Abstract
Background: Paediatric septicemia causes significant global morbidity and mortality, particularly in resource-poor regions. The knowledge of microbiological profile of sepsis in children is utmost important to guide the treatment. This study aims to investigate the prevalent pathogens and their antimicrobial susceptibility pattern in cases of pediatric sepsis in a tertiary care hospital.
Material and methods: In this cross-sectional study, a total of 321 Blood culture samples (BACTEC bottles) were collected from suspected sepsis patients aged 1 month to 18 years, admitted in the pediatric wards & intensive care units. The BACTEC bottles which flagged positive were inoculated on culture media and was further processed according to standard microbiological procedures. Antimicrobial susceptibility was done by using Kirby Bauer disc diffusion method as per Clinical Laboratory Standards Institute (CLSI) guidelines 2024. All the data was entered in excel sheet and analysed by using SPSS 23.0 software.
Results: A total of 321 blood culture samples were collected from children aged >1month to 18 years, admitted in wards and PICU. The overall positivity rate of blood culture samples was 29%. Staphylococcus aureus (56%) was found to be the predominant pathogen followed by CoNS (21.5%), E. coli (5.4%), Acinetobacter spp. (4.3%), Candida spp. (4.3%), Klebsiella spp. (3.2%), Enterococcus spp. (3.2%) and Pseudomonas spp. (2.1%). S. aureus isolates showed high susceptibility towards vancomycin (100%), linezolid (94.9%) and minocycline (97.4%) and low susceptibility towards fluoroquinolones (38.5%) and erythromycin (28.2%). Methicillin resistance was found in 41.5% S. aureus isolates. Gram negative isolates showed fair sensitivity towards colistin, carbapenems and minocycline while poor sensitivity was found towards amoxycillin clavulanate, cephalosporins and fluoroquinolones.
Conclusion: This study provides crucial information about the incidence, risk factors, prevailing pathogens causing pediatric sepsis and their changing antimicrobial trend which is required to formulate empirical treatment guidelines for better patient outcome.
Keywords: antimicrobial; susceptibility; blood culture; morbidity; sepsis
Full Text
Introduction
Sepsis is a clinical condition representing a dysregulated host reaction in response to severe infection. This uncontrolled and self-sustaining inflammatory cascade can lead to end organ dysfunction and rapidly progress to shock and multiple organ failure [1, 2]. If sepsis is not treated appropriately and timely, death can occur due to refractory shock, multiple organ dysfunction syndrome (MODS), respiratory failure and/or neurological failure [1, 2].
Sepsis continues to be a major public health concern and a leading cause of morbidity and mortality in developing countries like India, despite the widespread universal immunization program, standard treatment guidelines and improved intensive care techniques [3]. Sepsis affects all the age groups with relatively higher incidence in early childhood and older populations. Approximately 50 million people worldwide suffer from sepsis annually, among which children constitute half the proportion. A recent report suggests an estimated incidence of paediatric sepsis as 1.2 million cases per year which accounts for > 8% of all pediatric intensive care unit admissions with mortality ranging from 1- 20% depending upon the severity of sepsis [1, 3].
Early identification of sepsis in children is challenging owing to the non-specific clinical presentation that cannot differentiate sepsis from other more common febrile illnesses prevalent in this age group [4]. Moreover, physiology of children compensates and masks characteristic manifestations of sepsis until they land in shock. Frequent risk factors associated with pediatric sepsis are indwelling devices, malignancy, bone marrow or organ transplantation, and underlying chronic diseases [3, 4]. Etiological agents causing sepsis differ among previously healthy children and children with risk factors. Staphylococcus aureus is the most frequent pathogen implicated as a causative agent in sepsis both in healthy and children with chronic conditions. The other common organisms causing sepsis in healthy children are Escherichia coli and Streptococcus pneumoniae while Candida spp. and Pseudomonas spp. are common in children with chronic diseases [1, 3, 5].
Paediatric sepsis has considerable impact on children in form of increased morbidity and long-term sequelae. Often survivors of pediatric sepsis show eventual consequences even after hospital discharge such as cognitive, physical or development impairment [1, 3, 6]. In addition, pediatric sepsis imposes high economic burden on healthcare systems as well as on affected families and communities. The severity and significant mortality rate of this condition underscores it as a substantial challenge for health care system especially in developing countries [1, 3]. Early identification of pediatric sepsis requires high degree of clinical suspicion and vigilance. Any undue delay in initiation of the treatment can be fatal. Prognosis of children affected by sepsis relies on timely diagnosis and prompt initiation of appropriate empirical treatment. Hence, in suspected cases of sepsis, empirical antibiotic therapy should be started immediately with subsequent escalation or de-escalation of antimicrobials as per culture and sensitivity report. For judicious selection of empirical antibiotics, clinicians need to refurbish their knowledge of prevalent microorganisms causing childhood sepsis and their antibiogram in order to attain better patient outcome.
The spectrum of organisms causing pediatric sepsis varies over time and from region to region. Regular epidemiological studies about etiological agents and their antibiogram serve as a useful tool for selecting appropriate empirical as well as definitive antimicrobial therapy. There are limited studies and paucity of data available on the microbiological profile of pediatric sepsis in our region. So, this study was undertaken to bridge the gap in our knowledge about circulating pathogens of pediatric sepsis and their local antibiotic susceptibility pattern.
Materials and methods
This cross-sectional study was conducted in the department of Microbiology at Rohilkhand Medical College and Hospital from January 2024 to December 2024, after clearance from the institutional ethics committee. Informed consent was taken from guardians of each study participant. A total of 321 blood culture samples (BACTEC bottles) were collected from suspected sepsis patients aged 1 month to 18 years, admitted in the pediatric wards & intensive care units, following proper aseptic precautions. Neonates and children who were already on antibiotics were excluded from the study. A 3-5 ml blood sample was collected from each patient by peripheral venipuncture in BACTEC pediatric blood culture bottle, before initiation of antibiotics. The BACTEC bottles which flagged positive were inoculated on Blood agar and Mac Conkey agar and plates were incubated at 37° C overnight. Culture colonies obtained were identified by standard microbiological procedures [7]. Antimicrobial susceptibility was done by using Kirby Bauer disc diffusion method as per Clinical Laboratory Standards Institute (CLSI) guidelines 2024 [8]. All the data was entered in excel sheet and analysed by using SPSS 23.0 software.
Results
A total of 321 blood culture samples were collected during the study period, from children aged >1month to 18 years, admitted in wards and pediatric intensive care unit (PICU). Most of the suspected sepsis cases were infants and toddlers (130/321) (Table 1).
Table 1: Demographic profile of suspected pediatric sepsis cases.
|
Age group
|
Gender
|
|
Male - N (%)
|
Female - N (%)
|
|
1 month- 11 months
|
36 (58)
|
26 (41.9)
|
|
1- 5 years
|
46 (67.6)
|
22 (32.3)
|
|
6-10 years
|
32 (61.5)
|
20 (38.4)
|
|
>10 years
|
67 (48.2)
|
72 (51.7)
|
|
Total
|
181 (56.3)
|
140 (43.6)
|
The overall positivity rate of blood culture samples was 29%. The blood culture positivity was marginally higher in males than females (56.3%) (Figure 1).
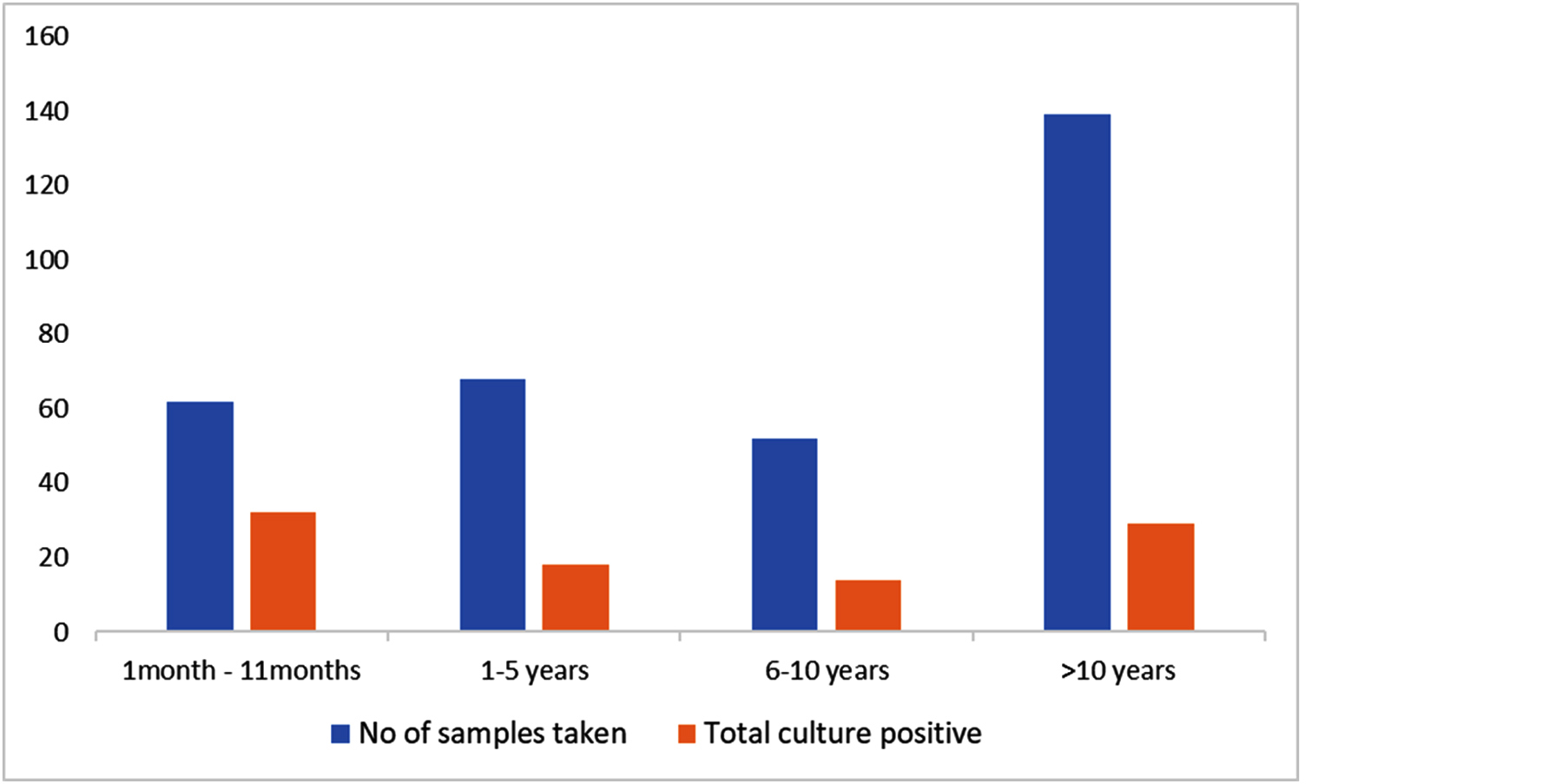
Figure 1: Distribution of positive blood culture samples in various age groups.
A substantial number of positive blood culture samples showed growth of Gram- positive cocci (81%), with Staphylococcus aureus (56%) being the predominant pathogen followed by coagulase negative Staphylococcus spp (CoNS) (21.5%). Among Gram- negative bacteria (21.5%), 14 isolates were enteric coliforms while 6 isolates were non-fermenters. Candida spp. were identified as the causative agent in 4.3% cases (Figure 2).
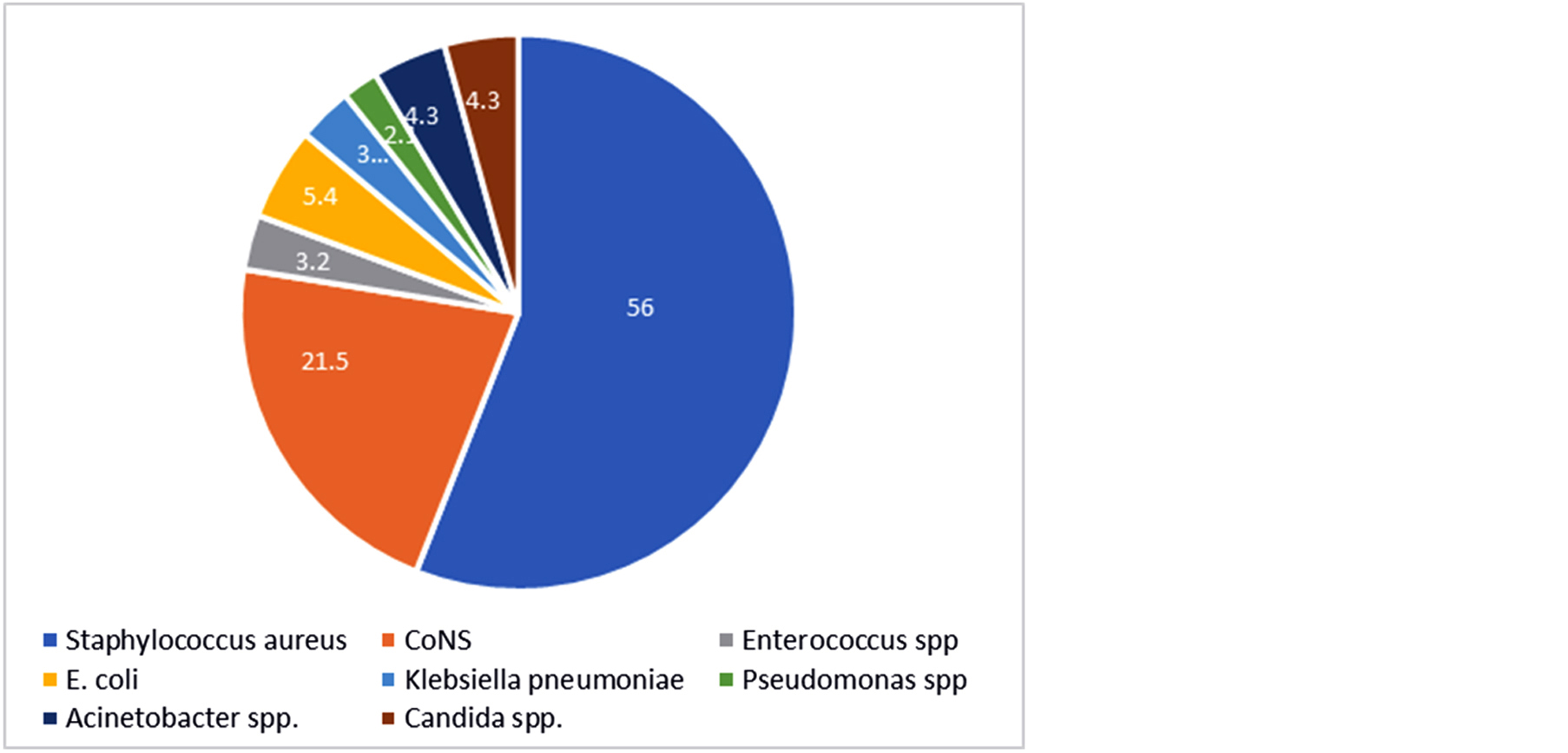
Figure 2: Organism- wise distribution of test isolates.
S. aureus isolates showed remarkable susceptibility towards vancomycin (100%), linezolid (94.9%), doxycycline (94.9%), minocycline (97.4%) and low susceptibility towards fluoroquinolones (38.5%), penicillin (12.8%) and erythromycin (28.2%). Among S. aureus isolates 41.5% isolates were found to be methicillin resistant Staphylococcus aureus (MRSA). Similarly, CoNS also showed high sensitivity towards vancomycin (100%), linezolid (87.9%), doxycycline (90.9%), minocycline (100%) while lower susceptibility was found for fluoroquinolones, penicillin, clindamycin and erythromycin. CoNS isolates exhibited higher resistance against cefoxitin depicting more methicillin resistance in CoNS as compared to S. aureus. All Enterococcus isolates were found to be sensitive to vancomycin, linezolid, high level gentamycin and erythromycin (Figure 3).
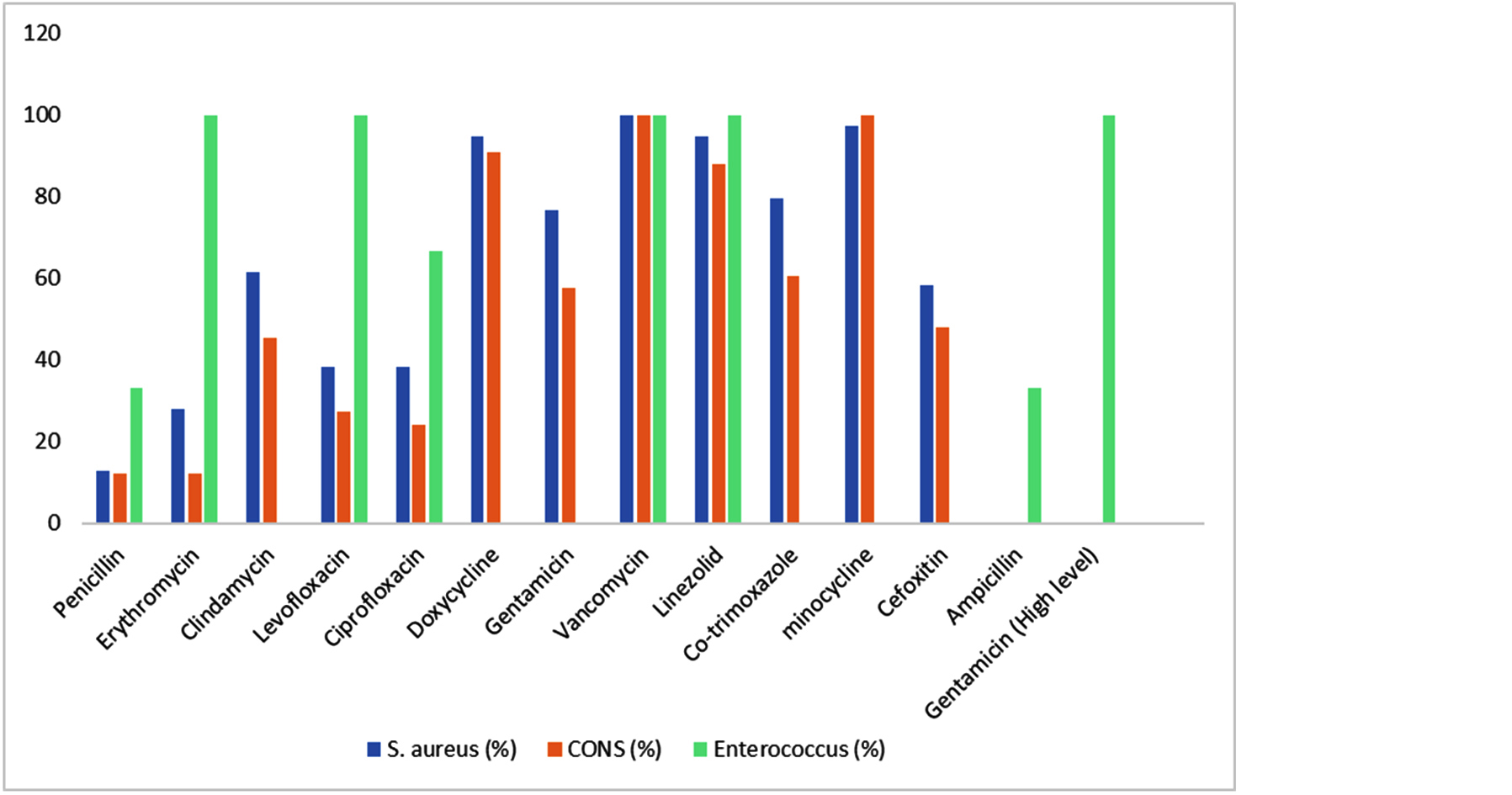
Figure 3: Susceptibility (%) of Gram- positive isolates to various antimicrobials.
E. coli and Klebsiella spp. isolates depicted remarkable sensitivity towards colistin and tetracycline. Additionally, E. coli also exhibited higher sensitivity for carbapenems, minocycline, gentamicin and tobramycin. Both, E. coli and Klebsiella spp. isolates showed poor sensitivity towards amoxycillin- clavulanate, piperacillin- tazobactam, cephalosporins and fluoroquinolones. Among non-fermenters, Pseudomonas aeruginosa isolates showed high sensitivity towards, colistin, piperacillin- tazobactam, amikacin and cefepime while Acinetobacter spp. showed fair susceptibility for carbapenems, aminoglycosides, minocycline and colistin. Both non fermenters showed poor sensitivity against cephalosporins and fluoroquinolones (Figure 4).
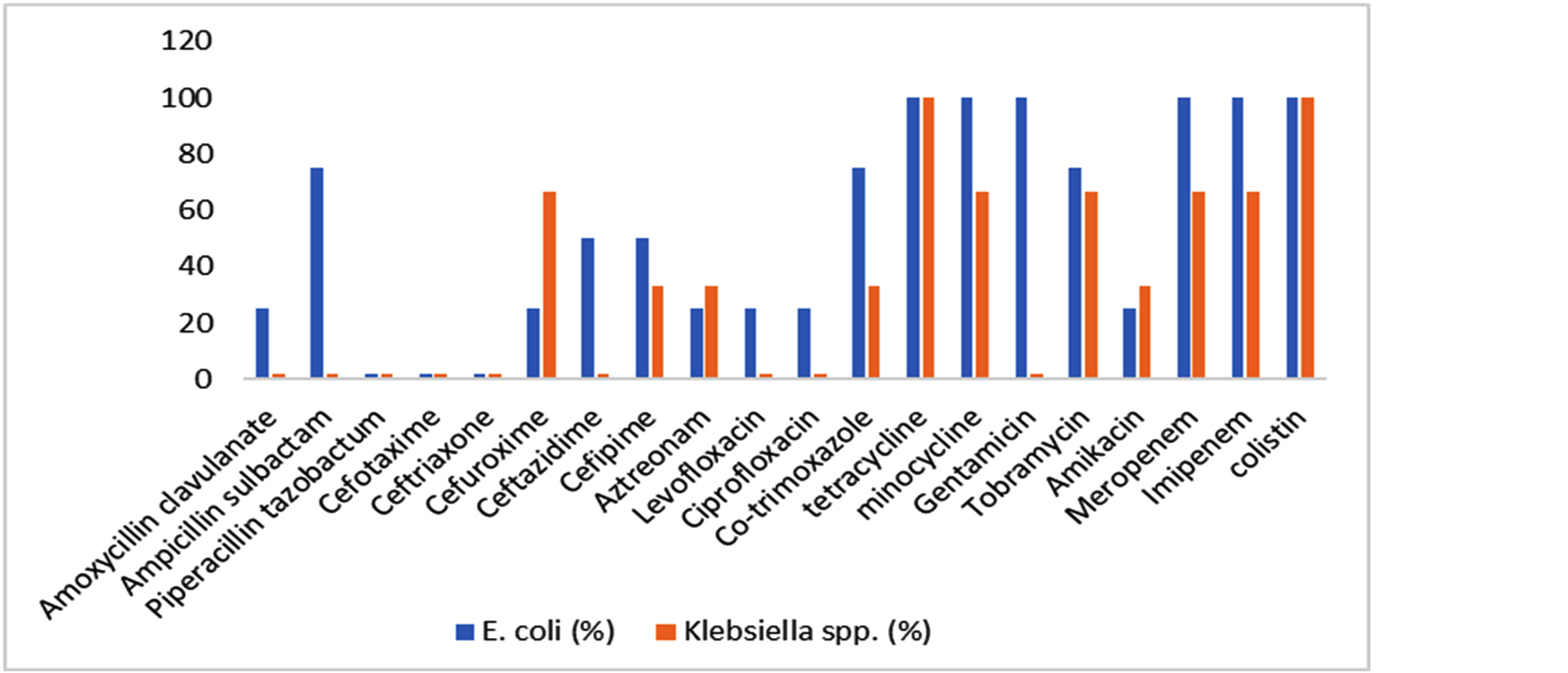
Figure 4: Susceptibility (%) of Gram- negative isolates to various antimicrobial agents.
Discussion
In our study, we have observed an overall blood culture positivity rate of 29% in suspected cases of pediatric sepsis patients. Chaitra et al and Sharma et al [9, 10] also reported similar blood culture positivity rate while Mehta et al [11] and Biswas et al [12] observed far higher positivity rate in their studies. We have found that a significant portion of the study population was comprised by infants and toddlers (130/321) in which blood culture positivity rate (38.5%) was also considerably higher as compared to other age groups. This finding was concordant with most studies [10, 12]. The humoral and cellular immune response of infants and younger children are not well developed as compared to adolescents and adults, making them more susceptible for infections.
In the present study, most prevalent isolate was S. aureus (56%) which was similar to various studies conducted in different parts of India and worldwide, that also reported S. aureus to be the main etiological agent of sepsis in patients admitted in pediatric wards and ICU. CoNS was isolated in 21.5 % blood culture samples and similar findings were reported by Chaitra et al, Mehta et al and Kumari et al. [9, 11, 13]. It is usually considered as a skin commensal but can be pathogenic in susceptible patients which necessitates judicious reporting of CoNS based on isolation from paired blood culture samples along with clinical correlation of the patients. Gram- negative isolates were obtained from 15.1% samples which included E. coli (5.4%), Klebsiella spp. (3.2%), Pseudomonas spp. (2.1%) and Acinetobacter spp. (4.3%). Concordant results were shown by Chaitra et al, Sharma et al and Biswas et al [9, 10, 12]. Conversely, Khan et al found that Gram- negative isolates were more prevalent as causative agents of pediatric sepsis than Gram- positive isolates [14].
In our study, linezolid and vancomycin have emerged as most effective antibiotics towards Gram- positive isolates. Apart from these reserved classes of drugs, Gram- positive bacteria were also found to be fairly susceptible to doxycycline and minocycline. Similar results were shown by Chaitra et al, Biswas et al and Khan et al. [9, 12, 14]. We have found methicillin resistance in 41.5% S. aureus isolates which is comparable to data provided by Mehta et al and Biswas et al [11, 12] in their studies.
Majority of Gram- negative isolates were found susceptible to colistin, carbapenems and minocycline. In our study, we have observed more multidrug resistance in Klebsiella isolates than Pseudomonas and Acinetobacter isolates. Comparable susceptibility pattern of Gram- negative bacteria isolated from sepsis patients was shown by Sharma et al and Kumari et al [10, 13]. This study demonstrates high resistance to commonly prescribed antimicrobials like cephalosporins, fluoroquinolones and amoxycillin- clavulanic acid, similar to other studies depicting injudicious overuse of these drugs both in clinical settings as well as over the counter [1]. We have also found 4 Candida isolates which showed good susceptibility to azoles and amphotericin B. For the appropriate management of pediatric sepsis patients timely initiation of empirical antimicrobials is a must which in turn depends on updated knowledge about local prevalent etiological agents and their susceptibility to various antibiotics. So, the data acquired from such studies may guide the clinicians to start appropriate antibiotics while waiting for culture report.
The limitations of this study were the small sample size and inclusion of patients from a single tertiary care hospital. While, this institutional study offers valuable insights into local trends, large-scale multicentric research is essential to develop effective, evidence-based treatment guidelines for pediatric sepsis.
Conclusion
Even in the era of advanced medical techniques and universal vaccination, sepsis continues to be a substantial cause of morbidity and mortality in pediatric population especially in children under 5 years. In our study, blood culture positivity was considerably high and S.aureus was found as the predominant pathogen isolated from study population. The antimicrobial susceptibility pattern of various etiological agents was also determined in this study which provides valuable data for appropriate management of pediatric sepsis cases.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Watson RS, Carrol ED, Carter MJ, Kissoon N, Ranjit S, et al. The burden and contemporary epidemiology of sepsis in children. Lancet Child Adolesc Health. 2024; 8:670–681.
[2] Massaud-Ribeiro L, Silami PHNC, Lima-Setta F, Prata-Barbosa A. Pediatric sepsis research: where are we and where are we going? Front Pediatr. 2022; 10:829119.
[3] Dharmapalan D, Shet A, Yewale V, Sharland M. High reported rates of antimicrobial resistance in Indian neonatal and pediatric bloodstream infections. J Pediatric Infect Dis Soc. 2017; 6:e62.
[4] Bracken A, Lenihan R, Khanijau A, Carrol ED. The aetiology and global impact of paediatric sepsis. Curr Pediatr Rep. 2023; 11:204–213.
[5] Pedro TDA C, Morcillo AM, Baracat EC. Etiology and prognostic factors of sepsis among children and adolescents admitted to the intensive care unit. Rev Bras Ter Intensiva. 2015; 27:240–246.
[6] Miranda M, Nadel S. Pediatric sepsis: a summary of current definitions and management recommendations. Curr Pediatr Rep. 2023; 11:29–39.
[7] Indian Council of Medical Research. Standard Operation Procedures, Bacteriology. New Delhi: Indian Council of Medical Research; 2019. Accessed December 22, 2024, Available from: http://icmr.nic.in/Publications/SOP/SOP_Bacteriology.pdf.
[8] Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing. CLSI Supplement M100. 34th ed. Wayne, PA: CLSI; 2024.
[9] Chaitra KM, Anil H, Varshini P, Agrawal A, Talewad SL. Study on etiological organisms in a suspected case of sepsis in the children admitted to paediatric intensive care unit. Int J Contemp Pediatr. 2019; 6:1609–1613.
[10] Sharma S, Suda A, Uppal B. Antimicrobial resistance in pediatric sepsis: a study from a tertiary care hospital in North India. Int J Curr Res Aca Rev. 2018; 6:7–13.
[11] Mehta A, Gupta R, Ajmariya M. Microbiological profile of pediatric sepsis in a tertiary care teaching hospital of Central India. SVU-IJMS. 2022; 5:90–104.
[12] Biswas PP, Akhter K, Sen A, Umesh, Chand MIA. Bacteriological profile and antibiogram of blood culture isolates from septicaemic neonates and children up to 10 years of age, in a tertiary care centre of eastern Bihar in India. J Evid Based Med Healthc. 2021; 8:882–887.
[13] Kumari K, Mahato R, Anand C, Kumar S. Bacteriological profile and antibiotic resistance pattern in systemic infection in children. Int J Health Clin Res. 2021; 4:128–231.
[14] Khan MS, Kareem A, Fatima K, Rauf S, Khalid A, et al. Microbial patterns and antibiotic susceptibility in blood culture isolates of septicemia suspected children in the pediatrics ward of a tertiary care hospital. J Lab Physicians. 2021; 13:64–69.