Full Text
Introduction
Metastases to the nose and paranasal sinuses are unusual [1]. The most common sinus involved is the maxillary sinus followed by the sphenoid, ethmoid, frontal sinuses and nasal cavity [2]. These tumors are most commonly seen in 4th to 6th decades of life [3]. Several primary malignant neoplasms of different organs can metastasize to nose and paranasal sinuses [5]. The most common one is clear cell renal cell carcinoma, accounting for almost half of the metastases [4]. It is followed by carcinoma breast, colon, thyroid, female genital tract, lymph nodes and brain [6, 7].
The clinical presentation may be analogous to that of primary sino-nasal tumors. Usually they presents with recurrent epistaxis, nasal obstruction, facial pain, proptosis, diplopia and impaired visual acuity [8].
Materials and methods
Retrospective data collected from hospital records of the Krishna Institute of Medical Sciences, Secunderabad, Telangana from 2020 to 2023. Around 233 patients underwent sinus surgery. Histopathology reports of specimens were reviewed. Most of the cases had infectious, inflammatory and allergic pathology. 14 cases were found to be having malignant etiology. Of them 11 cases were primary malignancies (Table 1), 3 cases were metastatic malignancies (Table 2). There were 9 males (64%), and 5 females (36%). They were aged between 14-80 years. The overall incidence of Sino-nasal malignancies was 1.4% (14 in 1000 cases). Which includes esthesioneuroblastoma (14%), chondrosarcoma (7%), lymphoma (7%), carcinoma maxilla (7%), carcinoma ethmoids (7%), carcinoma of sphenoid sinus (7%), carcinoma nasopharynx (14%), recurrent carcinoma nasopharynx (7%), malignant mesenchymal tumor (7%), metastatic carcinoma (27%).
Table 1: Shows malignant neoplasms of nose and paranasal sinuses.
|
Malignant neoplasm
|
Age (In years)
|
Sex
|
No. of cases
|
|
Esthesioneuroblastoma
|
50
|
Male
|
1
|
|
Esthesioneuroblastoma
|
56
|
Female
|
1
|
|
Chondrosarcoma
|
26
|
Male
|
1
|
|
Lymphoma
|
40
|
Male
|
1
|
|
Carcinoma maxilla
|
80
|
Male
|
1
|
|
Carcinoma ethmoids
|
60
|
Female
|
1
|
|
Carcinoma sphenoid sinus
|
14
|
Male
|
1
|
|
Carcinoma nasopharynx
|
17,25
|
Male
|
2
|
|
Recurrent carcinoma nasopharynx
|
45
|
Female
|
1
|
|
Malignant mesenchymal tumor
|
34
|
Male
|
1
|
|
Total
|
11
|
Table 2: Shows metastatic masses of nose and paranasal sinuses.
|
Metastatic neoplasm
|
Age
|
Sex
|
No. of cases
|
|
RCC
|
50
|
Male
|
1
|
|
Non Hodgkin’s lymphoma (Diffuse large B cell)
|
66
|
Female
|
1
|
|
Carcinoma breast
|
40
|
Female
|
1
|
|
Total
|
3
|
Among them we are reporting three metastatic nose and paranasal sinus masses. Which were evaluated in a systematic manner including clinical examination, diagnostic nasal endoscopy, radiological investigation and its management.
Case 1
A 50-years-old male, an electrician by occupation presented to the outpatient department with the complaint of bleeding from the left nasal cavity since 2 days. He was also complaints of nasal obstruction since long time.
He had a history of renal cell carcinoma with extension into the adrenal gland on the right side for which he underwent radical right sided nephrectomy 2 years ago. He is a known case of diabetes and hypertensive on medication.
On nasal endoscopic examination (DNE) a pinkish vascular mass seen between the left middle turbinate and septum (Figure 1).

Figure 1: Diagnostic nasal endoscopy shows a pinkish mass in the left nasal cavity.
Computed tomography scan of nose and paranasal sinuses (CT PNS) revealed a heterogenous lesion involving nose and ethmoidal sinuses with intracranial extension (Figures 2).
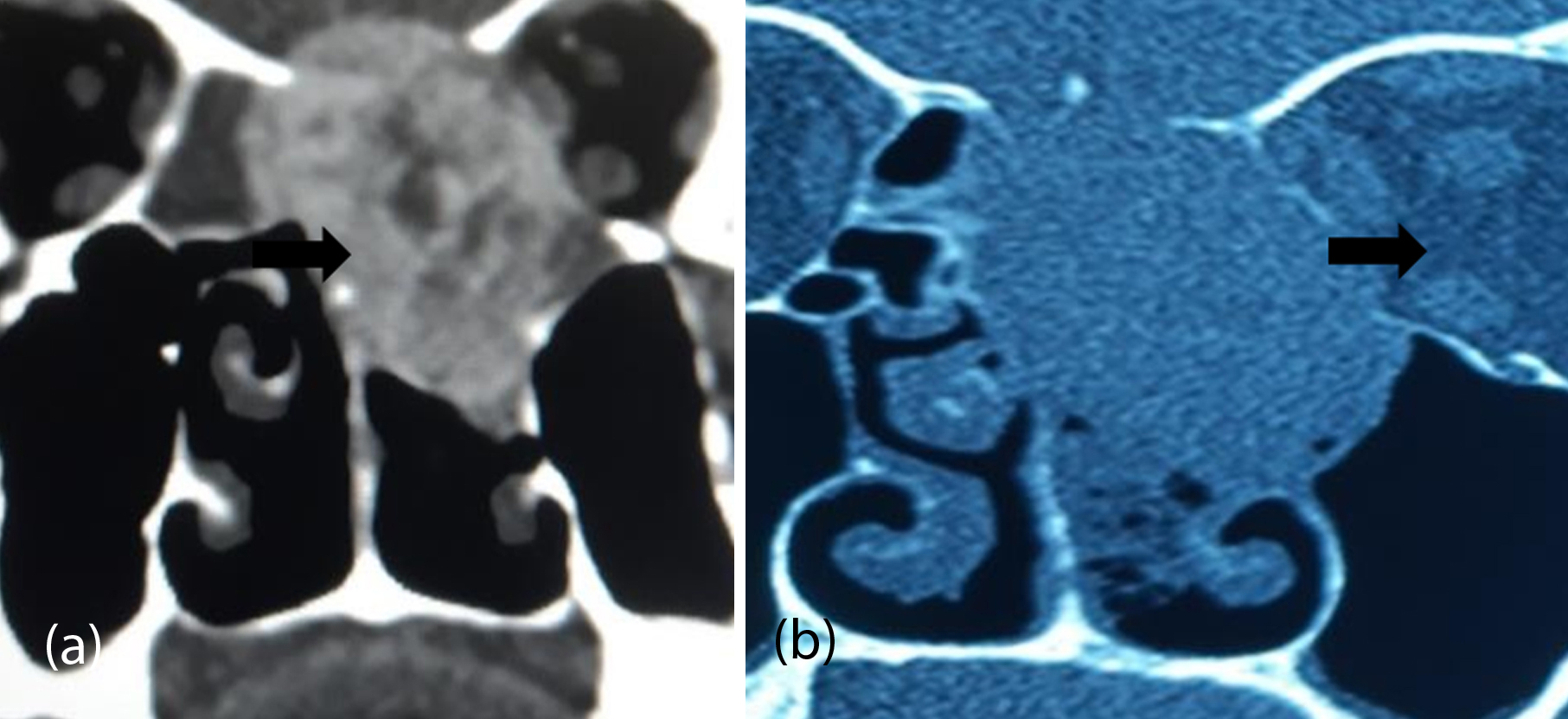
Figure 2a,b: CT scan coronal section shows a well-defined heterogenous lesion in the left nasal cavity with extension into the anterior cranial fossa superiorly, medial wall of left the orbit and maxillary sinus laterally and pushing the septum to the opposite side.
Mass resected endoscopically and the tissue sent for histopathological examination (HPE). It showed a tumor composed of nest of clear cells with vacuolated cytoplasm separated by a vascular septum (Figure3a). Immunohistochemistry (IHC) staining for PAX 8 was positive. All these features are suggestive of metastatic deposits of renal origin (Figure 3b).

Figure 3: (a) Histological findings shows a tumor composed of a nest of clear cells with vacuolated cytoplasm separated by a vascular septum, H&E 400x magnification. (b) Immunohistochemistry shows nuclear positivity with PAX 8, 400x magnification.
He underwent PET CT which showed increased uptake in nose and para nasal sinuses, lung, iliac bone and adrenal gland (Figure 4).
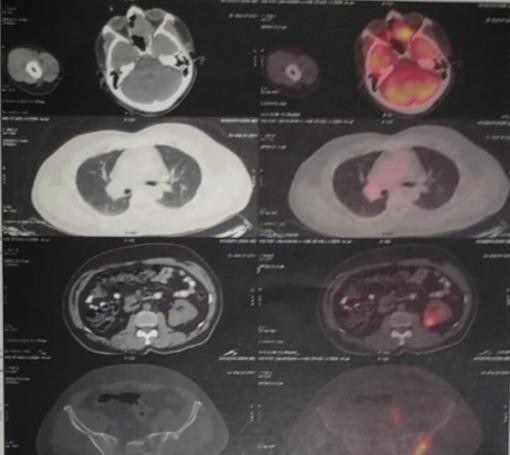
Figure 4: PET CT showing increased uptake suggestive metastasis to PNS, chest, iliac crest, and left adrenal glands.
It is suggestive of metastatic lesion. Patient was advised for further management, but he was reluctant to go for treatment.
Case 2
A 66-year-old female patient presented with complaints of cough with expectoration, intermittent fever and ptosis of left eye for the last 2 months. She was a known case of non-Hodgkin’s lymphoma (NHL) and received chemotherapy 2 years ago.
Diagnostic nasal endoscopy shows mucopurulent discharge in the left nasal cavity. Patient was advised MRI brain and orbits, which revealed as left pan sinusitis with orbital involvement (Figure 5).
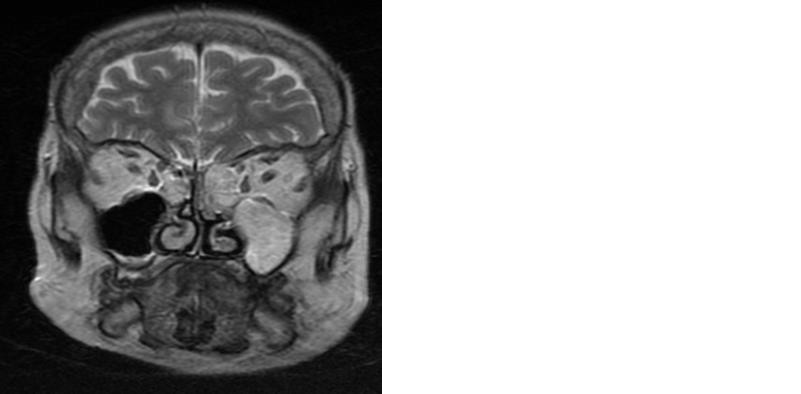
Figure 5: T2-weighted MRI brain and orbits coronal section shows hyperintense lesion involving left maxillary and bilateral ethmoidal sinuses.
Endoscopic sinus surgery done and polypoidal mass in maxillary and ethmoid sinuses excised. The tissue sent for HPE. It revealed as malignant small round cell tumor, probably NHL (Figure 6). On IHC tumor shows strong positivity to CD 20, negativity to CD3 and pan-cytokeratin (Figure 7). All these features are in favor of diffuse large B-cell NHL.
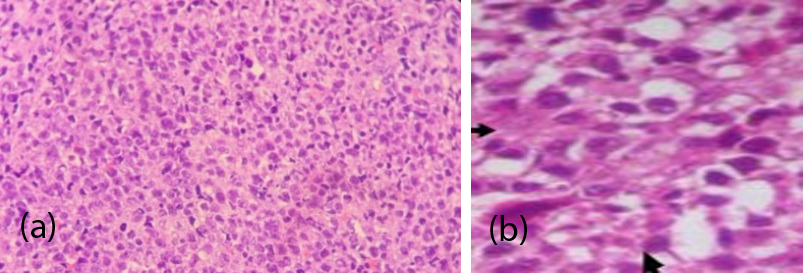
Figure 6: Histopathological examination shows sheets of neoplastic lymphoid cells, (a) 100x magnification, (b) 400x magnification.
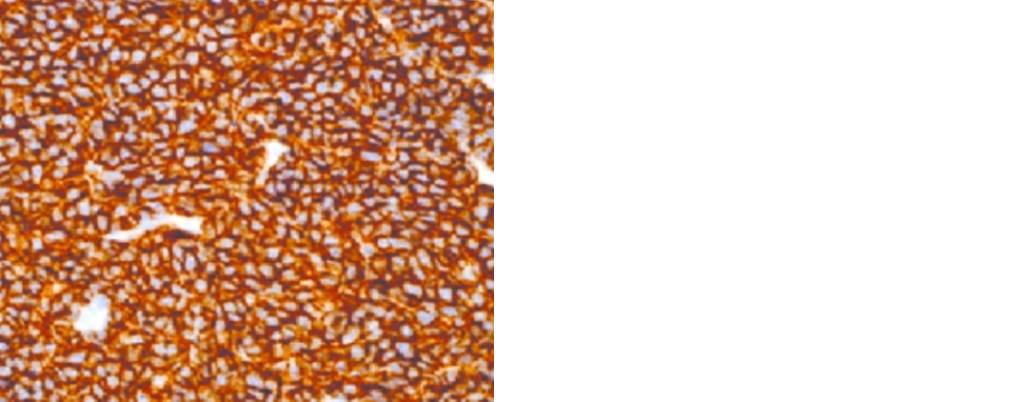
Figure 7: Immunohistochemistry shows positivity to CD 20. 400x magnification.
She was referred to medical oncology department for further management as per the protocol.
Case 3
A 40-years-old female presented to the department with running nose, post nasal drip and headache for the past one month. She also had a history of right sided mastectomy followed by hormonal therapy for carcinoma breast 10 years ago.
DNE shows mucopurulent discharge in the bilateral nasal cavities. CT PNS shows haziness in bilateral paranasal sinuses with heterogeneous opacities with the possibility of fungal sinusitis (Figure 8).

Figure 8: CT PNS coronal section showing heterogenous opacities involving bilateral maxillary sinuses with extension into bilateral ethmoidal sinuses.
Endoscopic sinus surgery was done, tissue was taken from maxillary and ethmoidal sinuses and sent for HPE. It showed a tumor deposits with gland formation, revealed as a metastasis from carcinoma breast (Figure 9). IHC shows neoplastic glands, which are ER-positive. Patient had received combination of chemoradiation.
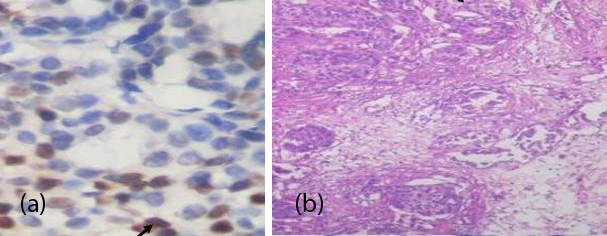
Figure 9: (a) Histopathological examination shows a tumor deposits with gland formation 100x magnification, (b) Immunohistochemistry shows neoplastic glands which are ER-positive 400x magnification.
Discussion
Metastases of primary tumors to the nose and paranasal sinuses are very rare [1]. The clinical presentation is similar to that of primary Sino-nasal tumors, so the diagnosis is often delayed.
In the literature review, renal cell carcinoma is the most common malignancy that metastases to the nose and paranasal sinuses [4]. It is followed by breast, colon, lung, stomach, prostate and lymph nodes have been reported [6, 7].
Most commonly involved sinus by metastatic tumors is maxillary sinus followed by the ethmoids, frontal, sphenoid sinuses and nasal cavity [5]. They are usually present with common nose and ocular symptoms which includes epistaxis, nasal obstruction, facial pain, proptosis, diplopia, decreased vision and ptosis [8]. Metastatic tumors of PNS with primary tumor of unknown origin is very rare. It may reach the PNS by hematogenous, lymphogenous or vertebral venous plexus pathways [9].
Differential diagnosis of sino-nasal metastasis are primary tumors such as adenocarcinomas, hemangiopericytomas, melanomas, hemangiomas, angiofibromas and metastatic tumors from the breast, renal and lungs. Rarely, we can see systemic diseases such as Wegner’s and midline granulomas [10].
CT and MRI of PNS may show either soft tissue masses involving the nose and paranasal sinuses or haziness seen in paranasal sinuses mirroring sinusitis. A definitive diagnosis requires a biopsy for confirmation,that may be obtained via endoscopic sinus surgery [11].
Aim of the treatment of these patients is to improve or maintain their quality of life. Treatment should be customized according to the tumor location and the general health of the patient. Surgery is probably the optimal treatment for patients with resectable sino-nasal metastases. For unresectable tumors, there are other available therapies, which include radiotherapy, chemotherapy, and immunotherapy. Radiotherapy is almost always the treatment of choice for local symptomatic control. The prognosis for patients with metastases to paranasal sinuses is generally poor [12].
Conclusion
Any patient with primary malignancy elsewhere in the body may present with nasal and ocular symptoms. The symptoms may not be specific to the underlying neoplasm and if they are not responding to regular treatment, evaluate the patient with a systematic approach. This includes clinical, endoscopic, radiological and histopathological examination to rule out the possibility of metastasis from primary tumor. Early diagnosis of such metastases will considerably change the prognosis if the intervention is not delayed.
Conflicts of interest
Authors declare no conflicts of interest.
References
[1] Sikdar A, Khan S, Agarwal R, Phatak S, Bhagat P, et al. Metastatic renal cell carcinoma: An enigmatic nasal mass. Indian J Otolaryngol Head Neck Surg. 2023; 75:680–688.
[2] Ruggeri CS, Acosta L, Proietti V, Serrano C. Nasal cavity and paranasal sinuses metastasis. Int J Cancer Clin Res. 2020; 7:143.
[3] Vo NH, Mashiana MK, Shih J, Vo CC, Nguyen J. Renal cell carcinoma metastasis to the maxillary sinus. Ear, Nose Throat J. 2020; 99:NP37–NP39.
[4] Petruzzelli GJ, Shook T, Campbell WJ, Gupta S. Paranasal sinus metastases of renal cell carcinoma: a case report and comprehensive literature review. Ann Clin Case Rep. 2019; 4:1642.
[5] Chang MH, Kuo YJ, Ho CY, Kuan EC, Lan MY. Metastatic tumors of the Sino-nasal cavity: A 15-year review of 17 cases. J Clin Med. 2019; 8:539.
[6] Reitsma S, Schuil PJ. Metastasis of breast carcinoma to the paranasal sinus: report of two cases and systematic review of literature. Rhinol Online. 2018; 1:3–8.
[7] Ravindra P, Viswanatha B. Metastatic lymphoma of the paranasal sinuses. Glob J Otolaryngol. 2018; 16:555943.
[8] Ralli M, Altissimi G, Turchetta R, Rigante M. Metastatic renal cell carcinoma presenting as a paranasal sinus mass: the importance of differential diagnosis. Case Report Otolaryngol. 2017; 2017:9242374.
[9] Mahajan R, Mayappa N, Prashanth V. Metastatic renal cell carcinoma presenting as nasal mass: case report and review of literature. Indian J Otolaryngol Head Neck Surg. 2016; 68:374–376.
[10] López F, Devaney KO, Hanna EY, Rinaldo A, Ferlito A. Metastases to nasal cavity and paranasal sinuses. Head & Neck. 2016; 38:1847–1854.
[11] Kovačić M, Krvavica A, Rudić M. Renal cell carcinoma metastasis to the sinonasal cavity: case report. Acta Clin Croatica. 2015; 54:223–226.
[12] Hong SL, Jung DW, Roh HJ, Cho KS. Metastatic renal cell carcinoma of the posterior nasal septum as the first presentation 10 years after nephrectomy. J Oral Maxillofacial Surg. 2013; 71:1813.