Full Text
Introduction
Stroke, the second leading cause of death and a major cause of disability worldwide [1], results in over 12.2 million new cases annually [2]. The burden is particularly heavy in low and middle-income countries, including India, where stroke is the fourth leading cause of death [3]. In India, the annual incidence ranges from 105 to 152 per 100,000 people [4]. Globally, over 101 million people live with stroke's effects, with women comprising 53% of cases. Each year, 5 million people die from stroke, and another 5 million are left permanently disabled, significantly impacting families and communities [5].
The prevalence of stroke has surged in recent years, with a notable 50% increase over the past 17 years, affecting approximately 1 in 4 individuals [6]. This rising incidence can be attributed to an alarming increase in hypertension, hyperlipidemia, diabetes mellitus, and other chronic disorders [7], coupled with lifestyle factors such as physical inactivity, smoking, obesity, inadequate fruit and vegetable consumption, and high sodium intake [8]. While established risk factors such as diabetes mellitus and hypertension are well-documented contributors to stroke [9], there remains a significant challenge in identifying and managing these factors before they lead to severe outcomes. Many individuals may have these risk factors undiagnosed (denovo) and sometimes inadequately treated even after diagnosis.
Stroke incidence can also be triggered by a variety of factors, many of which are related to underlying health conditions and lifestyle choices. Extreme physical exertion and emotional stress, such as intense anger or depression, can lead to physiological changes in the body, such as elevated blood pressure, increased heart rate, and heightened levels of stress hormones like cortisol, all of which can contribute to the conditions that predispose someone to a stroke [10]. The challenge in pinpointing physical exertion or emotional stress as direct triggers lies in the multifaceted nature of stroke. A stroke typically occurs due to the cumulative effects of long-standing vascular issues, such as atherosclerosis, hypertension, or other cardiovascular conditions [11]. In the presence of these underlying conditions, extreme physical or emotional stress may act as a catalyst by causing sudden, significant changes in blood pressure or heart rhythm, which can lead to a stroke [10]. Yet, these events do not always result in an immediate stroke, suggesting that additional factors or a critical threshold may need to be crossed for a stroke to occur. Understanding these triggers is crucial for stroke prevention and management, as addressing them can significantly reduce the risk of stroke occurrence.
This study sought to provide comprehensive insights into the prevalence of risk factors and triggers, with a particular focus on identifying and understanding both denovo and uncontrolled known risk factors. The findings from this research are expected to significantly enhance the understanding and management of stroke.
Methods
Study design and setting
This prospective observational study was conducted in the Department of Neurology at KIMS Hospitals, Secunderabad. The study spanned from August 2023 to November 2023 and included 100 patients who presented with stroke. The study was approved by the Institutional Ethics Committee of KIMS Hospitals (KIMS/EC/BMHR/2023/67-01) and adhered to the Helsinki guidelines for ethical research involving human subjects. All patients were informed about the study's purpose, and written informed consent was obtained from each participant before their inclusion in the study.
Study population
Patients aged 16 and above with an acute neurological deficit suggestive of stroke were eligible for inclusion in the study. Those with symptoms unrelated to acute stroke or those who were non-compliant with the study protocol were excluded.
Data collection
A structured study questionnaire was developed to capture both clinical and non-clinical information from the patients. The questionnaire included sections on: Demographic information (age, gender, occupation, educational background); Medical history (hypertension, diabetes mellitus, hyperlipidaemia, history of previous strokes or transient ischemic attacks, medication history); Stroke-specific information (time of onset of stroke symptoms, type of stroke-ischemic, haemorrhagic, transient ischemic attacks, presenting symptoms e.g., hemiplegia, speech disturbances, visual impairment); Risk factors (Lifestyle factors such as smoking, alcohol consumption, diet, physical activity, family history of stroke or cardiovascular diseases, comorbid conditions); Triggers (Recent physical or emotional stress, infection, missed medication or fever prior to stroke onset).
Upon presentation to the Neurology Department, patients with suspected stroke were evaluated by a neurologist. Eligible patients were then approached by the research team to explain the study details and obtain informed consent. Once consent was obtained, the structured questionnaire was administered through direct interviews and medical record reviews.
Patients underwent standard diagnostic procedures, including clinical examinations, and relevant laboratory tests to confirm the diagnosis of stroke and to classify the type of stroke. The collected data were then entered into a secure database for analysis.
Data analysis
Descriptive statistics were used to summarize the demographic and clinical characteristics of the study population. Continuous variables were expressed as means and standard deviations, while categorical variables were presented as frequencies and percentages. Comparative analyses were conducted to examine the prevalence of various risk factors and triggers among different subgroups (e.g., ischemic vs. hemorrhagic stroke, male vs. female patients).
To ensure data quality, all questionnaires were reviewed for completeness and accuracy. Any discrepancies or missing information were resolved through follow-up interviews with patients or consultations with their medical records.
Results
Demographic characteristics
The study cohort consisted of 100 patients, ranging in age from 16 to 90 years (Table 1).
Table 1: The age distribution.
|
Age range (years)
|
Number of patients
|
|
16 – 30
|
1
|
|
31 - 45
|
15
|
|
46 - 60
|
32
|
|
61 - 75
|
42
|
|
76 – 90
|
10
|
In terms of gender distribution, 69% of the patients were male and 31% were female, resulting in a male-to-female ratio of 2.22:1.
Stroke types and mechanisms
Among the 100 patients in the study, 81% experienced ischemic strokes, while 19% suffered haemorrhagic strokes (Figure 1a). In the haemorrhagic stroke group, the majority of cases were primarily attributed to hypertension. Whereas the mechanisms underlying ischemic stroke were diverse: 40% were due to large artery intracranial atherosclerosis (ICA), 9% to large artery extracranial atherosclerosis (ECA), 14% to lacunar stroke, 9% to cardioembolic stroke, and 18% to unknown mechanisms (Figure 1b). In the study population, 75% were experiencing a stroke for the first time, whereas 25% had a recurrence following a previous stroke (Figure 1c).
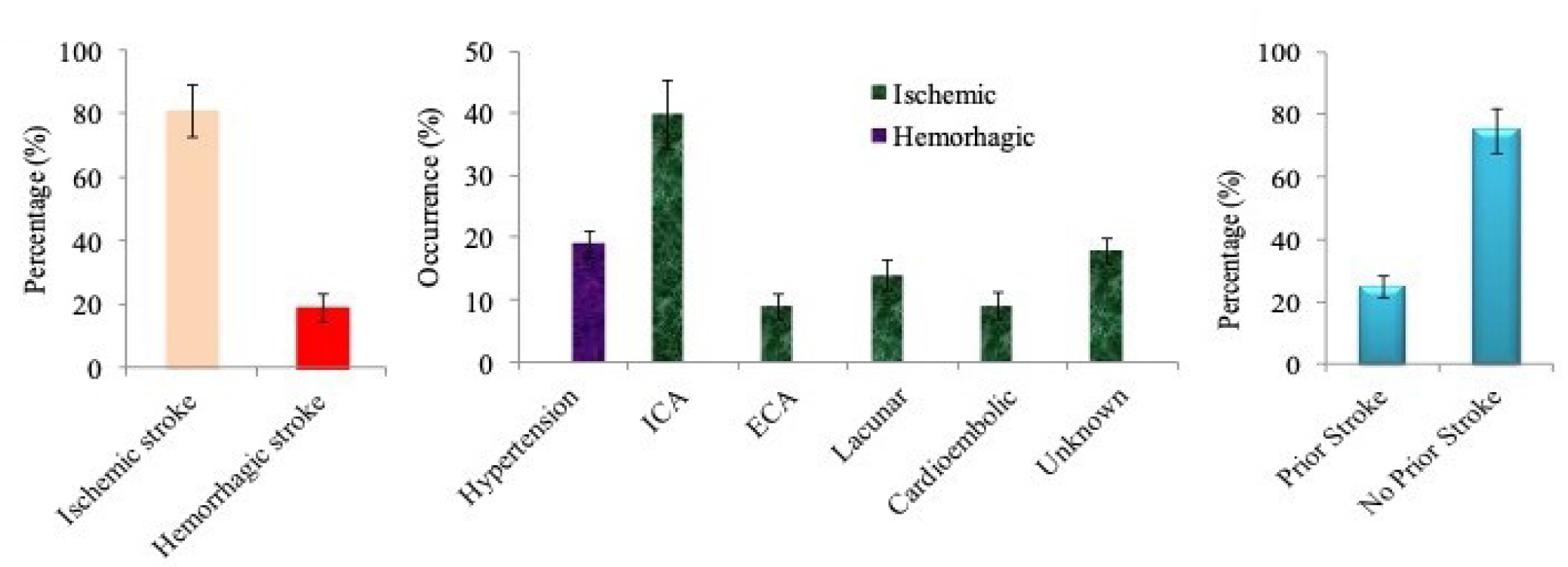
Figure 1: Stroke types and mechanisms, (a) Distribution of stroke types; (b) Mechanism underlying hemorrhagic and ischemic stroke; (c) Stroke recurrence.
Risk factors
The most common risk factors identified in our study population were hypertension and diabetes mellitus. Hypertension was the primary risk factor, affecting 84% of patients, with 58% being male and 26% female (Figure 2a). Among these patients, 44% had controlled hypertension through medication, 31% were uncontrolled hypertensives, and 9% were newly diagnosed (denovo) hypertensives (Figure 2b). Diabetes was the second major risk factor, present in 53% of patients, comprising 37% male and 16% female (Figure 2c). Within the diabetic group, 13% had controlled diabetes, 36% were uncontrolled diabetics, and 4% were newly diagnosed (denovo) diabetics (Figure 2d). Our further analysis revealed that approximately 81% of patients had an awareness of stroke, while 19% lacked any knowledge about it (Figure 2e).
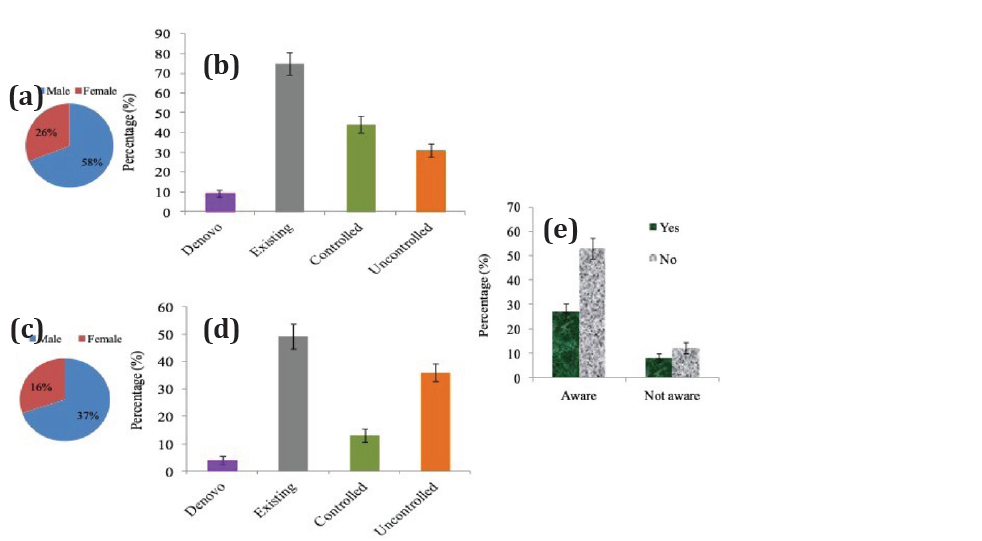
Figure 2: Risk Factors associated with stroke, (a) Gender distribution of patients with hypertension; (b) Hypertension control status among patients; (c) Gender distribution of patients with diabetes; (d) Diabetes control status among patients; (e) Awareness of stroke among patients.
Triggers
The study primarily investigated the triggers observed on the day of stroke onset. It was found that 65% of patients had no identifiable triggers. Among those with triggers, 6% experienced financial stress, another 6% encountered work-related stress, and 6% reported missing medication or having a fever/infection as contributing factors. Additionally, 4% of patients experienced anger prior to stroke onset, while 2% reported headache and family stress. Notably, chain smoking, alcohol binge, and sad emotional stress were identified as triggers in 3% of the study population (Figure 3a).
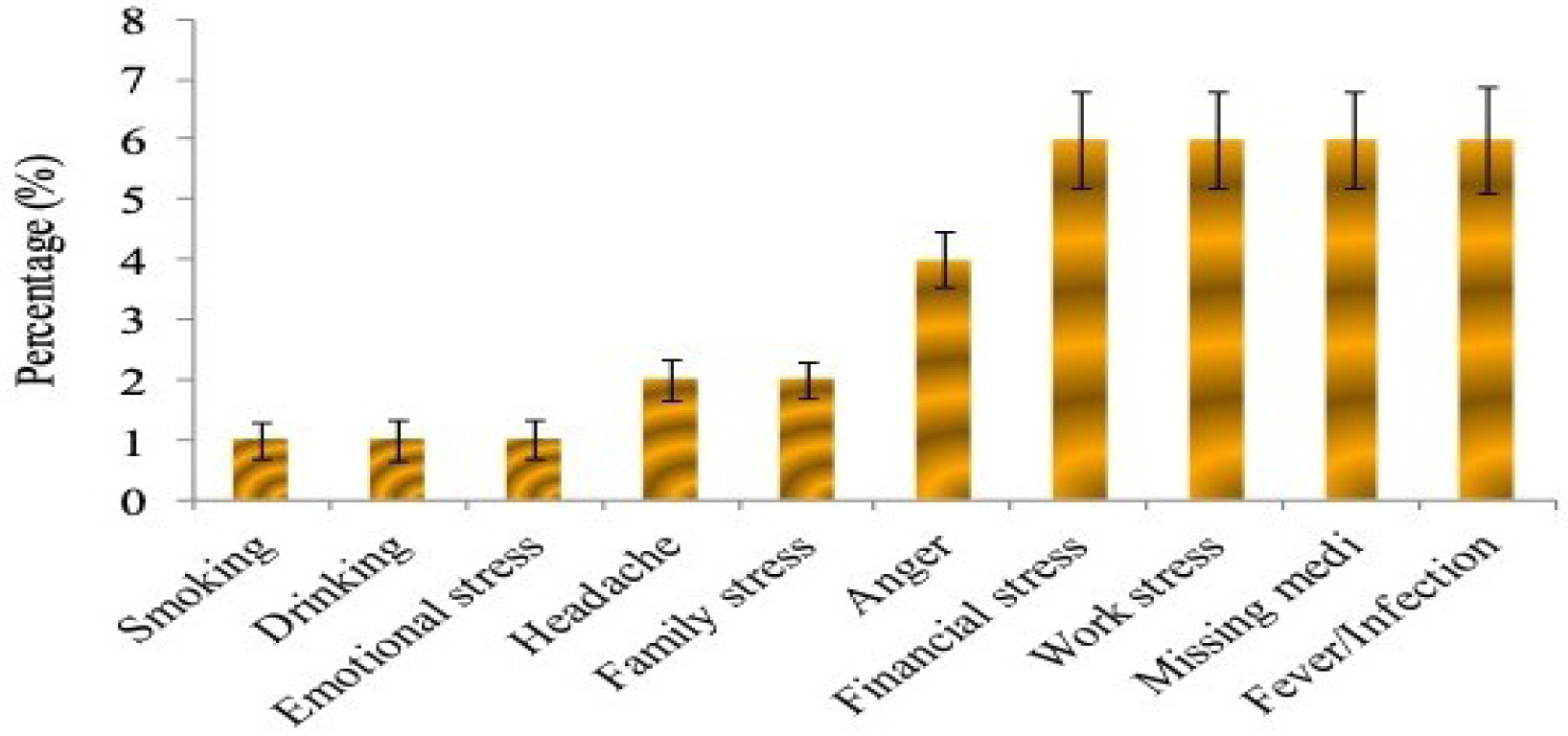
Figure 3: Potential triggers for the onset of stroke, triggers observed on the day of stroke onset.
Discussion
India faces a staggering burden of stroke, with over 15 lakh new cases annually (almost 4,000 daily) due to a lack of awareness about stroke symptoms, risk factors, and the “golden hour” for timely intervention [12]. Our study provides essential insights into the prevalence and distribution of both existing and newly identified (denovo) risk factors for stroke, which could aid in disease management. Additionally, this study evaluated triggers on the day of stroke occurrence to understand their impact on the onset or severity of stroke.
The study revealed that ischemic stroke was the most prevalent type of stroke observed, followed by haemorrhagic stroke. The underlying mechanisms driving these two types of strokes were distinctly different. Intracranial atherosclerosis emerged as the primary mechanism for ischemic stroke, wherein the build-up of fatty deposits within the arteries led to restricted blood flow to the brain [13]. On the other hand, hypertension was identified as the leading cause of hemorrhagic stroke, where elevated blood pressure resulted in the rupture of small blood vessels within the brain [14].
A critical finding of our study was the significant impact of undetected (denovo) and uncontrolled hypertension and diabetes mellitus as a major contributor to stroke in our cohorts. Our findings were consistent with existing literature [15], as we discovered that 9% and 4% of our patients were diagnosed with denovo hypertension and diabetes mellitus, respectively, following the onset of stroke. Furthermore, the study highlighted a concerning prevalence of uncontrolled chronic conditions within our patient cohort. Specifically, 31% of patients had uncontrolled hypertension, and 36% had uncontrolled diabetes mellitus. These uncontrolled conditions are likely to have played a significant role in elevating the risk of stroke in these individuals [8].
The role of acute triggers in the onset of stroke has been a subject of increasing interest, complementing the well-established understanding of chronic risk factors such as hypertension and diabetes mellitus [16]. In our study, we observed that approximately 29% of patients experienced significant stress—be it financial, work-related, emotional, or familial - on the day of stroke. Additionally, 6% of patients reported missing essential medications or having recent infections as immediate precipitating factors. Our findings align with existing literature that identifies stress as a significant, albeit often underrecognized, contributor to stroke incidence [16]. Studies have demonstrated that individuals experiencing high levels of psychosocial stress have a markedly increased risk of both ischemic and hemorrhagic strokes [17]. The INTERSTROKE study [10], identified stress and stressful life events as important risk factors for acute stroke across diverse populations. Our findings thus emphasize the significant impact of modifiable acute triggers such as stress, medication non-adherence, and infections on stroke incidence. Addressing these through targeted interventions, such as stress reduction, mental health support, patient education, and infection control, could reduce stroke rates and improve outcomes.
Our study revealed that while most patients were aware of stroke symptoms and risk factors, a small percentage lacked awareness, potentially delaying symptom recognition and medical care, leading to poorer outcomes. Bridging this gap through community education, informational materials, and local media can enhance awareness, prompt timely interventions, and improve stroke management, ultimately reducing incidence and improving outcomes.
Conclusion
Our study emphasizes the significant impact of hypertension, diabetes, and various triggers on stroke occurrence. Ischemic strokes were notably more prevalent, occurring nearly four times more often than haemorrhagic strokes. A key finding of our study was the substantial contribution of denovo hypertension and diabetes mellitus, along with poorly managed cases of these conditions to stroke incidence. Stress in its various forms emerged as a major trigger, though a considerable number of patients reported no identifiable triggers. These findings emphasize the need for heightened awareness and proactive management of stroke risk factors across all demographics. Future research with larger sample sizes is essential to further validate and expand upon these findings.
Acknowledgement
We would like to extend our sincere gratitude to all the patients and their caregivers who participated in this study.
Conflict of interest
There is no conflict of interest to declare.
References
[1] Katan M, Luft A. Global burden of stroke. Semin Neurol. 2018; 38:208–211.
[2] GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021; 20:795–820.
[3] Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, et al. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int J Stroke. 2022; 17:18–29.
[4] Jones SP, Baqai K, Clegg A, Georgiou R, Harris C, et al. Stroke in India: A systematic review of the incidence, prevalence, and case fatality. Int J Stroke. 2022; 17:132–140.
[5] Kuriakose D, Xiao Z. Pathophysiology and treatment of stroke: Present status and future perspectives. Int J Mol Sci. 2020; 21:7609.
[6] Pandian JD, Srivastava MVP, Aaron S, Ranawaka UK, Venkatasubramanian N, et al. The burden, risk factors and unique etiologies of stroke in South–East Asia Region (SEAR). The Lancet. 2023; 17:100290.
[7] Maida CD, Daidone M, Pacinella G, Norrito RL, Pinto A, et al. Diabetes and ischemic stroke: An old and new relationship an overview of the close interaction between these diseases. Int J Mol Sci. 2022; 23:2397.
[8] Liu Y, Wang H, Bai B, Liu F, Chen Y, et al. Trends in unhealthy lifestyle factors among adults with stroke in the United States between 1999 and 2018. J Clin Med. 2023; 12:1223.
[9] Morsy EY, Rohoma KH, Ali SAM, Elhalawany SH. Comparison study of clinical presentation and risk for cerebrovascular stroke in diabetic versus nondiabetic patients. The Egyp J Int Med. 2022; 34:78.
[10] Smyth A, O’Donnell M, Hankey GJ, Rangarajan S, Lopez–Jaramillo P, et al. Anger or emotional upset and heavy physical exertion as triggers of stroke: the INTERSTROKE study. Eur Heart J. 2022; 43:202–209.
[11] Abroix A. Cardiovascular risk factors for acute stroke: Risk profiles in the different subtypes of ischemic stroke. World J Clin Cases. 2015; 3:418–429.
[12] Kamalakannan S, Gudlavalleti ASV, Gudlavalleti VSM, Goenka S, Kuper H. Incidence and prevalence of stroke in India: A systematic review. Indian J Med Res. 2017; 146:175–185.
[13] Qin C, Yang S, Chu YH, Zhang H, Pang XW, et al. Signaling pathways involved in ischemic stroke: molecular mechanisms and therapeutic interventions. Signal Transduction and Targeted Therapy. 2022; 7:215.
[14] Unnithan AKA, Das JM, Mehta P. Hemorrhagic stroke. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024.
[15] Liu Y, Li J, Dou Y, Ma H. Impacts of type2 diabetes mellitus and hypertension on the incidence of cardiovascular diseases and stroke in China real–world setting: a retrospective cohort study. BMJ Open. 2021; 11:e053698.
[16] Ekker MS, Verhoeven JI, Rensink KML, Schellekens MMI, Boot EM, et al. Trigger factors for stroke in young adults: A case–crossover study. Neurology. 2023; 100:e49–e61.
[17] Reddin C, Murphy R, Hankey GJ, Judge C, Xavier D, et al. Association of psychosocial stress with risk of acute stroke. JAMA Netw Open. 2022; 5:e2244836.