Full Text
Introduction
Distal femur fractures involve fracture in the distal portion of femur (from metaphyseal-diaphyseal junction till knee articulate surface), encompassing epiphysis and metaphysis. This can be simple to complex intra-articular fracture [1]. The incidence of distal femur fracture is 8.7/1,00,000/year [2]. In United states incidence was found to be 37/100000/year [3]. Prevalence of distal femur fracture is very minimal, it is even less than 1% and it constitutes 6% of the femur fractures [4, 5].
It has bimodal age distribution, and it is more prevalent among young males after heavy force trauma and is also more prevalent among elderly females due to osteopenia and osteoporosis. It is also associated with comorbidities such as diabetes or hypertension [6]. Most common complication is malunion which leads to arthritis of both medial and lateral compartment of knee joint [7]. Loss of the range of motion is another challenging complication particularly among young individuals who have undergone high energy trauma [8]. Other complications include nonunion, knee stiffness and infection [9, 10].
Moreover, it poses significant challenges in orthopedic care, demanding precise surgical interventions for optimal outcomes. In spite of the advanced fixation technique, it still leads to poor clinical outcomes and persistent disability [9]. The complexity of these fractures, especially Muller’s Type C2 and C3 variants, often requires stable fixation. Dual implants, such as double-plate and plate-and-nail constructs, have emerged as viable options for achieving anatomical reconstruction. Understanding the background of these procedures is crucial for advancing the management of distal femoral fractures.
Despite the increasing incidence of distal femur fractures, there exists a noticeable gap in the literature concerning the retrospective assessment of clinical outcomes specifically related to double fixation constructs. The available studies often lack a focused evaluation of dual-implant techniques, leaving a void in evidence-based practices. Addressing this gap is crucial for refining treatment protocols and providing more nuanced insights into the efficacy of these procedures.
With a specific focus on dual-plate and plate-and-nail constructs, the study aims to comprehensively evaluate the effectiveness of these interventions in achieving good stability, good range of motion, union rate, and early mobility in high energy trauma, with minimal hospital stay, reduction of implant failure and limb salvage, and minimizing complications. The findings from this study hold the potential to guide orthopedic practitioners in making informed decisions regarding the selection and application of dual fixation constructs for distal femoral fractures, ultimately enhancing patient care and outcomes.
The study aimed to estimate the effect of dual implantation in distal femur fracture on union and clinical outcomes of the patients.
Materials and methods
This longitudinal study was done among patients of Dr. B. R. Ambedkar Medical College and Hospital, Bangalore, who underwent surgery with dual implantation for open or closed fractures of distal end femur. The total study period was 18 months from September 2022 to February 2024.
From a study done by Soe et al [11] on outcome of fracture union following dual plating of unstable distal femoral fracture it was found that 96% of patients achieved union. So, substituting the outcome incidence in the formula z2PQ/L2 with P as 96%, Q as 100-P that is 4%, Z as 1.96 and L as absolute precision of 7%, final sample size calculated was 30. 30 patients who underwent double implant surgery for distal femoral fracture during our reference period were selected using consecutive sampling and were included in the study. Patients with Muller’s classification of C2 and C3 types of distal end femur (C2: Articular simple, metaphyseal complex. C3: Multi fragmentary articular fracture), and patients with periprosthetic fracture or implant failure were included. Exclusions from the study involved delayed or old fractures, pathological fractures, pediatric distal femur fractures, and other Muller’s classification types of fractures.
Institutional ethical clearance was got. Written informed consent was also got from the patients. Confidentiality of the study population was maintained throughout the study. Data was collected using a pre-designed semi-structured validated questionnaire. The demographics and relevant histories of each individual were retrieved as secondary data from the records. Data on detailed characteristics of each fracture, including laterality, type, knee derangement, mode of injury, and associated injuries, were also collected. Overall, it was made sure that all the patients included in the study had undergone distal femur plating by both medial and lateral plate. Patients were evaluated for the union and clinical outcome parameters like range of motion, work capacity and complications by being followed up for 9 months or till radiographic union.
Range of movement, angular deformity, infection, limb length deformity, union, work capacity were the outcome variables used to assess the effect of double implants. The details compiled from the selected cases were documented in Microsoft Excel. Analysis was done using SPSS software version 23. Descriptive statistics, such as means and standard deviations, were used to represent continuous data, while categorical data was expressed in frequencies and proportions. Chi-square test was used to find the association between two qualitative variables and independent sample t test was used to find difference between two groups.
Results
The commonest age group in our study was found to be above 60 years (30.0%), and majority were males (53.3%). About 60.0% cases were having one or more comorbidities such as diabetes, or hypertension. And risk factors such as smoking as well as alcohol were present in about 43.3% cases (Table 1).
Table 1: Characteristics of the study subjects (n=30).
|
Subjects (N=30)
|
Frequency (N)
|
Percentage (%)
|
|
Age group
|
<30 years
|
6
|
20.0%
|
|
31 to 45 years
|
8
|
26.7%
|
|
46 to 60 years
|
7
|
23.3%
|
|
>60 years
|
9
|
30.0%
|
|
Gender
|
Male
|
16
|
53.3%
|
|
Female
|
14
|
46.7%
|
|
Co-morbidities
|
Absent
|
12
|
40.0%
|
|
Present
|
18
|
60.0%
|
|
Risk factors
|
Nil
|
17
|
56.7%
|
|
Obesity
|
1
|
3.3%
|
|
Smoking
|
6
|
20.0%
|
|
Smoking and alcohol
|
6
|
20.0%
|
Majority of the subjects suffered fracture over right femur (63.3%), while remaining 36.7% exhibited left sided fracture. Muller’s Type C3 was identified as the most prevalent variant of fracture, accounting for 66.7% of cases, with knee derangement evident in 43.3% cases. The most common mode of injury was observed to be RTA (53.3%) followed by fall from height (36.7%) and workplace injury (10.0%). Only 20.0% cases showed associated injuries such as mid shaft femur fracture, tibial plateau fracture, proximal both bone fracture and metatarsal fractures (Table 2).
Table 2: Characteristics of distal end femoral fractures among the study subjects (n=30).
|
Subjects (N=30)
|
Frequency (N)
|
Percentage (%)
|
|
Laterality
|
Right
|
19
|
63.3%
|
|
Left
|
11
|
36.7%
|
|
Mullers classification
|
Type C2
|
10
|
33.3%
|
|
Type C3
|
20
|
66.7%
|
|
Knee derangement
|
Absent
|
17
|
56.7%
|
|
Present
|
13
|
43.3%
|
|
Mode of injury
|
RTA
|
16
|
53.3%
|
|
FFH
|
11
|
36.7%
|
|
WPI
|
3
|
10.0%
|
|
Associated injury
|
Absent
|
24
|
80.0%
|
|
Present
|
6
|
20.0%
|
The implants were selected based on the type and severity of the fracture, and accordingly, majority were managed with plate-plate combination (73.3%). Remaining 26.7% cases required plate-nail constructs (Figure 1).
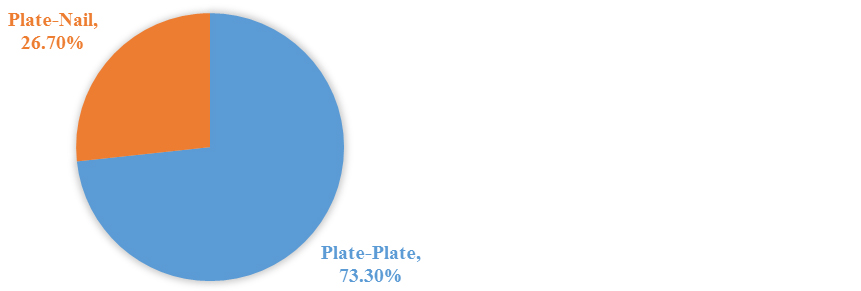
Figure 1: Type of implant used for management of distal end femoral fractures (n=30).
In about 40.0% patients, autogenous iliac bone grafting was required, for augmentation of bone healing (Figure 2).
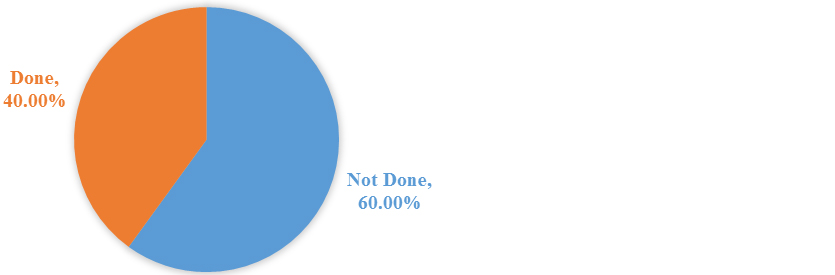
Figure 2: Requirement of autogenous iliac bone grafting among the study subjects (n=30).
In the study, the outcome of double fixation constructs i.e., both plate-plate and plate-nail combinations, was evaluated through the examination of specific parameters among the subjects during a follow-up period, including complete healing (83.3%), normal working capacity (66.7%), range of motion between 0 to 135 degrees (70.0%) (Table 3). However, about 16.7% cases suffered non-union, while 33.3% complained of reduction in their work capacities. Restricted flexion (90 to 115 degrees) was observed in 30.0% cases, while limited extension (46 to 90 degrees) occurred in about 13.3% cases (Table 3).
Table 3: Outcome of double fixation constructs for distal end femoral fractures (n=30).
|
Subjects (N=30)
|
Frequency (N)
|
Percentage (%)
|
|
Fracture union
|
Non union
|
5
|
16.7%
|
|
Healing
|
25
|
83.3%
|
|
Work capacity
|
Reduced
|
10
|
33.3%
|
|
Normal
|
20
|
66.7%
|
|
Range of motion
|
0 to 45 degrees
|
26
|
86.7%
|
|
46 to 90 degrees
|
4
|
13.3%
|
|
90 to 115 degrees
|
9
|
30.0%
|
|
116 to 135 degrees
|
21
|
70.0%
|
About 40.0% patients did not develop any complications. Among those with complications, limb length discrepancy was found in majority (43.3%), followed by valgus deformity (36.7%). The rate of superficial infections was 16.7% in our study, and all cases were treated with antibiotics (Figure 3).
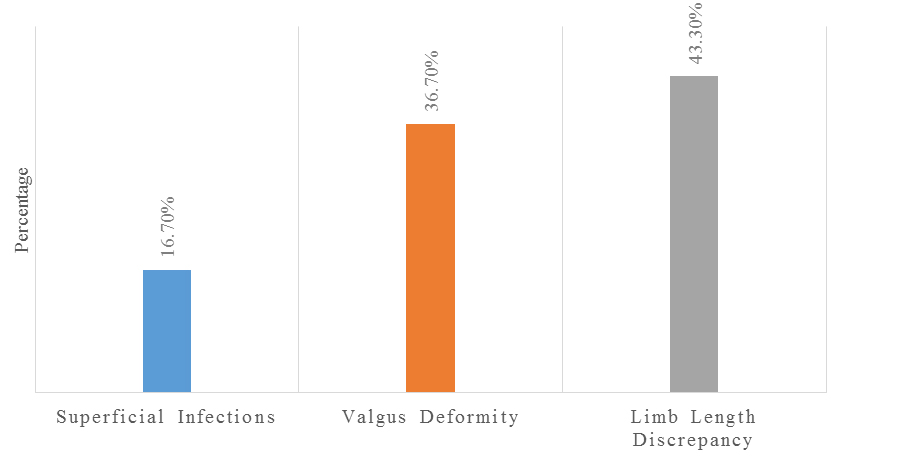
Figure 3: Complications among the study subjects (n=12).
Table 4 represents outcome in Muller’s C2 and C3 type of fracture. Complication like infection, reduction in work capacity and limb shortening was more prevalent among those who had C3 type of fracture than those who has Muller’s C2 type of fracture. Non-union and angular deformity was more among those who had C2 type of fracture than those who had Muller’s C3 type. But all these differences were not statistically significant.
Table 4: Outcome in Muller’s C2 and C3 type of fracture (n=30).
|
Muller’s type of fracture
|
Infection present
|
Work capacity reduced
|
Non union
|
Shortened limb
|
Angular deformity present
|
|
C2 (n=11 100%)
|
1(9.09%)
|
3 (27.3%)
|
2(18.2%)
|
3 (27.3%)
|
6 (54.6%)
|
|
C3 (n=19 100%)
|
3 (15.8%)
|
6 (31.6%)
|
3 (15.8%)
|
10
|
6 (33.3%)
|
|
Chi-square value
|
0.233
|
0.033
|
0.049
|
0.1
|
0.749
|
|
p- value
|
1
|
0.8
|
1
|
1.688
|
0.3
|
Table 5 represents mean degree of flexion and extension. Mean extension was statistically significantly lower in C3 type of fracture than in C2 type of fracture.
Table 5: Range of movement in Muller’s C2 and C3 type of fracture (n=30).
|
Muller’s type of fracture
|
Flexion (mean in degrees)
|
Extension after flexion (mean in degrees)
|
|
C2
|
121.30
|
42
|
|
C3
|
121.61
|
31.67
|
|
t value
|
- 0.069
|
2.193
|
|
p value
|
0.945
|
0.03*
|
Table 6 represents outcome in two types of implants. Complication like infection, non-union and limb shortening was more prevalent among those who had plate-nail implant than those who had plate-plate implant. Non-union and reduced work capacity were more among those who had plate-plate implant than those who had plate-nail implant. But all these differences were not statistically significant.
Table 6: Outcome in two types of implants (n=30).
|
Type of implant used
|
Infection
|
Work capacity reduced
|
Non union
|
Shortened limb
|
Angular deformity present
|
|
Plate nail (n=9 100%)
|
2 (22.2%)
|
1 (11.1%)
|
3 (33.3%)
|
6 (66.7%)
|
3 (33.3%)
|
|
Plate plate (n=21 100%)
|
2 (9.5%)
|
8 (38.1%)
|
2 (9.5%)
|
8 (38.1%)
|
8 (38.1%)
|
|
Chi-square value
|
1.05
|
1.981
|
2.946
|
1.163
|
0.015
|
|
p- value
|
0.55
|
0.21
|
0.12
|
0.41
|
1
|
Table 7 represents mean degree of flexion and extension. There was no statistically significant difference between Mean degrees of extension and flexion among those who had plate-nail and plate-plate implant.
Table 7: Mean degree of flexion and extension for two different types of implants (n=30).
|
Type of implant used
|
Flexion (mean in degrees)
|
Extension (mean in degrees)
|
|
Plate nail
|
122.50
|
34.38
|
|
Plate-plate
|
121.10
|
35.75
|
|
t value
|
0.295
|
-0.253
|
|
p value
|
0.7
|
0.8
|
Discussion
Our comprehensive study delved into the clinical outcomes of dual implantation surgery for distal femur fractures by meticulously analyzing records from 30 patients. The study primarily focused on elucidating the demographic characteristics, injury patterns, fracture types, and treatment outcomes in order to contribute valuable insights to the existing body of literature on this intricate surgical procedure.
A notable demographic trend emerged from our study, with a significant proportion (30.0%) of the patient cohort being above 60 years of age. This aligns with the observations of several prior studies, including notable works by Kanabur [12], Hussain [13], Liporace [14], and Garala [15], which consistently identified a higher incidence of distal femur fractures among the elderly population. The prevalence of such fractures in older individuals underscores the importance of tailored interventions for this demographic.
In our study, a clear male predominance was evident, with a male-to-female ratio of 53.3:46.7. This finding resembles the results of a study by Khalil et al [16], which reported a similar gender distribution (66.7:33.3). Nevertheless, contrasting ratios were observed in study done Passias et al [17] (43.2:56.8), highlighting the variability in gender distribution across different research cohorts.
The analysis of the mode of injury revealed that RTA constituted the most common cause (53.3%) of distal femur fractures in our study, corroborating the universal trend identified in studies by Attum et al [18], Hussain et al [13], Passias et al [17]. This emphasizes the significance of preventive measures and targeted interventions to mitigate the impact of RTAs on distal femur fractures.
Muller’s type C3 emerged as the predominant fracture variant in our study, constituting 66.7% of cases. This aligns with the findings of studies by Khalil et al [16], Kontakis et al [19] suggesting a consistent prevalence of this fracture type across diverse populations.
In terms of surgical management, our study revealed a preference for plate-plate combination (73.3%) in the majority of cases, with plate-nail constructs employed in the remaining 26.7%. The success of the procedure was evident in favorable outcomes, including high rates of complete healing (83.3%), normal working capacity (66.7%), and satisfactory ranges of motion in flexion (70.0%) and extension (86.7%). These outcomes resonate with positive results reported in studies by Khalil et al [16], Park et al [20], Tripathy et al [21] Stoffel [22], supporting the efficacy of dual implantation surgery.
Despite these positive trends, a subset of cases experienced complications, including non-union in 16.7% and reduced work capacity in 33.3%. This underscores the need for continued refinement of the surgical technique and vigilant postoperative monitoring. Nonetheless, the overall safety of the procedure was reinforced by minimal complications reported in studies such as Attum et al [18], Hussain et al [13], Tripathy et al [21], and Passias et al [17].
Limitations: The possibility of delayed healing because to excessive build stiffness is another significant worry with twin implants. This data was collected in tertiary care centre in limited patients, multi-centre with more patients gives precise results.
Conclusion
Distal end femur fracture is a highly complicated fracture and need the most stable fixation and highly invasive approach to facilitate anatomical reconstruction of Muller’s type-C2 and C3. Using dual implants like dual plate or plate with nail can achieve good clinical outcome with acceptable knee range of motion, good union rates, and best reconstruction of supra patella area for the knee joint articulation with less complications. So, we conclude that dual implants can be considered as a standard procedure for managing these complex injuries.
Acknowledgement
We sincerely thank the faculty of the institute for helping us in each aspect of the study.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Ehlinger M, Ducrot G, Adam P, Bonnomet F. Distal femur fractures. Surgical techniques and a review of the literature. Orthop Traumatol Surg Res. 2013; 99:353–360.
[2] Elsoe R, Ceccotti AA, Larsen P. Population-based epidemiology and incidence of distal femur fractures. Int Orthop. 2018; 42:191–196.
[3] Zlowodzki M, Bhandari M, Marek DJ, Cole PA, Kregor PJ. Operative treatment of acute distal femur fractures: systematic review of 2 comparative studies and 45 case series (1989 to 2005). J Orthop Trauma. 2006; 20:366–371.
[4] Martinet O, Cordey J, Harder Y, Maier A, Bühler M, et al. The epidemiology of fractures of the distal femur. Injury. 2000; Supp 3:C62–C63.
[5] Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review Injury. 2006; 37:691–697.
[6] Arneson TJ, Melton LJ, Lewallen DG, O'Fallon WM. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965-1984. Clin Orthop Relat Res. 1988; 234:188–194.
[7] Sanders R, Swiontkowski M, Rosen H, Helfet D. Double-plating of comminuted, unstable fractures of the distal part of the femur. J Bone Joint Surg Am. 1991; 73:341–346.
[8] Moore TJ, Watson T, Green SA, Garland DE, Chandler RW. Complications of surgically treated supracondylar fractures of the femur. J Trauma. 1987; 27:402–406.
[9] Ehlinger M, Ducrot G, Adam P, Bonnomet F. Distal femur fractures. Surgical techniques and a review of the literature. Orthop Traumatol Surg Res. 2013; 99:353–360.
[10] Onizuka N, Farmer S, Wiseman JM, Alain G, Quatman-Yates CC, et al. Timing of complications following surgery for distal femur fractures in older adults. Geriatr Orthop Surg Rehabil. 2023; 16:14:21514593231195539.
[11] Seo JH, Lee BS, Kim JM, Kim JJ, Kim JW. Outcomes of dual plating for unstable distal femoral fractures: a subgroup comparison between periprosthetic and non-periprosthetic fractures. Int Orthop. 2022; 46:2685–2692.
[12] Kanabar P, Kumar V, Owen PJ, Rushton N. Less invasive stabilisation system plating for distal femoral fractures. J Orthop Surg. 2007; 15:299–302.
[13] Hussain MS, Dailey SK, Avilucea FR. Stable fixation and immediate weight-bearing after combined retrograde intramedullary nailing and open reduction internal fixation of noncomminuted distal interprosthetic femur fractures. J Orthop Trauma. 2018; 32:e237–e240.
[14] Liporace FA, Yoon RS. Nail plate combination technique for native and periprosthetic distal femur fractures. J Orthop Trauma. 2019; 33:e64–e68.
[15] Garala K, Ramoutar D, Li J, Syed F, Arastu M, et al. Distal femoral fractures: a comparison between single lateral plate fixation and a combined femoral nail and plate fixation. Injury. 2022; 53:634–639.
[16] Khalil AS, Ayoub MA. Highly unstable complex C3-type distal femur fracture: can double plating via a modified Olerud extensile approach be a standby solution? J Ortho Traumatol, 2012; 13:179–188.
[17] Passias BJ, Emmer TC, Sullivan BD. Treatment of distal femur fractures with a combined nail-plate construct: techniques and outcomes. J Long Term Eff Med Implants. 2021; 31:15–26.
[18] Attum B, Douleh D, Whiting PS, White-Dzuro GA, Dodd AC, et al. Outcomes of distal femur nonunions treated with a combined nail/plate construct and autogenous bone grafting. J Orthop Trauma. 2017; 31:e301–e304.
[19] Kontakis MG, Giannoudis PV. Nail plate combination in fractures of the distal femur in the elderly: A new paradigm for optimum fixation and early mobilization? Injury. 2023; 54:288–291.
[20] Park KH, Oh CW, Park IH, Kim JW, Lee JH, et al. Additional fixation of medial plate over the unstable lateral locked plating of distal femur fractures: A biomechanical study. Injury. 2019; 50:1593–1598.
[21] Tripathy SK, Mishra NP, Mishra NP. Dual-plating in distal femur fracture: A systematic review and limited meta-analysis. Indian J Orthopaed. 2022; 56:183–207.
[22] Stoffel K, Sommer C, Lee M, Zhu TY, Schwieger K, et al. Double fixation for complex distal femur fractures. Effort Open Rev. 2022; 7:274–286.