Orginal Research
2023
September
Volume : 11
Issue : 3
Functional outcome of rotating platform total knee arthroplasty - A prospective observational study
Kavalakkatt K, Roy ASS, Shibu R, Dhrushith EP, Suseelan A, Biju S
Pdf Page Numbers :- 204-209
Kevin Kavalakkatt1, Shyam Roy AS1, Shibu R1, Dhrushith EP1, Akhil Suseelan1, and Biju S1,*
1Department of Orthopaedics, Government Medical College, Thiruvananthapuram, Kerala-695011, India
*Corresponding Author: Dr. Biju S, Associate Professor Orthopaedics, Government Medical College, Thiruvananthapuram, Kerala-695011, India. Email: sb19780119@gmail.com
Received 25 April 2023; Revised 13 June 2023; Accepted 22 June 2023; Published 30 June 2023
Citation: Kavalakkatt K, Roy ASS, Shibu R, Dhrushith EP, Suseelan A, Biju S. Functional outcome of rotating platform total knee arthroplasty - A prospective observational study. J Med Sci Res. 2023; 11(3):204-209. DOI: http://dx.doi.org/10.17727/JMSR.2023/11-38
Copyright: © 2023 Kavalakkatt K et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Rotating platform (RP) is a form of mobile-bearing design for total knee arthroplasty (TKA). This reduces the polyethylene contact stresses and the forces acting on tibial component and bone cement interfaces. It increases the femoral roll-back and flexion. The objective was to assess the functional outcome of rotating platform design in primary TKA, in patients with osteoarthritis of knee and the association of age and gender with the outcome.
Materials and methods: A prospective observational study was done on 42 patients who underwent primary TKA with RP design and followed-up for one year. The outcome was assessed with the Knee Society Score at one year. Data analysis was done using statistical package SPSS V-27.0.
Results: The mean age was 64.33(±6.12). The mean pre-op knee clinical score was 30(±6.409), which improved to mean post–op score of 92.17(±5.53). 37(88.1%) had excellent and 5(11.9%) had good results. 7(70%) patients in the age group <60 years, 24(96%) cases of 60–69 years and 6(85.7%) cases of ≥70 years had excellent results. 23(95.8%) females and 14(77.8%) males had excellent knee clinical scores. The mean pre-op knee functional score was 33.81(±9.988), which improved to a mean post–op score of 82.38(±6.917). 36 cases (85.7%) had excellent and 6(14.3%) had good results. 7(70%) patients <60 years, 22(88%) of 60- 69 years and 7(100%) of ≥70 years had excellent results. 21(87.5%) females and 15(83.3%) males had excellent knee functional scores.
Conclusion: Total knee arthroplasty with rotating platform design has shown excellent clinical and functional outcome without any serious complications at one year follow-up.
Keywords: total knee arthroplasty; functional outcome; rotating platform design; knee scoring system
Full Text
Introduction
Osteoarthritis is the most common form of arthritis in the elderly. It is more common in knee than in hip or ankle [1]. Drugs, physiotherapy and life style modifications can relieve pain to some extent but cannot cure the underlying pathology. Total knee arthroplasty (TKA) is the treatment of choice for severe osteoarthritis knee, which relieves the joint pain and improve the joint function. TKA also corrects deformity and have more than 90% survival rate after 15 years [2]. Mechanical alignment has been used in TKA for more than 3 decades. Hip- knee- ankle less than 3º to mechanical axis is required for a good outcome. Regaining closer-to-normal knee mechanics results in fewer revision rates and improved outcomes [3]. Cemented TKA remains the gold standard procedure with successful long-term outcome [4]. Preoperative range of motion affects the postoperative range of motion and should be considered during planning of TKA. Posterior cruciate retaining designs showed comparable results of functional outcome, range of motion and complications to cruciate substituting designs [5]. Computer assisted TKA offered no advantage in function, survivorship, or quality of life over conventional technique [6].
The two types of bearing designs for TKA are fixed-bearing and mobile-bearing designs. The fixed-bearing design results in high contact stress between femoral and tibial surfaces which results in polyethylene wear and fixation failure. This lead to the concept of mobile-bearing (MB) design. The MB design TKA was first developed as meniscal bearing concept and later modified to rotating platform (RP) design. The RP design reduces the polyethylene contact stresses and reduces the forces acting on tibial component and bone cement interfaces [7]. The rolling curvilinear motion is dissociated from the transverse axial rotation motion onto two articulating surfaces. These leads to decreased wear and aseptic loosening. Polyethylene movement relative to tibial tray increases the femoral roll-back and flexion, thereby improving the range of movement and knee function [7, 8].
There are various mobile-bearing designs, differing in their mobility [9]. The meniscal bearing designs mimic meniscus with independent movements of medial and lateral bearings. The anteroposterior glide and rotation designs allow gliding in anteroposterior plane and minimal rotation about central axis of tibia. The RP design allows free rotation of tibial polyethylene insert about central axis of tibia. There are many articles relating to mobile bearing design in literature [4, 8, 10]. Very few studies have been documented specifically for rotating platform design [11]. The purpose of this study was to assess the functional outcome of rotating platform design of TKA in patients with osteoarthritis of knee. Also to assess the association of age and gender with the functional outcome of RP design TKA.
Materials and methods
A prospective observational study was done on 42 consecutive patients who underwent primary TKA with RP design at Department of Orthopaedics, Government Medical College, Thiruvananthapuram during the period December 2020 to May 2022, after institutional ethics committee clearance (HEC No: 07/77/2020/MCT). All the patients who satisfied the inclusion and exclusion criteria, and who gave informed written consent were included in the study.
Inclusion criteria: diagnosed osteoarthritis knee patients who underwent RP design TKA who were available for a minimum follow up of 12 months, who gave written informed consent, patients undergoing both unilateral and bilateral TKA. Exclusion criteria: patients who had previous knee surgery, patellectomy or high tibial osteotomy; patients with a history of septic arthritis and rheumatoid arthritis; patients who had flexion contracture > 20o or valgus deformity >15o or varus deformity >20o and patients requiring revision TKA.
Surgical technique
Authors used Buechel-Pappas™ primary knee system CoCr (Rotating Platform) knee implant for all the surgeries. Under epidural anaesthesia and strict aseptic precautions, knee joint exposed through a medial parapatellar incision after inflating tourniquet. A medial soft tissue release was performed from the medial proximal tibia for fixed varus deformity. Symmetric and balanced flexion-extension gaps were obtained by Gap balancing technique. Upper tibial resection done using tibial resection guide. A femoral guide is used for drilling a hole into the femoral intramedullary canal, the entry portal being a point anterior to origin of posterior cruciate ligaments just medial to midline. Intramedullary rod is inserted into the femoral shaft. The A-P femoral resection guide is fixed with 2 pins and anterior and posterior femoral resections done. Flexion tension and alignment checked with spacer block and releases done if necessary, for equal medial and lateral gaps. The distal femoral resection guide is placed and the distal femoral resection done, with the resection angle being the difference between the mechanical and anatomical axis of femur. Extension gap (Figure 1a) and limb alignment checked using spacer block. The extension gap must be same as the flexion gap. Finishing guide is placed and anterior and posterior chamfer cuts done. The appropriate size tibial reamer guide template is placed and hole for tibial stem reamed. Tibial trial component and trial polyethylene is inserted. Knee flexed to 120° and trial femoral component placed (Figure 1b). Patella is reduced and patella tracking evaluated. Patellar osteophytes removed and denervation of patella performed with electrocautery. The appropriate tibial and femoral components implanted using antibiotic impregnated bone cement. Adequate range of motion (Figures 1c,d), free bearing movement and proper patella tracking were ensured. Tourniquet released and saline irrigation done. Watertight closure of deep retinacular tissues done after keeping suction drain and attaining haemostasis. Staples used for skin closure. Compression dressing and knee immobilizer applied.
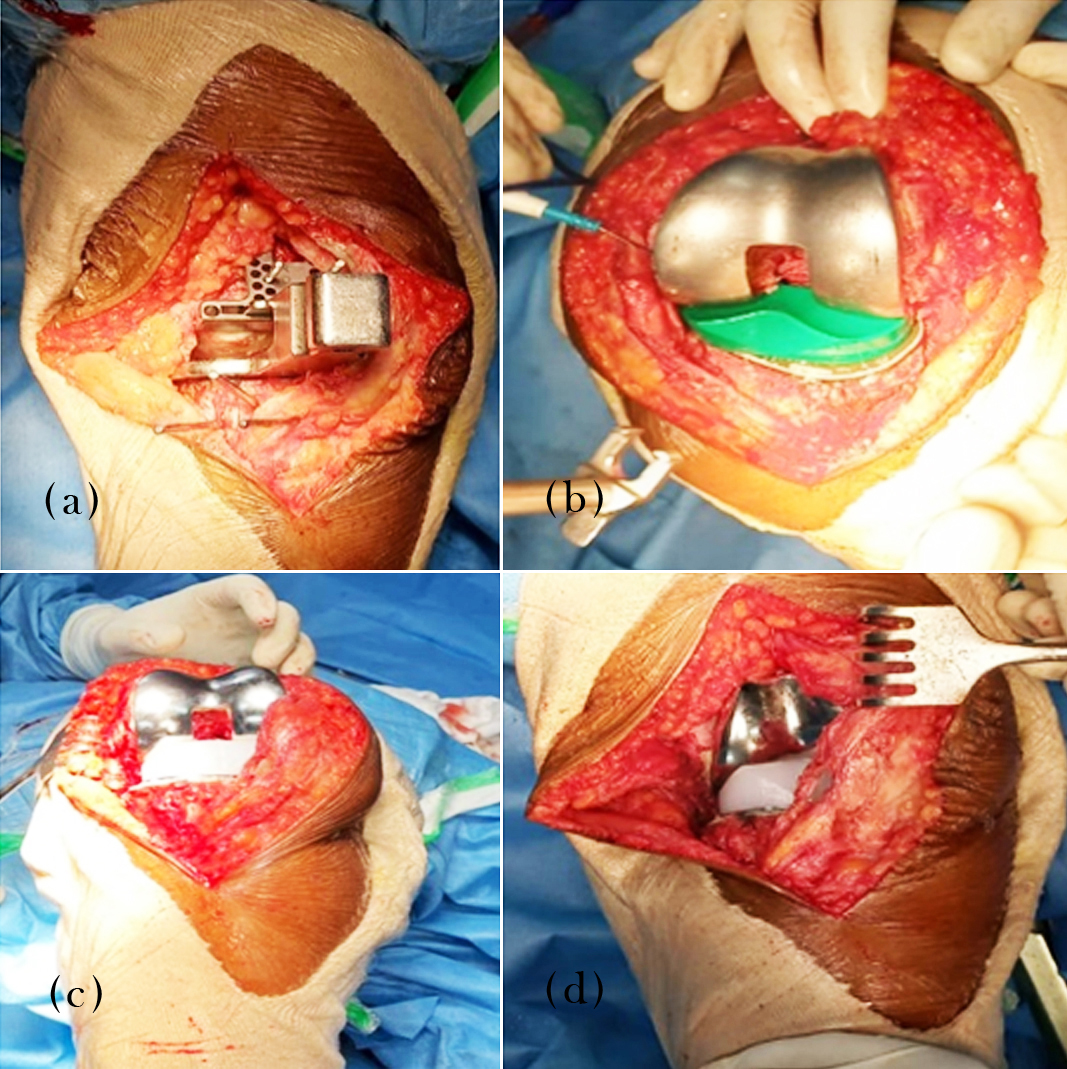
Figure 1: (a) Assessing extension gap, (b) Reduction with trial implants, (c) Flexion with implants, and (d) Knee extension with implant.
Intravenous antibiotics were continued for 3-5 days. Epidural analgesia given till epidural removed on 1st post op day. Low molecular heparin was given for DVT prophylaxis for 5 days after which it was converted to oral ecospirin for 6 weeks. Patients were made to walk with walker on 1st post op day and isometric quadriceps exercises advised. Suction drain removed after 48 hours and patients discharged on 5-7th post op day. Sutures removed on 15th post op day and patient was advised to continue regular physiotherapy.
The patients were assessed clinically, functionally and with X-rays at 6 weeks post-operatively and re-assessed every 6 weeks for a minimum of 12 months. The knee society score (KSS) [12] was tabulated at 12 months by an independent observer. The KSS include pre-op and post-op versions. The objective knee score is completed by surgeon, which includes pain walking on level ground, on stairs or inclines. Also alignment, ligament stability and range of motion are assessed along with flexion contracture or extensor lag. The functional component of the score include a patient specific survey evaluating activities of daily living, sports or recreational activities, patient satisfaction and their expectations. A KSS of 80-100 is considered excellent, 70-79 as good, 60-69 as fair and <60 as poor.
Statistical analysis
A study proforma was used to collect data from patients. Data analysis was done using statistical package SPSS V-27.0 (IBM Corp, Armonk, NY, USA). Qualitative variables were expressed in proportion and quantitative variables were expressed in mean and standard deviation. The mean and standard deviation of knee functional and clinical scores at 12 months follow up and age of patients was calculated. Chi-square test was used to check for any significant association between age and the mean Knee Functional and Clinical Score at follow up. P-value less than 0.05 was considered statistically significant.
Results
Out of the 42 patients, 25(59.5%) belonged to the age group of 60-69 years (Table 1). The youngest patient was 49 and the oldest 79 years. The mean age was 64.33(±6.12). Twenty four (57.1%) patients were females (Table 2). Right side was involved in 25(59%) cases. The mean pre-op knee clinical score was 30(±6.409) in this study which improved to mean post–op score of 92.17(±5.53) (Table 3). According to the knee society clinical scoring, 37(88.1%) had excellent and 5(11.9%) had good results (Table 4). Based on knee clinical scoring system, 7(70%) patients in the age group <60 years, 24(96%) cases in the age group 60 – 69 years and 6(85.7%) cases in the age group ≥70 years had excellent results (Table 5). Out of the 24 females, 23(95.8%) had excellent and 1(4.2%) had good knee clinical scores. Out of the 18 male patients, 14(77.8%) had excellent and 4(22.2%) had good knee clinical scores (Table 6) .
Table 1: Age distribution.
|
Age in years
|
Frequency
|
Percent
|
|
<60
|
10
|
23.8
|
|
60-69
|
25
|
59.5
|
|
≥70
|
7
|
16.7
|
|
Total
|
42
|
100
|
Note: Mean age- 64.33(±6.12)
Table 2: Gender and side distribution.
|
SEX
|
Frequency
|
Percent
|
SIDE
|
Frequency
|
Percent
|
|
Female
|
24
|
57.1
|
Left
|
17
|
40.5
|
|
Male
|
18
|
42.9
|
Right
|
25
|
59.5
|
|
Total
|
42
|
100
|
Total
|
42
|
100
|
Table 3: Knee clinical score and knee functional score.
|
Total cases
|
Knee clinical score
|
Knee functional score
|
|
Min
|
Max
|
Mean
|
Standard deviation
|
Min
|
Max
|
Mean
|
Standard deviation
|
|
Pre- op
|
42
|
20
|
44
|
30
|
6.409
|
20
|
50
|
33.81
|
9.988
|
|
Post- op
|
42
|
79
|
98
|
92.17
|
5.53
|
70
|
90
|
82.38
|
6.917
|
Table 4: Grading of knee clinical and knee functional scores.
|
Knee clinical score
|
Frequency
|
Percent
|
Knee functional score
|
Frequency
|
Percent
|
|
Good
|
5
|
11.9
|
Good
|
6
|
14.3
|
|
Excellent
|
37
|
88.1
|
Excellent
|
36
|
85.7
|
|
Total
|
42
|
100
|
Total
|
42
|
100
|
Table 5: Age and knee clinical score.
|
Age in years
|
Knee clinical score
|
Total
|
|
Good
|
Excellent
|
|
N
|
%
|
N
|
%
|
N
|
%
|
|
<60
|
3
|
30
|
7
|
70
|
10
|
100
|
|
60-69
|
1
|
4
|
24
|
96
|
25
|
100
|
|
≥70
|
1
|
14.3
|
6
|
85.7
|
7
|
100
|
|
Total
|
5
|
11.9
|
37
|
88.1
|
42
|
100
|
Note: Chi-Square test χ2 = 4.65, df =2, p-value= 0.098
Table 6: Gender and knee clinical score.
|
Sex
|
Knee clinical score
|
Total
|
|
Good
|
Excellent
|
|
N
|
%
|
N
|
%
|
N
|
%
|
|
Female
|
1
|
4.2
|
23
|
95.8
|
24
|
100
|
|
Male
|
4
|
22.2
|
14
|
77.8
|
18
|
100
|
|
Total
|
5
|
11.9
|
37
|
88.1
|
42
|
100
|
Note: Chi-Square test χ2 = 3.197, df =1, p-value= 0.074
The mean pre-op knee functional score was 33.81(±9.988), which improved to a mean post–op score of 82.38(±6.917) (Table 3). According to the knee society functional scoring system, 36 cases (85.7%) had excellent and 6(14.3%) had good results (Table 4). Based on knee functional score, 7(70%) patients <60 years, 22(88%) of 60- 69 years and 7(100%) of ≥70 years had excellent results (Table 7). Out of the 24 females, 21(87.5%) had excellent and 3(12.5%) had good knee functional scores. 15(83.3%) males had excellent and 3(16.7%) had good knee functional scores (Table 8).
Table 7: Age and knee functional score.
|
Age
|
Knee functional score
|
Total
|
|
Good
|
Excellent
|
|
N
|
%
|
N
|
%
|
N
|
%
|
|
<60
|
3
|
30
|
7
|
70
|
10
|
100
|
|
60-69
|
3
|
12
|
22
|
88
|
25
|
100
|
|
≥70
|
0
|
0
|
7
|
100
|
7
|
100
|
|
Total
|
6
|
14.3
|
36
|
85.7
|
42
|
100
|
Note: Chi-Square test χ2 = 3.29, df =2, p-value= 0.193
Table 8: Gender and knee functional score.
|
Sex
|
Knee functional score
|
Total
|
|
Good
|
Excellent
|
|
N
|
%
|
N
|
%
|
N
|
%
|
|
Female
|
3
|
12.5
|
21
|
87.5
|
24
|
100
|
|
Male
|
3
|
16.7
|
15
|
83.3
|
18
|
100
|
|
Total
|
6
|
14.3
|
36
|
85.7
|
42
|
100
|
Note: Chi-Square test χ2 = 0.146, df =1, p-value= 0.703
Discussion
In this prospective study involving 42 patients who underwent rotating platform TKA, the outcome was assessed with the knee society score. The scoring system combines a relatively objective knee clinical score (based on clinical parameters) and a knee functional score (based on how the patients perceive that knee function with specific activities). The mean age of the patients in this study was 64.33 (±6.12) years (range 49 to 79) which is comparable to the study done by Maniar et al in Indian population with the low contact stress rotating platform(LCS-RP) knee arthroplasty in 45 patients(55 knees) where the mean age was 59.6 years (range 40 to 77) [13]. In this study of 42 patients who underwent mobile bearing total knee arthroplasty, 85.7% had excellent and 14.3% had good functional outcome at 12 months follow up according to Knee Functional Score.
The mean pre-op knee clinical score was 30(±6.409) in this study which improved to mean post–op score of 92.17(±5.53). An improvement in knee society knee clinical score from 34(pre-op) to 94(post-op) was reported by Argenson et al., involving 112 patients with an average follow up of 10.6 years [14]. Meftah et al [15] in a prospective study of 117 patients reported an improvement in the Knee Society pain score from a pre-op average of 44.1 to final average of 94.3. Maniar et al reported an increase in knee clinical score from a pre operative average of 33 to a final value of 91 with the LCS-RP knee [13]. Vaidya et al [16], using the Press Fit Condylar-Rotating Platform-Posterior stabilized (PFC-RP-PS) design in 121 knees reported an increase in Knee Clinical Score from a mean pre op value of 27 to a final of 93.
The mean pre-op and post-op knee functional scores were 33.81(±9.988) and 82.38(±6.917) respectively in the present study which were also comparable to the results of the previous studies shown below. Argenson et al [14] reported an improvement in knee functional scores from 55(pre-op) to 88(post-op) in his study. Meftah et al [15] reported an improvement in knee functional score from pre-op mean of 39.4 to a post-op mean of 90.2. Maniar et al reported an increase in knee functional score from a pre-op mean 45 to post-op mean 76, with the LCS-RP knee [13]. Study by Vaidya et al [16], reported an increase in Knee Functional score from a mean pre op value of 40 to a final of 95. The post-operative knee flexion was in the range of 95-120 degrees in the present study. The results were comparable to that of the studies done by Vaidya [16], and Maniar et al [13].
Based on knee clinical scoring system, 7(70%) patients in the age group <60 years, 24(96%) cases in the age group 60 – 69 years and 6(85.7%) cases in the age group ≥70 years had excellent results. According to Knee Functional Score, 7(70%) patients <60 years, 22(88%) of 60- 69 years and 7(100%) of ≥70 years had excellent results. But there was no statistically significant association between age group and knee clinical score (p-value= 0.098) or knee functional scores (p-value= 0.193) (Tables 5, 7). Out of 24 females, 23(95.8%) had excellent and 1(4.2%) had good knee clinical scores. Out of the 18 males, 14(77.8%) had excellent and 4(22.2%) had good knee clinical scores. 21(87.5%) females had excellent and 3(12.5%) had good knee functional scores. 15(83.3%) males had excellent and 3(16.7%) had good knee functional scores. There was no statistically significant association between gender and knee clinical score (p-value= 0.074) or knee functional scores (p-value= 0.703) in the current study (Tables 6, 8).
Rotating platform design total knee prostheses combines conformity and mobility and at the same time, provides an increased area of contact and also lower contact stress from extension to flexion, thereby reducing polyethylene wear and aseptic failure after TKA [14]. The rotational mismatch between the femur and tibia is self-corrected in the RP design which improves patella tracking and also reduces anterior knee pain [17]. Anatomic postoperative alignment depends on accurate resection of bone and ligament balancing, is critical for long term survival of knee prosthesis. Gap balancing technique was employed in all cases and the authors found it comfortable for obtaining symmetric and balanced flexion and extension gaps. Femoral component was positioned parallel to the resected proximal tibia with each collateral ligament equally tensioned to obtain a rectangular flexion gap. A precise proximal tibial resection is critical when using a gap balancing technique. A varus tibial resection will result in increased internal rotation of the femoral component and a valgus tibial cut will lead to excessive external rotation of the femoral component. Precise balancing of the flexion and extension gaps is required to prevent the bearing dislocation in mobile bearing knee arthroplasty. Maniar et al reported a case of revision for bearing dislocation in their study of 55 TKAs [13]. Fisher et al [18], reported 7 cases of rotating platform spinouts in a total of 1255 patients (0.56 %). We did not encounter any such bearing related complications in the current study.
One patient developed knee stiffness at 6 weeks follow up and had a knee flexion of 0-80° which was successfully managed with supervised physiotherapy and 95° flexion was attained at 12 months follow up. The prevalence of stiffness as per literature is 1.3% to 12% [19]. Risk factors for stiffness after TKA are reduced preoperative knee range of motion, history of prior knee surgery, prior arthritis, mal-positioning or oversizing of components, and incorrect gap balancing [19]. Czekaj et al in his study of 154 patients, reported 1 case each with deep infection, periprosthetic fracture and a revision for femoral component loosening [20]. Study of 55 knees by Maniar et al reported a complication rate of 6.8%, one case each of infection, aseptic loosening and bearing dislocation [13]. The current study reported no cases of serious complications as discussed above in the limited follow-up period.
The study requires a longer follow up to assess the long term clinical and functional outcome of using RP bearing TKA in patients with osteoarthritis.
Conclusion
Total knee arthroplasty with rotating platform design was found to be performing well and has shown excellent clinical and functional outcome without any serious complications at short term follow-up. Meticulous attention to ligamentous and gap balancing can prevent complications of bearing spin out in RP design TKA. There was no statistically significant association between age or gender with knee clinical and functional scores in the current study.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Roque VA, Agre M, Barroso J, Brito I. Managing knee ostheoarthritis: Efficacy of hyaluronic acid injections. Acta Reumatol Port. 2013; 38:154–161.
[2] Abdel MP, Ollivier M, Parratte S, Trousdale RT, et al. Effect of postoperative mechanical axis alignment on survival and functional outcomes of modern total knee arthroplasties with cement: A concise follow-up at 20 years. J Bone Joint Surg Am. 2018; 100:472–478.
[3] Banks SA, Deckard E, Hodge WA, Meneghini RM. Rationale and results for fixed-bearing pivoting designs in total knee arthroplasty. J Knee Surg. 2019; 32:590–595.
[4] Milligan DJ, O’Brien S, Doran E, Gallagher NE, Beverland DE. Twenty-year survivorship of a cemented mobile bearing total knee arthroplasty. Knee. 2019; 26:933–940.
[5] Zhang Z, Zhu W, Zhang W. High-flexion posterior-substituting versus cruciate-retaining prosthesis in total knee arthroplasty: functional outcome, range of motion and complication comparison. Arch Orthop Trauma Surg. 2015; 135:119–24.
[6] Ollivier M, Parratte S, Lino L, Flecher X, Pesenti S, et al. No benefit of computer-assisted TKA: 10-year results of a prospective randomized study. Clin Orthop. 2018; 476:126–34.
[7] Capella M, Dolfin M, Saccia F. Mobile bearing and fixed bearing total knee arthroplasty. Annal Transl Med. 2016; 4:127–129.
[8] Powell AJ, Crua E, Chong BC, Gordon R, McAuslan A, et al. A randomized prospective study comparing mobile-bearing against fixed-bearing PFC Sigma cruciate-retaining total knee arthroplasties with ten-year minimum follow-up. Bone Jt J. 2018; 100:1336–1344.
[9] Moskal JT, Capps SG. Rotating-platform TKA no different from fixed-bearing TKA regarding survivorship or performance: a meta-analysis. Clin Orthop. 2014; 472:2185–2193.
[10] Wang K, Zhang FF, Yan X, Shen Y, Cai W, et al. Superior Mid- to long-term clinical outcomes of mobile-bearing total knee arthroplasty compared to fixed-bearing: A meta-analysis based on a minimum of 5 years of study. J Knee Surg. 2021; 34:1368–1378.
[11] Quinlan ND, Wu Y, Chiaramonti AM, Guess S, Barfield WR, et al. Functional flexion instability after rotating-platform total knee arthroplasty. J Bone Joint Surg Am. 2020; 102:1694–1702.
[12] Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, et al. The new knee society knee scoring system. Clin Orthop Relat Res. 2012; 470:3–19.
[13] Maniar RN, Singhi T, Gangaraju B, Patil A, Maniar PR. Mid term results of LCS knee. The Indian experience. Indian J Orthop. 2013; 47:57–62.
[14] Argenson AJ, Parratte S, Ashour A. The outcome of rotating-platform total knee arthroplasty with cement at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2012; 94:638–644.
[15] Meftah M, Ranawat SA, Ranawat CS. Ten-year follow up of a rotating-platform, posterior-stabilized total knee arthroplasty. J Bone Joint Surg Am. 2012; 94:426–432.
[16] Vaidya SV, Virani S, Phunde R. What have we learned from 100% success of press fit condylar rotating platform posterior stabilized knees?: A 5-10 years followup by a nondesigner. Indian J Orthop. 2016; 50:647–654.
[17] Abdel MP, Tibbo ME, Stuart MJ, Trousdale RT, Hanssen AD, et al. A randomized controlled trial of fixed- versus mobile-bearing total knee arthroplasty: a follow-up at a mean of ten years. Bone Joint J. 2018; 100:925–929.
[18] Fisher DA, Bernasek TL, Puri RD. Rotating platform spinouts with cruciate- retaining mobile-bearing knees. J Arthroplasty. 2011; 26:877–882.
[19] Manrique J, Gomez MM, Parvizi J. Stiffness after total knee arthroplasty. J Knee Surg. 2015; 28:119–126.
[20] Czekaj J, Fary C, Gaillard T. Does low-constraint mobile bearing knee prosthesis give satisfactory results for severe coronal deformities? A five to twelve year follow up study. Int Orthop. 2017; 41:1369–1377.