The deposited drug surrounds the clavicle, involving all the nerves piercing the fascia to enter the clavicle. The success of the fascial plane block depends on the integrity of the fascia and the potentiality of the interfacial plane [3].
In this study we aim to compare block efficacy as well as the duration of post operative analgesia in superficial cervical plexus block with interscalene block versus superficial cervical plexus block with clavipectoral fascia block by comparing VAS score and satisfactory score of the patients among the two groups in the post operative period.
Material and methods
This is a prospective comparative observational study which was conducted on 70 patients in the Department of Anaesthesiology, in a tertiary care hospital after obtaining written informed consent from patient and approval from institutional ethical committee as well as Clinical Trial Registry of India (CTRI). The study was conducted from November 2022 to October 2023, for a duration of 12 months.
The sample size was estimated using the formula n = 2(Zα/2 +Zβ)2 σ2/d2, by considering the standard deviation of 1.96 and 0.84, respectively for each group. With the combined standard deviation of two groups (σ) as 2.99, the approximate standard deviation of 35 in each group was obtained. The scheme of patient recruitment for the study is shown in figure 1.
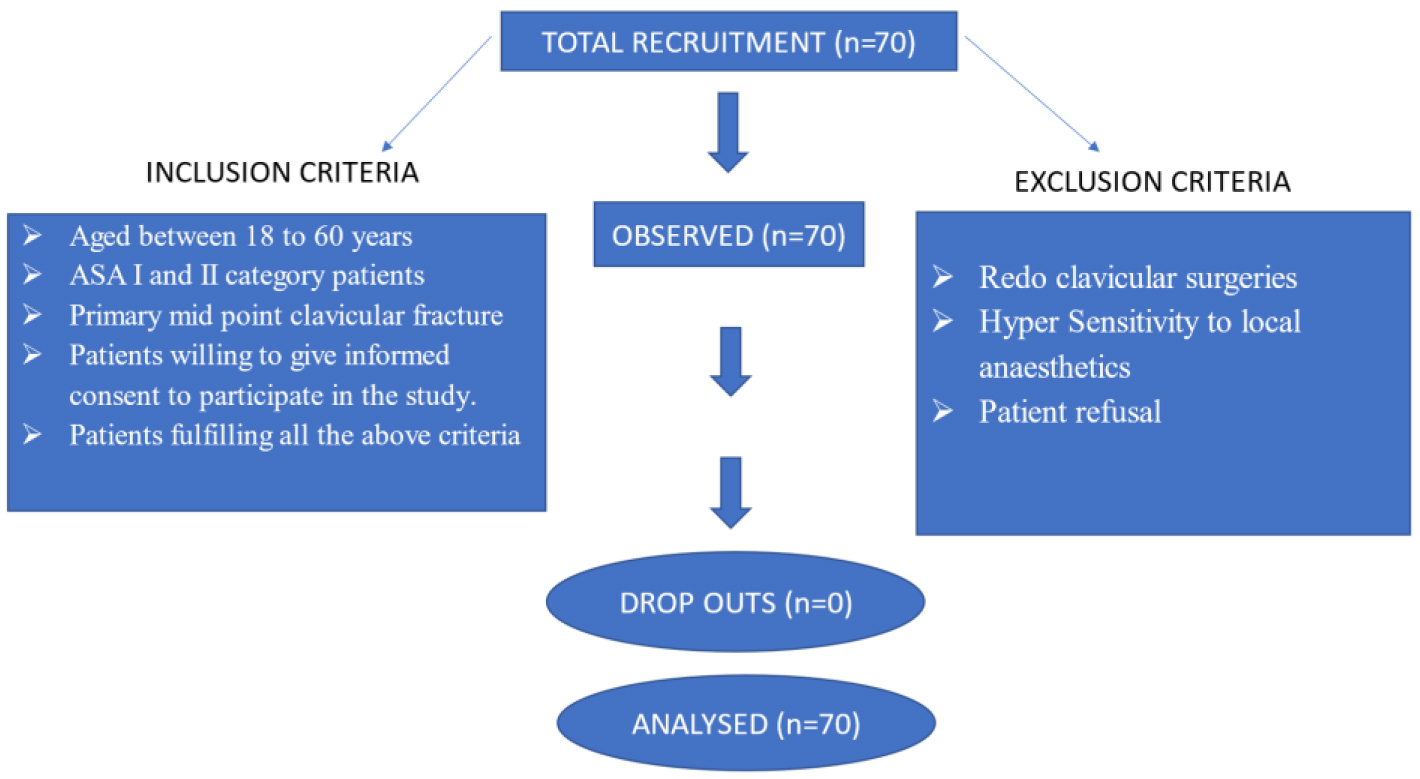
Figure 1: Showing the scheme of recruitment of study participants.
70 patients between age 18 to 60 years of either sex belonging to the American Society of Anaesthesiologists (ASA) physical class I and II posted for midpoint clavicle surgeries under peripheral nerve blocks were included in the study. Patients who are posted for redo clavicle surgeries, who has hypersensitivity to local anaesthetics and patients who refused to give consent were excluded from the study.
Patients details regarding their baseline pulse rate, systolic and diastolic blood pressure, mean arterial pressure and peripheral oxygen saturation (SPO2) were recorded. On arrival in operation theatre (OT), standard monitoring with non-invasive arterial pressure, electrocardiography and pulse oximetry was established. The base line vitals were noted. They were given midazolam 1 mg and inj. fentanyl 0.5 µg/kg .35 consecutive patients posted for clavicle surgeries in OT 1 received ISB with SCPB using USG guided technique with 1 mg/ kg bupivacaine and 3 mg/kg Lignocaine with adrenaline and making up to a volume of at least 20 ml with NS and SCPB with 0.5 mg/kg bupivacaine and 1 mg/kg lignocaine with adrenaline and making up to a volume of at least 10 ml with NS. Remaining 35 consecutive patients posted for clavicle surgeries in OT 2 received CPB with SCPB using a high-frequency linear probe (Sonosite HFL38x/13-6 MHz; Fujifilm SonoSite, Bothell, WA) placed on the anterior surface of the clavicle; by injecting 1 mg/ kg bupivacaine and 3 mg/kg Lignocaine with adrenaline and making up to a volume of at least 20 ml with NS in between the clavipectoral fascia and the periosteum on both sides of the clavicle fracture and SCPB with 0.5 mg/kg Bupivacaine and 1 mg/kg lignocaine with adrenaline and making up to a volume of at least 10 ml with NS.
Patients in both the groups were checked for adequacy of anaesthesia and analgesia under motor and sensory divisions. For motor response, subjects were instructed to elevate the shoulder and bend the elbow every 5 minutes following the block's administration for a total of 30 minutes. Motor response was assessed using a modified Bromage score ranging from 0 to 2. For sensory response, subjects were assessed for deep touch/pressure at the medial end, midpoint, and lateral end of the clavicle, every 5 minutes following the block administration for a total of 30 minutes.
If there is insufficient motor response after half an hour of administering the block, patients were intubated, and general anaesthesia was given using LMA or ETT. Number of patients with inadequate effect and requiring general anaesthesia were recorded in both the groups. HR, SPO2 and non-invasive blood pressure (NIBP: SBP and DBP) was recorded every 10 min during intraoperative period. The patient was observed for any discomfort or pain or change in vital parameters or any other side effect like hoarseness, difficulty in breathing, nausea/vomiting, etc., for first 24 hours. A rise/fall of >20% in hemodynamic parameters was considered as significant. Patient satisfaction score and duration of analgesia were monitored post operatively.
Results
The study was conducted on 70 patients where 35 patients received ISB with SCPB and remaining 35 patients received CPB with SCPB. Demographic variables such as age, sex and ASA were comparable between two groups. Majority of the patients who received CPB belonged to the age group pf 51-60 years (10/35; 28.6%), followed by 31-40 years and 41-50 years (9/35; 25.7%, respectively). Majority of the patients receiving ISB belonged to the age group of 31-40 years (10/35;28.6%), followed by 21-30 years and 51-60 years (8/35; 22.9%, respectively). The p value for the age group comparison among the two groups was 0.26, which was statistically not significant.
Out of 35 patients who received clavipectoral fascia block, 21 (60%) were males and 14 (40%) were females. Male: Female ratio for Clavipectoral fascia block patients was 1.5:1. Out of 35 patients who received interscalene block, 18 (51.4%) were males and 17 (48.6%) were females, with the Male: Female ratio of 1.05:1. The p value for gender comparison was 0.31, which was statistically not significant. The ASA grade was assessed among two groups. The CPB group had 19/35;54.3% belonging to group 1, and 16/35; 45.7% having grade 2 ASA score. Among the patients receiving ISB, 18/35;51.4% had a grade 1 score and 17/35; 48.6% had grade 2 ASA score. The ASA comparison among the two groups was not statistically significant (p value- 0.5).
The vital parameters were stable and near baseline readings during intraoperative as well as post operative period in all patterns. The mean baseline values for heart rate, SBP, DBP and MAP for patients receiving clavipectoral fascia block was 82.8 bpm, 120.3 mmHg, 73.3 mmHg, and 88.9 mmHg, respectively. The mean baseline values for Heart rate, SBP, DBP and MAP for patients receiving Interscalene block was 81.3 bpm, 119.6 mmHg, 75.2 mmHg, and 90.0 mmHg, respectively. The p value for each was 0.28, 0.69, 0.24, and 0.39, which were not statistically significant.
The average duration of analgesia in CPB +SCPB group was 12.5 hours as compared to 5.9 hours in ISB +SCPB. This difference was statistically significant with a p value of 0.01 (Table 1).
Table 1: Duration of analgesia by groups.
|
|
Clavipectoral fascia block
|
Interscalene block
|
P value
|
|
Duration of analgesia
|
12.5 (1.1)
|
5.9 (0.5)
|
0.01
|
In CPB +SCPB group, 29 patients were highly satisfied with the block characteristics while 6 patients were partially satisfied, on contrary 22 patients were highly satisfied with the block characteristics and 13 patients were partially satisfied in ISB +SCPB group. This difference in patient satisfaction scores between the two groups is statistically significant with p value 0.05. (Table 2). Modified Bromage score was statistically significant between the two groups with p value < 0.001 (Table 3).
Table 2: Patient satisfaction score by groups.
|
|
Clavipectoral fascia block
|
Interscalene block
|
P value
|
|
1
|
6 (17.1)
|
13 (37.1)
|
0.05
|
|
2
|
29 (82.9)
|
22 (62.9)
|
|
Total
|
35 (100)
|
35 (100)
|
Table 3: Modified bromage score by groups.
|
|
Clavipectoral fascia
block
|
Interscalene block
|
P value
|
|
0
|
35 (100)
|
0(0.0)
|
<0.001
|
|
1
|
0(0.0)
|
2 (5.7)
|
<0.001
|
|
2
|
0(0.0)
|
33 (94.3)
|
|
Total
|
35 (100)
|
35 (100)
|
Discussion
The mainstay of treatment for the fractures of clavicle is conservative management. If they are operated, they will be painful like any other fracture and require adequate post operative analgesia. There are not many reports regarding post operative analgesia for surgically operated clavicle fractures.
There are certain studies which show that ISB blocks have been used in combination or as a single technique to provide some degree of postoperative analgesia. There have been hardly any studies regarding CPB with SCPB as a sole anesthetic technique for post operative analgesia so, in this study we have compared CPB with SCPB and ISB with SCPB for post operative analgesia.
In 2019, Gupta et al conducted a study on 60 clavicle fracture patients by dividing into 2 groups, with one group receiving only interscalene block and another group receiving combination of interscalene block and superficial cervical plexus block. The adequacy of sensory block at mid-point of the clavicle and at the lateral end of clavicle and of motor block was similar in both the groups. The onset of sensory block at lateral end of the clavicle was faster in group receiving combination of interscalene block and superficial cervical plexus block. The sensory block at medial end of clavicle was significantly faster and adequate in group receiving combination of interscalene block and superficial cervical plexus block. The surgeons' rating was excellent in group receiving combination of interscalene block and superficial cervical plexus block and satisfactory in group receiving only interscalene block. They concluded that ISB+SCPB is superior to ISB alone as regional anesthesia technique for surgical fixation of clavicular fractures. But in our study, we have compared the patient satisfaction score rather than surgeons’ satisfaction score and found that patient`s satisfaction score being excellent in CPB with SCPB rather than ISB with SCPB [5].
In 2022, Jyothi P. Deshpande et al have done a case series on 12 patients and reported that USG guided CPB is a good regional anesthesia technique that provides safe and precise postoperative analgesia for clavicle surgeries without any adverse effects. Even the lesser dose of anesthesia gives adequate anesthetic effect required. They have found that the average duration of analgesia was around 10 to 13 hours with a VAS score from 2 to 4 [6]. Average duration of analgesia was around 12.5 hours with clavipectoral fascia block and with interscalene block , the average duration of analgesia was around 5.9 hours in our study (p value of 0.01) .The rate of post operative complications such as post operative nausea and vomiting , giddiness was found to be higher in the above study but these were attributed to the use of general anesthesia rather than CPB as concluded in the study. No post-operative complications were found in our study.
In 2020 Magnus Olofsson et al conducted a matched case control study in order to assess the analgesic efficacy of an interscalene brachial plexus block (ISB) by comparing 50 consecutive patients scheduled for surgical fixation of middle/lateral clavicle fracture under general anaesthesia with ISB with historical control of 76 retrospective patients without regional block. In this study, before matching, patients who were given ISB had a low I.V morphine consumption (mean difference 0.7 mg)when compared to control patients(mean difference 8.8 mg) which is statistically significant (p< 0.001). After matching, the mean difference was 8.3 mg which is statistically significant (P < 0.001) [7]. This study also supports the finding of prolonged duration of post operative analgesia in our study.
With the advent of ultrasound guided CPB, regional anesthesia for clavicle fractures has gained importance. Utilizing regional methods enhances postoperative recovery, resulting in quicker mobilization due to decreased pain and earlier discharge. Furthermore, the minimal use of opioids decreases postoperative issues such as PONV and dizziness, enhancing the postsurgical results [8, 9].
Another advantage of CPB is that it can be utilized in patients with trauma having occult pneumothorax where administering general anesthesia may aggravate the pre-existing pathology of pneumothorax and further complicate the condition and patients with bilateral clavicle fractures where the administration of bilateral nerve block is not feasible thereby, we can avoid administration of GA in the group of patients [9, 10].
Our study shows that the duration of post operative analgesia is significantly higher in CPB with SCPB group than in group receiving ISB with SCPB with a p value of < 0.001. All patients were comfortable and had no adverse events in the intraoperative period. Two patients were uncomfortable in the mobilization of fracture which can be justified by the patient’s psychological anxiety in the usage of upper limb with no motor paralysis and was managed with inj. ketamine 50 mg intravenously. Since the patient does not have motor block of upper limb on the operated side, patients’ satisfaction score was significantly more in CPB+SCPB group as compared to ISB +SCPB group during post operative period (p value 0.05).
Limitations of the study: This is a single institute study that was conducted on a small group of study population. Thus, we recommend the study trial to be conducted on a larger population to obtain the generalized data.
Conclusion
This study suggests that the ability of the patient to mobilize the upper limb on the operated side in CPB +SCPB group was dramatically higher in comparison to the ISB+SCPB in the immediate post-operative period. Thus, this study concludes that CBP+SCBP had better efficacy, longer duration of post-operative analgesia and superior patient satisfaction compared to ISB+SCBP.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Balaban O, Dulgeroglu TC, Aydın T. Ultrasound–guided combined interscalene–cervical plexus block for surgical anesthesia in clavicular fractures: A retrospective observational study. Anesthesiol Res Pract. 2018; 2018:7842128.
[2] Kukreja P, Davis CJ, MacBeth L, Feinstein J, Kalagara H. Ultrasound–guided clavipectoral fascial plane block for surgery involving the clavicle: A case series. Cureus. 2020; 12:e9072.
[3] Kartik S, Hrudini D, Balavenkatasubramanian, Palanichamy G. Uncovering secrets of the beauty bone: A comprehensive review of anatomy and regional anesthesia techniques of clavicle surgeries. Open J Orthop Rheumatol. 2021;19–29.
[4] Gonçalves D, Sousa CP, Graça R, Miguelez MP, Sampaio C. Clavipectoral fascia plane block combined with superficial cervical plexus block for the removal of osteosynthesis material from clavicle fracture. Cureus. 2023; 15:e43146.
[5] Gupta N, Gupta V, Kumar G, Gupta V, Gupta DK. Comparative evaluation of efficacy of interscalene block vs Interscalene block and superficial cervical plexus block for fixation of clavicular fractures. Int J Contemp Med Res. 2019; 6.
[6] Panse NA, Deshpande JP, Panse NA. Efficacy of clavipectoral fascia plane block as analgesic modality in clavicle fractures: Exploring New Horizons. Anesthesia and Clinical Research. 2022; 1–4.
[7] Olofsson M, Taffé P, Kirkham KR, Vauclair F, Morin B, et al. Interscalene brachial plexus block for surgical repair of clavicle fracture: a matched case–controlled study. BMC Anesthesiol. 2020; 20:91.
[8] Azikakath MSS, Tanna D, Parikh N, Bose N, Vasava JC. Ultrasound guided combined interscalene–superficial cervical plexus block in clavicular fractures for surgical anesthesia: A retrospective observational study. MedPulse Int J of Anesthesiol. 2022; 21:12–16.
[9] Labandeyra H, Heredia C, Váldes–Vilches LF, Prats–Galino A, Sala–Blanch X. Clavipectoral fascia plane block in midshaft clavicle fractures: A cadaveric study. J Clin Anesth. 2024; 96:111469.
[10] Pereira CS, Ferros C, Dinis I, Pereira D, Miguel D, et al. Clavipectoral fascial plane block for clavicle fracture surgery: A case report. J Peri oper Pract. 2024; 34:375–377.