Full Text
Introduction
Cholecystectomy, the surgical removal of the gallbladder, is one of the most frequently performed surgeries worldwide. It has become the preferred treatment for a variety of conditions, including gallbladder inflammation (cholecystitis), pain caused by gallstones (biliary colic), and pancreatitis triggered by gallstones. The widespread use of cholecystectomy can be attributed to its effectiveness in providing lasting relief from the symptoms associated with these conditions, which, if left untreated, can lead to severe complications [1].
The journey to the modern cholecystectomy, however, is relatively recent in the history of medicine. Before the late 1800s, gallbladder diseases were primarily treated through a procedure called cholecystostomy. This approach involved making an incision to open the gallbladder, remove the stones, and drain any accumulated fluid. At the time, there was a prevailing belief among medical practitioners that completely removing the gallbladder would be fatal to patients. This belief was largely due to the lack of understanding of the gallbladder's role in the body and concerns about the potential consequences of its removal [2].
The cholecystostomy procedure provided only temporary relief. While it could alleviate immediate symptoms by removing gallstones or draining infected fluids, it did not offer a permanent solution. Patients often continued to suffer from recurrent pain, infections, and the formation of fistulas-abnormal connections that develop between the gallbladder and other organs or the skin. As a result, the search for a more effective and lasting treatment for gallbladder disease continued. The idea that the gall bladder was essential was first challenged in the late 1600s, when two Italian doctors proved animals could live without it [3, 4].
In 1882, Langenbuch performed the first successful cholecystectomy on a man who had suffered from gallstones for 16 years. The patient’s condition improved dramatically, and he was effectively cured of his painful ailment overnight. This groundbreaking procedure marked a turning point in the treatment of gallbladder diseases [5].
By 1897, over 100 cholecystectomies had been performed, proving that gallbladder removal not only alleviated pain but also significantly improved patients' quality of life. The success of these early surgeries helped establish cholecystectomy as a viable and effective treatment option, gradually replacing cholecystostomy as the gold standard for nearly a century. The open cholecystectomy, which involves a larger abdominal incision to access and remove the gallbladder, became the preferred surgical approach during this period [6].
The next major advancement in gallbladder surgery came in the 1980s with the introduction of laparoscopic techniques. In 1985, German surgeon Erich Mühe performed the first laparoscopic cholecystectomy, using a small camera and specialized instruments inserted through small incisions in the abdomen. This minimally invasive technique was a radical departure from the traditional open approach. The laparoscopic method was soon replicated by a French gynecologic surgeon in 1987, who successfully removed a gallbladder using similar laparoscopic tools. This technique quickly gained popularity among surgeons due to its numerous advantages over the open procedure [5, 6].
The laparoscopic approach offered several benefits, including smaller incisions, reduced pain, shorter hospital stays, quicker recovery times, and lower rates of post-operative complications. These advantages were quickly recognized by the medical community, and within two years, laparoscopic cholecystectomy had revolutionized surgical practice in the United States. The rapid adoption of this technique reflected a broader trend in surgery towards minimally invasive procedures that prioritize patient comfort and faster recovery [6, 7].
In 1992, the National Institutes of Health (NIH) officially endorsed the laparoscopic cholecystectomy in its new guidelines, recognizing the procedure’s safety and effectiveness. This endorsement further solidified the procedure's status as the preferred method for gallbladder removal. Since then, laparoscopic cholecystectomy has become the standard approach for treating gallbladder diseases, with millions of procedures performed worldwide each year [7].
Traditionally, the Tokyo Guidelines are used to assess the severity of acute cholecystitis. However, the three grades outlined in these guidelines are based on local signs of inflammation, systemic signs of inflammation and radiological findings of acute cholecystitis. It does not adequately account for intraoperative findings. There is a clear need for a preoperative scoring system that can reliably predict difficult or complex laparoscopic cholecystectomy cases. Such a system would aid in selecting patients for day-case surgery, determining optimal timing and operating room preparation, assigning cases to surgeons with appropriate expertise, and providing detailed patient counseling during the consent process. The Nassar Difficulty Grading Scale is widely regarded as a simple, clinically relevant, and surgically applicable preoperative scoring system that effectively addresses these needs [7, 8].
Today, cholecystectomy remains one of the most common surgeries, with the laparoscopic approach being the dominant technique. The evolution of cholecystectomy-from the early days of cholecystostomy to the pioneering open procedures and the modern laparoscopic era-illustrates the continuous advancements in surgical practice and the ongoing quest to improve patient outcomes. The history of gallbladder surgery is a testament to medical innovation and the willingness of physicians to challenge established beliefs in pursuit of better treatments and care for their patients. As surgical techniques continue to evolve, the focus remains on refining these methods to enhance safety, efficacy, and patient comfort, ensuring that the treatment of gallbladder diseases continues to improve in the years to come [8].
The present study was done to assess the reliability of C-reactive protein and Gall bladder wall thickness as a predictor for difficult laparoscopic cholecystectomy.
Materials and methods
The prospective, observational study conducted at The Department of General Surgery, Jubilee Mission Medical College and Research Institute, Thrissur from October 2022 to March 2024. Approval for the study was granted by Institutional Ethics Committee, Jubilee Mission Medical College & Research Institute, Thrissur. Institutional Ethics Committee Study Reference Number was 32/22/IEC/JMMC&RI. Evaluation was done by appropriate lab and radiological investigation, and outcomes was assessed by appropriate scoring system for intra operative difficulty. Consent was obtained or waived by all participants in this study.
Based on the sensitivity of GBW Thickness for predicting conversion of lap into open cholecystectomy in an earlier Publication “D Kania, Ultrasound of the gallbladder wall thickness and the risk of conversion/10.1515/pjs-2016-0073" with 95% confidence level and 10% relative allowable error, minimum sample size comes to 50 [9].
Inclusion criteria: The study's inclusion criteria require patients to be over 18 years of age and undergoing either early or interval laparoscopic cholecystectomy. Participants must also provide informed consent and have completed both a preoperative ultrasound (USG) and C-reactive protein (CRP) test within two weeks before the study.
Exclusion criteria: The exclusion criteria for the study include patients under the age of 18, those with ultrasound (USG) reports or preoperative C-reactive protein (CRP) values obtained more than two weeks prior to surgery, and patients who decline participation in the study. Additionally, patients who have undergone tube cholecystostomy or had gallbladder perforation are also excluded.
Data collection
The pre OP CRP value and GBWT based on USG report was analyzed with intra OP difficulty given by Nassar criteria. The Cut Off Value for normal gall bladder wall thickness is <4mm and that for CRP is <0.6mg/dL. The significance of increased CRP is that high pre OP values is associated with increasing difficulty in laparoscopic cholecystectomy since it is an objective finding surrogate of inflammation/fibrosis.
Data analysis
Analysis was carried out using Pearson chi-square test or Fischer's exact test for qualitative variables. A p-value <0.05 was considered significant in all statistical analyses. To determine the cutoff value of CRP as a predictor for a difficult laparoscopic cholecystectomy, ROC analysis was performed to assess its sensitivity, specificity, and positive and negative predictive values as a pre-operative marker for intraoperative difficulty. Data analysis was conducted using IBM SPSS Statistics software, version 25.0.0 (IBM Corp., Armonk, New York, USA).
Results
The study has been conducted to determine the relationship between gallbladder wall thickness and CRP levels with the degree of difficulty in performing a laparoscopic cholecystectomy.
The study population primarily consists of middle-aged to older adults, with the highest representation in the 51 to 60-year age group. No participants are aged 10 to 20 years, suggesting a focus on conditions affecting older individuals. The study had 29 (58%) females and 21 (42%) males, indicating a higher proportion of female participants. This gender distribution may suggest that the condition or treatment studied is more common or relevant among females. Understanding both age and sex distributions is essential for interpreting the study's findings and potential gender-specific outcomes.
Out of the 50 patients studied, 11 (22%) had blood group A (both positive and negative), 16 (32%) had blood group B (positive), 22 (44%) had blood group O (both positive and negative), and 1 (2%) patient had blood group AB (positive) as depicted in Figure 1.
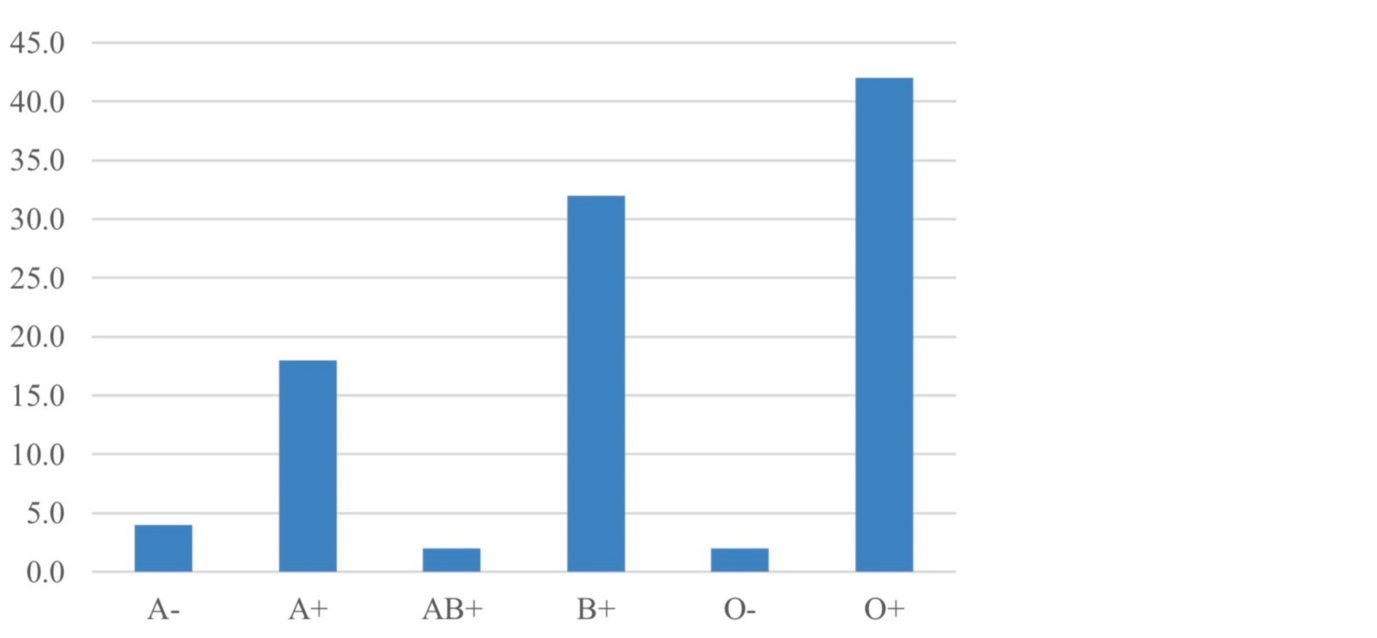
Figure 1: Blood group distribution among the study subjects. x axis - blood groups of participants; y axis - percentage of participants with corresponding blood groups.
Of the 50 patients analyzed, 21 (42%) were classified as overweight, 19 (38%) had a normal body mass index (BMI), and 10 (20%) were categorized as Obese Grade 1. Dietary habits revealed that a significant majority, 45 (90%), adhered to a mixed diet, while 5 (10%) were strictly vegetarian. Regarding alcohol consumption, 9 (18%) of the patients reported alcohol use, whereas 41 (82%) abstained. This is represented in Table 1.
Table 1: Distribution of patients with obesity, diet and alcohol.
|
Parameter
|
Frequency
|
Percent
|
|
|
N
|
19
|
38
|
|
Obesity
|
|
|
Obese 1
|
10
|
20
|
|
|
Overweight
|
21
|
42
|
|
Total
|
50
|
100
|
|
Diet
|
|
|
Mixed
|
45
|
90
|
|
|
Vegetarian
|
5
|
10
|
|
Total
|
50
|
100
|
|
Alcohol
|
|
|
Yes
|
9
|
18
|
|
|
No
|
41
|
82
|
|
Total
|
50
|
100
|
Table 2 presents the distribution of symptoms among the 50 patients studied. Pain was the most common symptom, reported by 46 (92%) patients, while only 4 (8%) did not experience pain. Fever was observed in 27 (54%) patients, with the remaining 23 (46%) not having this symptom. Vomiting was noted in 22 (44%) patients, whereas 28 (56%) did not report vomiting. These findings indicate that pain was the predominant symptom, followed by fever and vomiting, in the patient population.
Table 2: Distribution of the patients with their symptoms.
|
Parameter
|
Frequency
|
Percent
|
|
Pain
|
|
|
Yes
|
46
|
92
|
|
|
No
|
4
|
8
|
|
Total
|
50
|
100
|
|
Fever
|
|
|
Yes
|
27
|
54
|
|
|
No
|
23
|
46
|
|
Total
|
50
|
100
|
|
Vomiting
|
|
|
Yes
|
22
|
44
|
|
|
No
|
28
|
56
|
|
Total
|
50
|
100
|
Among the 50 patients studied, 25 (50%) demonstrated increased gallbladder wall thickness (GBWT) on preoperative ultrasound (USG). Additionally, 48 (96%) of the patients were diagnosed with calculus cholecystitis, while 2 (4%) had acalculous cholecystitis. These findings highlight a high prevalence of gallstones in the patient population and a notable association between increased GBWT and the presence of calculus cholecystitis as shown in Table 3.
Table 3: Distribution of the patients with their GBWT and GB stone.
|
Parameter
|
Frequency
|
Percent
|
|
GBWT
|
|
|
Increased
|
25
|
50
|
|
|
Normal
|
25
|
50
|
|
Total
|
50
|
100
|
|
GB stone
|
|
|
Yes
|
48
|
96
|
|
|
No
|
2
|
4
|
|
Total
|
50
|
100
|
The intraoperative difficulty of laparoscopic cholecystectomy was evaluated using the Nassar scale and is represented in Figure 2. Among the 50 patients studied, 22 (44%) experienced grade 1 difficulty, 18 (36%) had grade 2 difficulty, 8 (16%) faced grade 3 difficulty, and 2 (4%) encountered grade 4 difficulty. No patients were reported to have grade 5 difficulty.
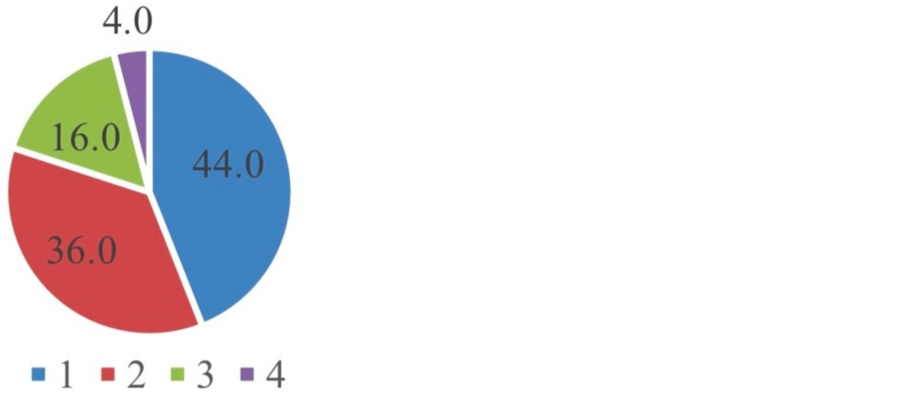
Figure 2: Difficulty based on Nassar grades: Grade 1: 22 (44%); Grade 2: 18 (36%); Grade 3: 8 (16%); Grade 4: 2 (4%); Grade 5: Nil.
The descriptive analysis of the variables shows that the patients' ages ranged from 22 to 82 years, with a mean age of 50.49 and a standard deviation of 17.359. CRP values ranged from 0.01 to 29.90, with a mean of 6.0044 and a high variability (standard deviation of 9.36456). Hemoglobin levels ranged from 8.3 to 17.2, with a mean of 11.652 and a standard deviation of 1.7787, indicating moderate variation in Hb levels among patients as shown in Table 4.
Table 4: Descriptive statistics of variables.
|
Variables
|
Minimum
|
Maximum
|
Mean
|
Std. Deviation
|
|
Age
|
22
|
82
|
50.49
|
17.359
|
|
CRP
|
0.01
|
29.9
|
6.0044
|
9.36456
|
|
Hb
|
8.3
|
17.2
|
11.652
|
1.7787
|
Crosstabulation: The chi-square test for independence between gallbladder wall thickness (GBWT) and CRP levels yielded a highly significant p-value of <0.001 and a Pearson chi-square statistic of 13.235. It is shown in Table 5.
Table 5: Correlation of the GBWT with the CRP.
|
CRP
|
>2.5
|
<2.5
|
Total
|
|
GBWT
|
>3MM
|
Count
|
14
|
11
|
25
|
|
% within GBWT
|
56%
|
44%
|
100%
|
|
<3MM
|
Count
|
2
|
23
|
25
|
|
% within GBWT
|
8.00%
|
92%
|
100%
|
|
Total
|
Count
|
16
|
34
|
50
|
|
% within GBWT
|
32%
|
68%
|
100%
|
The chi-square test for independence between gallbladder wall thickness (GBWT) and the difficulty of laparoscopic cholecystectomy demonstrated a highly significant p-value of <0.001, with a Pearson chisquare statistic of 12.5, as presented in Table 6.
Table 6: Correlation of the GBWT with the NASSAR.
|
NASSAR
|
Grade 3 or 4
|
Grade 1 or 2
|
Total
|
|
GBWT
|
>3MM
|
Count
|
10
|
15
|
25
|
|
% within GBWT
|
40%
|
60%
|
100%
|
|
<3MM
|
Count
|
0
|
25
|
25
|
|
% within GBWT
|
0%
|
100%
|
100%
|
|
Total
|
Count
|
10
|
40
|
50
|
|
% within GBWT
|
20%
|
80%
|
100%
|
The chi-square test for independence between gallbladder wall thickness (GBWT) and the difficulty of laparoscopic cholecystectomy demonstrated a highly significant p-value of <0.001, with a Pearson chi-square statistic of 13.235. The correlation between CRP and difficult laparoscopic cholecystectomy is shown in Table 7.
Table 7: Correlation of the CRP with the NASSAR.
|
NASSAR
|
Grade 3 or 4
|
Grade 1 or 2
|
Total
|
|
CRP
|
>2.50
|
Count
|
8
|
8
|
16
|
|
% within CRP
|
50%
|
50%
|
100%
|
|
<=2.50
|
Count
|
2
|
32
|
34
|
|
% within CRP
|
5.9%
|
94.1%
|
100%
|
|
Total
|
Count
|
10
|
40
|
50
|
|
% within CRP
|
20%
|
80%
|
100%
|
The ROC curve displays the balance between sensitivity and false positive rate (1-specificity) at all cut-off points, enabling evaluation of a test's performance regardless of the decision threshold. In this analysis, CRP was identified as a reliable predictor of difficult laparoscopic cholecystectomy with an AUC of 0.790 (95% CI, 0.606-0.974). The AUC summarizes the diagnostic accuracy, with values closer to 1 indicating higher accuracy; 0.5 suggests no discrimination, while 0.7-0.9 is acceptable to excellent, and above 0.9 is outstanding. This is represented in Figure 3.
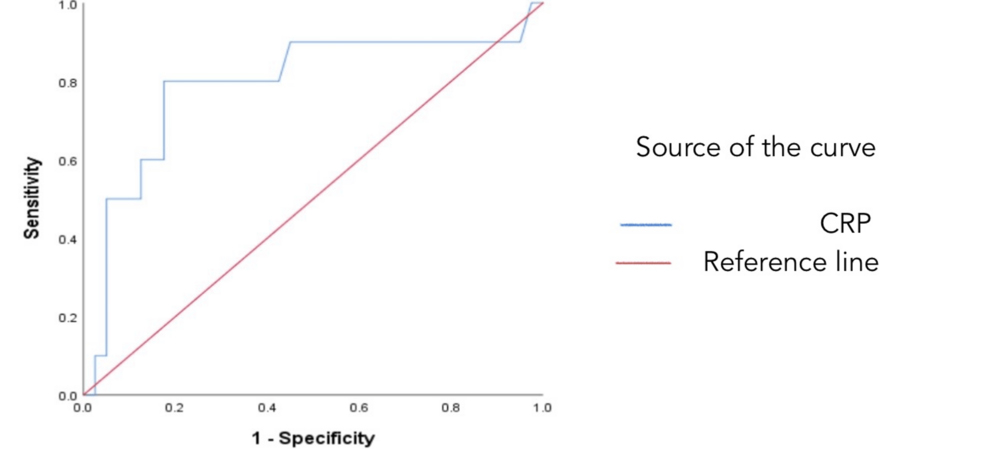
Figure 3: ROC curve showing CRP as a good predictor of difficult laparoscopic cholecystectomy.
Discussion
The study has been conducted to determine the relationship between gallbladder wall thickness and CRP levels with the degree of difficulty in performing a laparoscopic cholecystectomy. In our study, the population primarily consists of middle-aged to older adults, with the highest representation in the 51 to 60- year age group, and no participants aged 10 to 20 years, indicating a focus on conditions more prevalent in older individuals. Females comprise 29 (58%) of the study sample, while males account for 21 (42%), suggesting that the condition or treatment may be more common or relevant among females. Understanding the age and sex distributions is crucial for interpreting the study's findings and identifying potential gender specific outcomes. This demographic pattern aligns with findings by Kanakala et al. and Shi et al. who also reported that most patients undergoing laparoscopic cholecystectomy are middle-aged, with a predominance of female patients [10, 11].
In our study of 50 patients, 22 (44%) had blood group O (both positive and negative), 11 (22%) had blood group A (both positive and negative), 16 (32%) had blood group B (positive), and 1 (2%) patient had blood group AB (positive). This distribution is consistent with the findings of Radunovic et al. and Barrett-Lee J. et al. who also reported that blood group O is the most common among patients, followed by blood groups A and B [12, 13].
In our study of 50 patients, 21 (42%) were classified as overweight, 19 (38%) had a normal body mass index (BMI), and 10 (20%) were categorized as Obese Grade 1. Dietary habits indicated that 45 (90%) of the patients followed a mixed diet, while 5 (10%) were strictly vegetarian. Additionally, 9 (18%) reported alcohol consumption, with 41 (82%) abstaining. This aligns with findings by Radunovic et al. and Farkas et al. which also reported that the majority of patients undergoing similar studies are overweight [12-14].
In our study of 50 patients, it was found that pain was the most prevalent symptom, reported by 46 (92%) of the participants, while only 4 (8%) did not experience pain. Fever was observed in 27 (54%) of the patients, and 23 (46%) did not have this symptom. Vomiting was present in 22 (44%) of the patients, with 28 (56%) not reporting vomiting. These findings show that pain is the most common symptom, followed by fever and vomiting. This is consistent with the studies by Bülent Mentes et al., Radunovic et al. and Bates et al. which also reported that most patients experience pain, fever, and vomiting [12, 15, 16].
In our study of 50 patients, 25 (50%) showed increased gallbladder wall thickness (GBWT) on pre-operative ultrasound (USG). Additionally, 48 (96%) were diagnosed with calculus cholecystitis, while 2 (4%) had acalculous cholecystitis. These results indicate a high prevalence of gallstones and a significant association between increased GBWT and calculus cholecystitis. Similar findings were reported by Radunovic et al. and Kokoroskos et al. who also observed increased gallbladder wall thickness in their patient populations [12-17].
In our study, the intraoperative difficulty of laparoscopic cholecystectomy was assessed using the Nassar scale. Of the 50 patients evaluated, 22 (44%) experienced grade 1 difficulty, 18 (36%) had grade 2 difficulty, 8 (16%) encountered grade 3 difficulty, and 2 (4%) faced grade 4 difficulty, with no patients experiencing grade 5 difficulty. This distribution is consistent with findings by Ramírez-Giraldo et al. and Ng HJ et al. who also used the Nassar scale and reported that most patients had grade 1 difficulty, followed by grades 2 and 3 [18, 19] (Table 8).
Table 8: Nassar scale for intra operative difficulty in laparoscopic cholecystectomy.
|
Nassar Grade
|
Gallbladder
|
Cystic pedicle
|
Adhesions
|
|
I
|
Floppy, nonadherent
|
Thin and clear
|
Simple up to neck/Hartmann’s pouch
|
|
II
|
Mucocele, packed with stones
|
Fat-laden
|
Simple up to the body
|
|
III
|
Deep fossa, acute cholecystitis, contracted, fibrosis, Hartman’s adherent to Common bile duct, impaction
|
Abnormal anatomy or cystic duct short, dilated, or obscured
|
Dense up to fundus; involving hepatic flexure or duodenum
|
|
IV
|
Completely obscured, empyema, gangrene, mass
|
Impossible to clarify
|
Dense, fibrosis, wrapping the gallbladder, duodenum or hepatic flexure difficult to separate
|
|
V
|
Findings as in Grade 4+presence of either Mirizzi type 2 or higher, cholecystocutaneous or cholecystoenteric fistula
|
In our study, descriptive analysis of the variables revealed that patient ages ranged from 22 to 82 years, with a mean age of 50.49 and a standard deviation of 17.359. CRP levels varied widely, from 0.01 to 29.90, with a mean of 6.0044 and a standard deviation of 9.36456, indicating high variability. Hemoglobin levels ranged from 8.3 to 17.2, with a mean of 11.652 and a standard deviation of 1.7787, reflecting moderate variation among patients. Similar findings were reported by Bülent Mentes B et al. and Radunovic et al. who observed hemoglobin levels ranging from 7 to 16 [12, 15]. In our study, the chi-square test for independence showed a highly significant correlation between gallbladder wall thickness (GBWT) and CRP levels, with a p-value of <0.001 and a Pearson chi-square statistic of 13.235. Additionally, a significant association was observed between GBWT and the difficulty of laparoscopic cholecystectomy, with a p-value of <0.001, with a Pearson chi-square statistic of 13.235. These results align with the findings of Radunovic et al. and N. Kokoroskos et al. which also reported similar correlations [12-17].
A similar study by Kokoroskos et al. found that gallbladder wall thickness (GBWT) was a robust and objective indicator of risk and complexity in laparoscopic cholecystectomy, as reflected by operative time and intraoperative events. GBWT also independently predicted the length of hospital stay. In another study by Ng et al. a higher Nassar scale grade was observed with elevated preoperative peak CRP concentrations, suggesting that increased CRP levels can predict greater operative difficulty and may assist in surgical planning [17-19].
The ROC curve illustrates the trade-off between sensitivity and the false positive rate (1-specificity) across all cut-off points, allowing for the assessment of a test's performance independently of the decision threshold. In our analysis, CRP was shown to be a reliable predictor of difficult laparoscopic cholecystectomy, with an AUC of 0.790 (95% CI, 0.606-0.974). The AUC provides a summary of the diagnostic accuracy, where values closer to 1 indicate higher accuracy; an AUC of 0.5 suggests no discrimination, 0.7-0.9 is considered acceptable to excellent, and above 0.9 is outstanding. Similar to our findings, studies by Vivek MA et al. and Gupta N et al. also used ROC curve analysis to demonstrate that AUC values closer to 1 reflect greater diagnostic accuracy [20, 21].
The limitations of the study include procedures being performed by surgeons with different levels of experience, and a small study population, which restricts the generalizability of the results.
Conclusions
The study concludes that increased gallbladder wall thickness and elevated CRP levels are significant predictors of increased difficulty in laparoscopic cholecystectomy. These findings underscore the importance of preoperative evaluation of GBWT and CRP as useful tools for anticipating surgical challenges, thereby aiding in better surgical planning and potentially improving patient outcomes. Further studies with larger sample sizes are needed to validate these results and refine the predictive accuracy of these markers.
Acknowledgements
The authors wish to place on record their gratitude to Mr. Unnikrishnan for the statistical help and assistance. They are also grateful to Ms. Mridula of research department for the efforts and invaluable guidance provided in preparing this manuscript.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Garg PK, Pandey D, Sharma J. The surgical management of gallbladder cancer. Expert Rev Gastroenterol Hepatol. 2015, 9:155–166.
[2] Tang C. Technological change in “ordinary medicine”. The emergence of minimally invasive gallbladder surgery, c. 1970–1992; Thesis. Available from: https://escholarship.mcgill.ca/concern/theses/5712mc66h
[3] Hung YL, Sung CM, Fu CY, Liao CH, Wang SY, et al. Management of patients with acute cholecystitis after percutaneous cholecystostomy. From the acute stage to definitive surgical treatment. Front Surg. 2021, 15:616320.
[4] Mousa OY, Kamath PS. A history of the assessment of liver performance. Clin Liver Dis (Hoboken). 20212918, 1:28–48.
[5] Helling TS, Azoulay D. Historical foundations of liver surgery. Springer International Publishing, 2020; 23:10–1007.
[6] Sun J, Xie TG, Ma ZY, Wu X, Li BL. Current status and progress in laparoscopic surgery for gallbladder carcinoma. World J Gastroenterol. 2023, 28:2369–2379.
[7] Buia A, Stockhausen F, Hanisch E. Laparoscopic surgery- A qualified systematic review. World J Methodol. 2015, 26:238–254.
[8] Gallstones and laparoscopic cholecystectomy. NIH Consens Statement. 1992. 10:1–28.
[9] Kania D. Ultrasound measurement of the gallbladder wall thickness in the Assessment of the Risk of Conversion from Elective Laparoscopic Cholecystectomy to Open Surgery - Olkusz County Experience. Pol Przegl Chir. 2016; 88:334–345.
[10] Kanakala V, Borowski DW, Pellen MG, Dronamraju SS, Woodcock SA, et al. Risk factors in laparoscopic cholecystectomy. a multivariate analysis. Int J Surg. 2011:318–323.
[11] Shi HY, Lee KT, Lee HH, Uen YH, Tsai JT, et al. Post-cholecystectomy quality of life: a prospective multicenter cohort study of its associations with preoperative functional status and patient demographics. J Gastrointest Surg. 2009, 13:1651–1658.
[12] Radunovic M, Lazovic R, Popovic N, Magdelinic M, Bulajic M, et al. Complications of Laparoscopic Cholecystectomy, Our Experience from a Retrospective Analysis. Open Access Maced J Med Sci. 2016, 15:641–646.
[13] Barrett-Lee J, Vatish J, Vazirian-Zadeh M, Waterland P. Routine blood group and antibody screening prior to emergency laparoscopy. Ann R Coll Surg Engl. 2018, 100:322–325.
[14] Farkas DT, Moradi D, Moaddel D, Nagpal K, Cosgrove JM. The impact of body mass index on outcomes after laparoscopic cholecystectomy. Surg Endosc. 2012, 4:964–969.
[15] Bates T, Ebbs SR, Harrison M, A'Hern RP. Influence of cholecystectomy on symptoms. Br J Surg. 1991, 78:964–967.
[16] Mentes BB, Akin M, Irkörücü O, Tatlicioğlu E, Ferahköşe Z, et al. Gastrointestinal quality of life in patients with symptomatic or asymptomatic cholelithiasis before and after laparoscopic cholecystectomy. Surg Endosc. 2001, 15:1267–1272.
[17] Kokoroskos N, Peponis T, Lee JM, El Hechi M, Naar L, et al. Gallbladder wall thickness as a predictor of intraoperative events during laparoscopic cholecystectomy- A prospective study of 1089 patients. Am J Surg. 2020, 220:1031–1037.
[18] Ramírez-Giraldo C, Alvarado-Valenzuela K, Isaza-Restrepo A, Navarro-Alean J. Predicting the difficult laparoscopic cholecystectomy based on a preoperative scale. Updates Surg. 2022, 74:969–977.
[19] Ng HJ, Ahmed Z, Khan KS, Katbeh T, Nassar AHM. C-reactive protein level as a predictor of difficult emergency laparoscopic cholecystectomy. BJS Open. 2019, 2:641–645.
[20] Vivek MA, Augustine AJ, Rao R. A comprehensive predictive scoring method for difficult laparoscopic cholecystectomy. J Minim Access Surg. 2014, 10:62–67.
[21] Gupta N, Ranjan G, Arora MP, Goswami B, Chaudhary P, et al. Validation of a scoring system to predict difficult laparoscopic cholecystectomy. Int J Surg. 2013:1002–1006.