Orginal Research
2025
March
Volume : 13
Issue : 1
Gender differences among newly diagnosed type 2 diabetes mellitus patients at tertiary care hospital
Verma K, Karnam N, Haritha M, Manchi RK, Sangeeta BSR
Pdf Page Numbers :- 56-58
Kavyanshi Verma1, Nithya Karnam2, Haritha M3, Rajesh Kumar Manchi1,* and Sangeeta BSR4
1Department of Pharmacology, T.S. Misra Medical College, T.S. Mishra University, Anora, Lucknow 226009, India
2Department of Pharmacology, Sri Venkateswaraa Medical College Hospital and Research Institute, Affiliated to Sri Venkateswaraa University, Red hills, Chennai, Tamil Nadu 600067, India
3Department of Pharmacology, Narayana Medical College, Chintareddy Palam, Nellore, Andhra Pradesh 524003, India
4Symbiosis College of Nursing, Faculty of Nursing, Symbiosis International University, Pune 412115, India
*Corresponding author: Dr. Rajesh Kumar Manchi, Department of Pharmacology, T.S. Misra Medical college, T.S. Misra University, Anora, Lucknow, 226401, India. Email: manchirajesh1985@gmail.com
Received 19 September 2024; Revised 11 November 2024; Accepted 19 November 2024; Published 3 December 2024
Citation: Verma K, Karnam N, Haritha M, Manchi RK, Sangeeta BSR. Gender differences among newly diagnosed type 2 diabetes mellitus patients at tertiary care hospital. J Med Sci Res. 2025; 13(1):56-58. DOI: http://dx.doi.org/10.17727/JMSR.2024/13-10
Copyright: © 2025 Verma K et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Diabetes mellitus (DM) refers to a diverse group of metabolic conditions marked by elevated blood sugar levels, with type 2 DM specifically involving insulin resistance where cells fail to respond effectively to insulin. The objective of the study was to evaluate gender differences among type 2 diabetes mellitus (T2DM) patients based on body mass index (BMI), clinical presentation and glycemic parameters.
Methodology: This prospective, cross-sectional, study comprised 100 newly diagnosed T2DM patients attending Department of General Medicine. The patients were included in the study after obtaining institutional ethics approval and informed consent as per the inclusion and exclusion criteria. The patient demographics and glycemic parameters like fasting blood sugars, post-prandial blood sugars, HBA1c, C-peptide, and fasting insulin were obtained and analyzed.
Results: Among 100 T2DM patients, 25 were female and 75 were male patients. More T2DM female patients were in age range of 41-50 years followed by 51-60, and this was comparable with age ranges of male patients. Burning sensation in legs was comparable between the gender. Majority of female patients had BMI more 30 kg/m2 and majority of male had normal BMI. The glycemic parameter was comparable between both genders.
Conclusion: This study results demonstrated the gender differences among the T2DM patients which was significant with BMI and, among other parameter comparable which may require large sample size to confirm the differences.
Keywords: diabetes mellitus; clinical characterization; incidence
Full Text
Introduction
Diabetes is an important risk factor. It is estimated that the number of diabetic patients will reach 552 million by 2030 [1, 2]. Diabetic eye disease and nephropathies are common diabetic complications, that can lead to blindness and renal failure [3-5]. In addition, diabetes is also significantly related to the occurrence, death and all-cause mortality of cerebrovascular diseases, making it a serious economic burden for individuals and society. Type 2 diabetes affects both the male and female, and is highly associated with morbidity, mortality, and a high health cost to individual patients, their families, and countries [6, 7].
The present study aimed to study the gender differences in BMI, clinical characteristics and glycemic control among type 2 diabetes mellitus (T2DM) patients.
Methodology
This prospective, cross-sectional study was conducted at Department of Pharmacology in collaboration with Department of Medicine, Rama Medical College & Research Hospital during March 2022 to August 2022 comprising a sample size of 100 newly diagnosed T2DM patients. The study has been approved by the institutional ethical committee. The adults T2DM patients aged between 30 and 65 years of both genders were included in the study. Already known diabetics, pregnant women and those who are not willing to provide informed consent or participation in study were excluded from the study. The included patient’s demographic data was collected. The blood samples were collected into vacutainer with standard procedures and analyzed for FBS, PPBS, HBA1c, fasting insulin and c-peptide levels to evaluate the glycemic control [8]. BMI was calculated using standard method [9]. HOMA-IR was calculated using previously described method [10]. Male preponderance and age‑wise increase in prevalence noted as per the study [11]. The clinical symptoms (polydipsia, polyuria, polyphagia) incidence was in line with previous study [12].
Statistical analysis
The data was analyzed using SPSS software version 21.0. The data was expressed in frequency (N), percentage, mean, standard deviation and student’s t-test was used for significance. p value of 0.5 has been taken as statistically significant.
Results
This study included 100 newly diagnosed T2DM patients. Current data on clinical characteristics and gender differences in diabetes are limited. In our study, there was male preponderance and age‑wise increase in prevalence noted, which have been reported in previously in numerous studies. The mean age between the genders was comparable (p>0.05). Majority of female patients had BMI more 30 kg/m2 and majority of male had normal BMI. The glycemic parameter was comparable between both genders. Majority of female patients were having BMI > 30 kg/m2 and male patients had < 29 kg/m2. Past family history of diabetes was seen in 56% female patients (Table 1).
Table 1: Demographic details of study participants.
|
Age (Mean±SD)
|
Female (N=25)
|
Male (N=75)
|
|
48.36±6.06
|
47.08±5.77
|
|
Body mass index (kg/m2)
|
18.5 – 24.9 n (%)
|
3 (12)
|
35 (46.7)
|
|
25-29.99 n (%)
|
4 (16)
|
23 (30.7)
|
|
>30 n (%)
|
18 (72)
|
17 (22.7)
|
|
Past history n (%)
|
14 (56)
|
2 (2.7)
|
N- total number, n- incidence, percentage, SD-standard deviation. Polydipsia, polyphagia and polyuria incidence was more in male patients. Marginal variations were seen with other clinical symptoms. Fatigue was more in female patients (Figure 1).
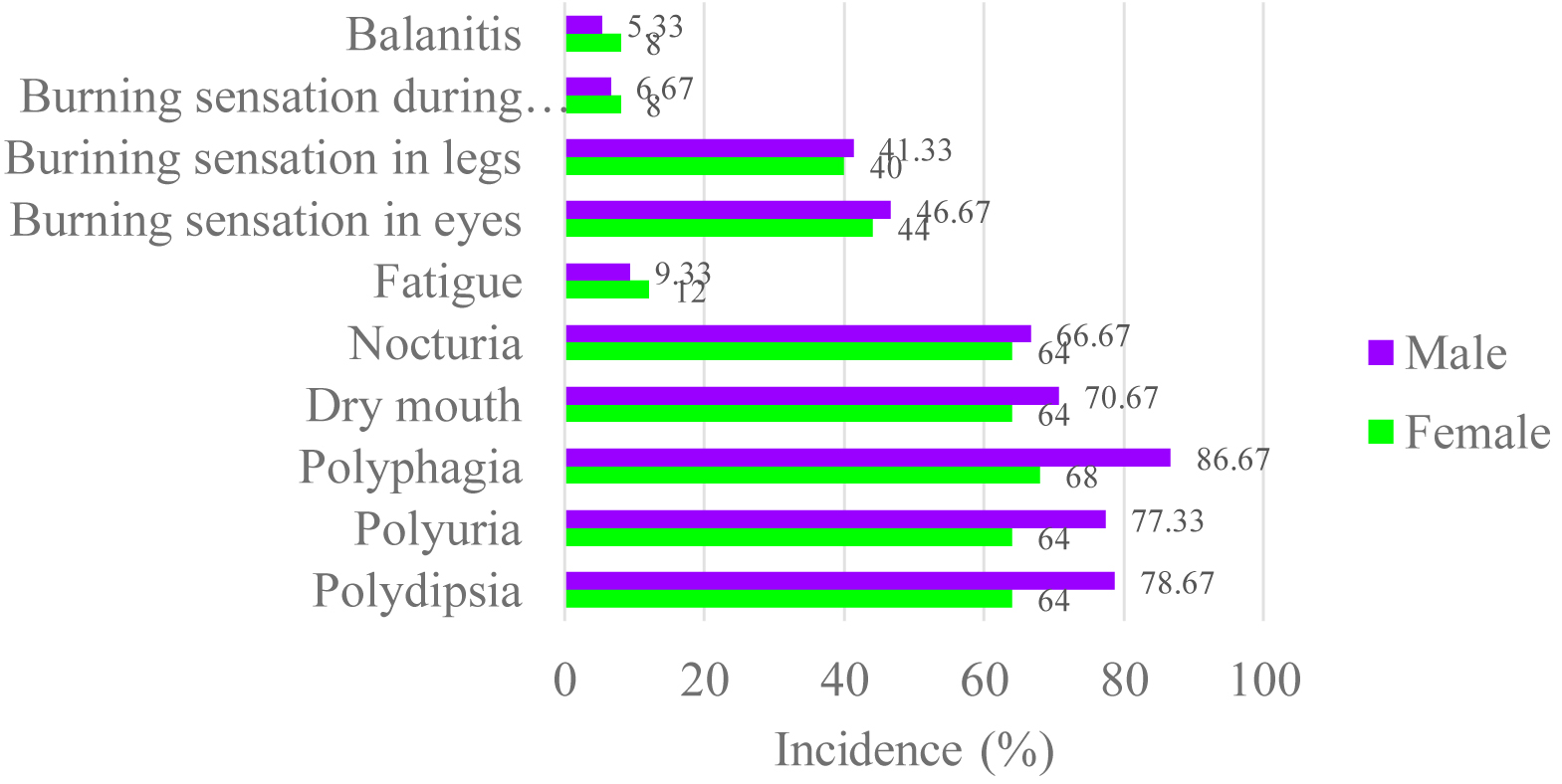
Figure 1: Clinical characteristics of study participants.
The glycemic parameters were comparable among the study groups. Studies including larger population size may show better relationships between the glycemic parameters and study participants (Table 2).
Table 2: Glycemic parameters between genders. SD- standard deviation, significance was obtained using student’s t test.
|
Glucose parameter
|
Female (N=25)
Mean ± SD
|
Male (N=75)
Mean ± SD
|
P value
|
|
Fasting blood sugars (mmol/L)
|
9.05±0.80
|
9.18±0.92
|
0.5
|
|
Post prandial blood sugars (mmol/L)
|
16.54±2.96
|
15.91±2.35
|
0.3
|
|
HBA1C %
|
8.59±0.83
|
8.62±0.76
|
0.8
|
|
CPEP (ng/ml)
|
0.94±0.20
|
0.91±0.19
|
0.1
|
|
HOMA-IR
|
9.67±1.94
|
9.92±1.94
|
0.5
|
During the study period, only 100 patients were enrolled into the study and the gender distribution was not comparable. Yet the study was continued to study the clinical characteristics among the available study samples which may be considered as limitations of the study.
Discussion
Gender differences in the clinical presentation of newly diagnosed T2DM patients at a tertiary care hospital highlight distinct symptom patterns between males and females. Men were more likely to be diagnosed at a younger age, potentially due to higher exposure to modifiable risk factors like smoking, alcohol consumption, and sedentary lifestyles. Women, on the other hand, were diagnosed at a later age, often with more advanced complications such as neuropathy or retinopathy. This delay is often attributed to lower health awareness and socioeconomic constraints impacting timely access to care [13].
Obesity and waist-to-hip ratio were found to be higher in women, indicating a stronger association between central adiposity and diabetes risk in females. Men tended to present with higher fasting glucose levels and lipid abnormalities at diagnosis, suggesting a predisposition to metabolic syndrome. Hormonal factors, such as the protective role of estrogen in premenopausal women, might delay the onset of diabetes, whereas postmenopausal women exhibited higher susceptibility.
Females were found to have a higher incidence of balanitis, attributed to recurrent infections due to poor glycemic control. Similarly, burning micturition was more common among females, likely linked to higher rates of urinary tract infections and delayed healthcare-seeking behavior. Fatigue was also reported more frequently by females, potentially due to anemia, hypothyroidism, or greater psychological stress associated with caregiving roles [14].
Conversely, males exhibited distinct symptomatology, including a higher prevalence of burning sensations in the legs and eyes. Peripheral neuropathy leading to burning sensations in the legs might be more pronounced in males due to a combination of vascular complications and earlier onset of nerve damage [15]. Dry mouth, polyphagia, polyuria, and polydipsia were also more commonly reported in males, reflecting their tendency toward more severe hyperglycemia at diagnosis. Nocturia was particularly prevalent in males, potentially linked to prostate-related issues in addition to diabetes [16].
These gender-specific differences in symptomatology underscore the need for tailored approaches to diagnosis and treatment. For instance, females may benefit from improved screening for urinary and genital infections, as well as interventions addressing fatigue and overall health awareness. In contrast, males may require earlier screening for neuropathy and glycemic control strategies to mitigate hyperglycaemia-related symptoms [17].
The findings also highlight the role of social, cultural, and biological factors in shaping the presentation of T2DM. Gender-sensitive education programs aimed at raising awareness about specific symptoms could aid in early detection and management. Understanding these differences can guide clinicians in adopting a holistic approach to diabetes care that considers the unique needs of both men and women [18, 19].
Conclusion
The study concludes with significant BMI differences between male and female T2DM patients. Patients with these characteristics require special consideration, and health-care providers must be conscious of the possible complications of patient subgroups based on clinical characteristics of DM. Clinical management in DM care should include attempts to symptomatic therapies in this regard.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Bergman M, Buysschaert M, Schwarz PE, Albright A, Narayan KV, et al. Diabetes prevention: global health policy and perspectives from the ground. Diabetes Manag (Lond). 2012; 2:309–321.
[2] Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011; 94:311–21.
[3] Manikowski ST, Atta MG. Diabetic kidney disease: Pathophysiology and therapeutic targets. J Diabetes Res. 2015; 2015:697010.
[4] Wong CW, Wong TY, Cheng CY, Sabanayagam C. Kidney and eye diseases: common risk factors, etiological mechanisms, and pathways. Kidney int. 2014; 85:1290–1302.
[5] Ghanta MK, Nayaka SR, Nuthalapati P, Khan AKA, Elango P, et al. Molecular docking study of Momordica charantia Linn phytoconstituent with caspase 3 and implications for renoprotective actions in diabetes mellitus. J Nephropharmacol. 2025; 14:e10394.
[6] Nwaokoro JC, Okokon BE, Nwaokoro AA, Emerole CO, Ibe SN, et al. Problems associated with treatment compliance among type 2 diabetic patients at a tertiary health institution in Nigeria. Afr J Diabetes Med. 2014; 22.
[7] World Health Organization. Management of Substance Abuse Unit. Global status report on alcohol and health, 2014. World Health Organization. 2014.
[8] Gutch M, Kumar S, Razi SM, Gupta KK, Gupta A. Assessment of insulin sensitivity/resistance. Indian J Endocrinol Metab. 2015; 19:160–164.
[9] WHO Expert Consultation. Appropriate body–mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–163.
[10] Qu HQ, Li Q, Rentfro AR, Fisher–Hoch SP, McCormick JB. The definition of insulin resistance using HOMA–IR for Americans of Mexican descent using machine learning. PloS one. 2011; 6:e21041.
[11] Ramachandran A. Epidemiology of diabetes in India: Three decades of research. J Assoc Physicians India. 2003; 51:771–777.
[12] Pawar SD, Thakur P, Radhe BK, Jadhav H, Behere V, et al. The accuracy of polyuria, polydipsia, polyphagia, and Indian Diabetes Risk Score in adults screened for diabetes mellitus type–II. Med J Dr. DY Patil University. 2017; 10:263.
[13] American Diabetes Association. Standards of Medical Care in Diabetes. Diabetes Care. 2023; 46:S1–S26.
[14] Wandell PE, Carlsson AC. Gender differences and time trends in incidence and prevalence of type 2 diabetes. Diabetologia. 2005; 48:1460–1465.
[15] Nair M. Socioeconomic determinants of diabetes in India. BMJ Open. 2021; 11:e044919.
[16] Manchi RK, Chenchula S, Haritha M. Effectiveness and Safety of metformin, teneligliptin, and glimepiride combination therapy in Type 2 diabetes: A quasi-experimental clinical trial. Curr Diabetes Rev. 2025; 21:102–111.
[17] Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008; 93:S9–30.
[18] Verma S. Gender differences in symptomatology of diabetes in India. J Diabet Res. 2020; 1234567.
[19] Chenchula S, Sharma P, Ghanta MK, Amerneni KC, Rajakarunakaran P, et al. Association and mechanisms of proton pump inhibitors use with Type–2 diabetes mellitus incidence in adults: A systemic review and meta–analysis. Current Diabetes Reviews. 2024; 20:1–2.