Orginal Research
2024
June
Volume : 12
Issue : 2
Persisting anosmia after COVID-19 infection: The continuing mystery
Sherinsha S, Archana S, Rajesh R
Pdf Page Numbers :- 134-137
Sherinsha S1, Archana S1 and Rajesh R1,*
1Department of ENT, Government T D Medical College, Vandanam, Alappuzha, Kerala 688005, India
*Corresponding Author: Dr. R. Rajesh, Assistant Professor, Department of ENT, Government T D Medical College, Vandanam, Alappuzha, Kerala 688005, India. Email: drrrajeshent@gmail.com
Received 25 January 2024; Revised 11 March 2024; Accepted 18 March 2024; Published 28 March 2024
Citation: Sherinsha S, Archana S, Rajesh R. Persisting anosmia after COVID-19 infection: The continuing mystery. J Med Sci Res. 2024; 12(2):134-137. DOI: http://dx.doi.org/10.17727/JMSR.2024/12-25
Copyright: © 2024 Sherinsha S et al. Published by KIMS Foundation and Research Center. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: COVID-19 pandemic has had a massive impact on global health-care systems and economic stability. Smell and taste dysfunction is now recognized as one of the cardinal symptoms of COVID-19. Since the prevalence of olfactory dysfunction in COVID-19 infection varies from place to place, this study was done to find out the prevalence of olfactory dysfunction in COVID-19 infection, and its persistence on follow-up in a tertiary care centre situated in Alappuzha (South India).
Methods: The present study was a tertiary hospital based descriptive study. 150 patients with COVID-19 Infection who presented to the centre during a period of 6 months were selected, and their detailed history, clinical findings and investigation results were recorded in a proforma. Follow-up of the patients was done for a period of 2 years.
Results: Among the 150 COVID-19 patients 114 (76%) of them had olfactory dysfunction. There were no significant difference in the gender or age distribution, for olfactory dysfunction. Among those with olfactory dysfunction, 88 patients (77.2%) had a faster recovery within 2 weeks. On follow-up, there was persistence of olfactory dysfunction in 2 patients even after 2 years.
Conclusion: The prevalence of olfactory dysfunction seen among COVID-19 patients was much more than that described in studies from other places. The persistence of olfactory dysfunction for a long period in some patients is a matter that needs further research to bring out the causative factors.
Keywords: COVID-19; Olfactory dysfunction; anosmia; prevalence; persistence
Full Text
Introduction
Coronavirus Disease 2019 (COVID-19) outbreak occurred in December 2019 in Wuhan, Hubei Province, China and spread rapidly throughout China, and then emerged around the world [1]. On February 12, 2020, WHO (World Health Organization) named the disease caused by the novel coronavirus as COVID-19. Anosmia is defined as the total absence of all olfactory sensation, which can be caused by a variety of causes, with upper respiratory tract infections being a frequent cause. Among the various pathogens, the most common is the virus, and coronavirus is one of them [2].
Anosmia caused by severe acute respiratory syndrome due to corona virus (SARS-CoV) has been reported during the SARS epidemic in 2003 [3]. However, the incidence of anosmia caused by SARS-CoV-2 (COVID-19) was much higher than that of SARS-CoV. Olfactory dysfunction after COVID-19 infection is due to damage of the olfactory epithelium rather than to the central olfactory pathways [2].
Research is going on in various parts of the world regarding how the virus affects the senses of smell and taste. Significant progress has now been made to reveal the cellular and molecular mechanisms of coronavirus-induced anosmia. Recent work has provided new insights into the cell types in the olfactory epithelium that express the relevant virus entry proteins [4] and that accumulate the virus after infection [5]. The deficit appears to be most often transient; with a regaining of smell and taste within several days or a few weeks [6]. The prospects for making use of the olfactory dysfunction seen in COVID-19 as an early, rapid, and effective diagnostic screening tool can be considered.
We planned to conduct this study since the prevalence of olfactory dysfunction in COVID-19 infection varies from place to place and there aren’t many studies on long term follow-up from south India. The objectives were to study the prevalence of olfactory dysfunction among COVID-19 infected patients in this tertiary care centre in south India as the primary objective, and to study the onset, duration, age & gender predisposition in patients with COVID-19 infection who had olfactory dysfunction.
Materials and methods
This descriptive study was done on patients attending COVID-19 triage at Government T D Medical College, Alappuzha during a period of 6 months from August 2021 to January 2022. Clearance from the institutional ethics committee was obtained prior to the research. All the patients were RTPCR (Reverse transcriptase Polymerase chain reaction) or RAT (Rapid Antigen Test) positive cases. Patients who already had olfactory dysfunction before acquiring COVID-19 infection, patients not giving consent and unconscious patients were excluded from the study.
Minimum sample size was calculated, total of 150 patients were selected and they were interviewed after getting written consent. The personal details of the patient was filled by them in the proforma. The detailed history was collected along with clinical examination findings and investigation reports and documented in the proforma. The patients with olfactory dysfunction were followed up. Statistical analysis was done using IBM SPSS version 25 (Chicago USA).
Results
This study was a tertiary hospital based descriptive study conducted in a centre in south India. 150 patients with COVID-19 Infection who presented to the centre during a period of 6 months were selected, and prevalence of olfactory dysfunction among them was evaluated. Follow-up of the patients was done for a period of 2 years, and duration of persistence of olfactory dysfunction was also assessed. Among the 150 patients, 114 (76%) had olfactory dysfunction (Figure 1).
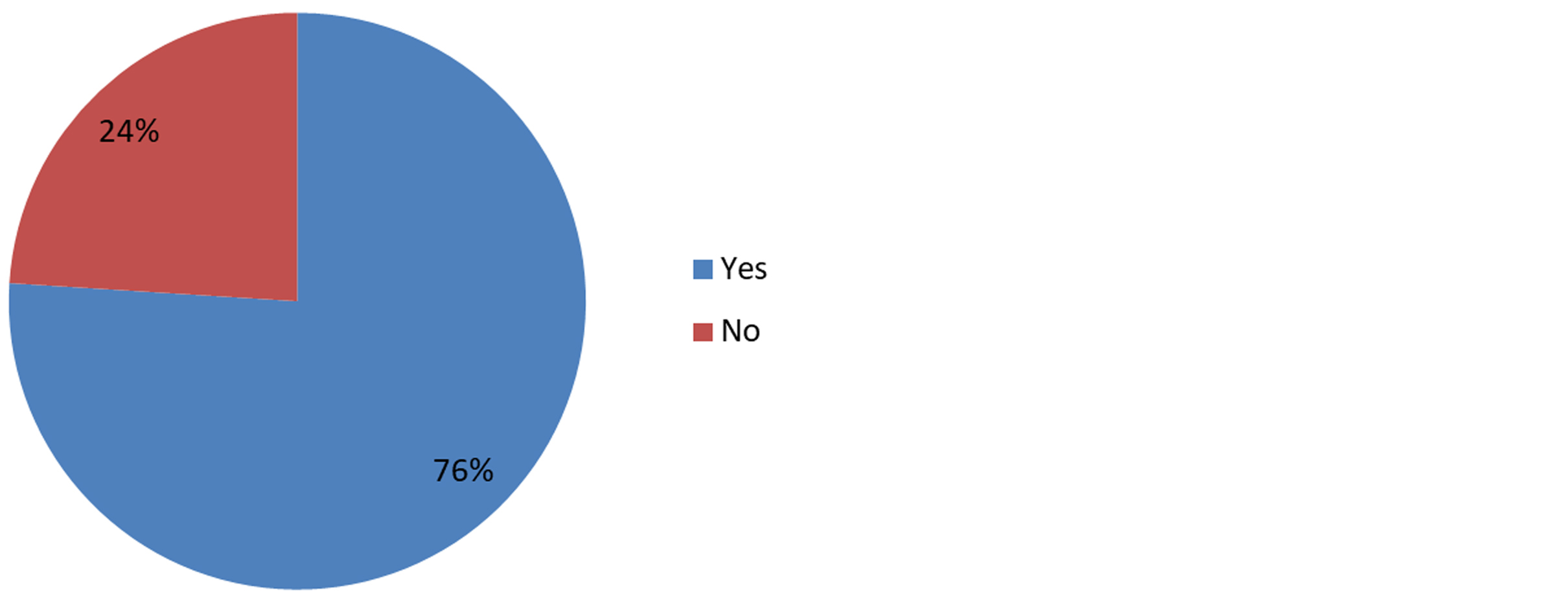
Figure 1: Distribution of Olfactory dysfunction.
70 among 93 males and 44 among 57 females had olfactory dysfunction. The association of gender with olfactory dysfunction was found to be not statistically significant (Table 1).
Table 1: Proportion of olfactory dysfunction in each gender.
|
Gender
|
Olfactory dysfunction
|
Chi square value
|
p value
|
|
Yes
|
No
|
|
Male
|
70(75.3)
|
23(24.7)
|
0.072
|
0.789
|
|
Female
|
44(77.2)
|
13(22.8)
|
Maximum number of patients with olfactory dysfunction was in the age-group of 31-40, which also showed no statistical significance (Table 2).
Table 2: Age distribution of patients with olfactory dysfunction.
|
Age group
|
Olfactory dysfunction
|
Chi Square value
|
p value
|
|
Yes
|
No
|
|
10-20
|
6(85.7)
|
1(14.3)
|
4.117
|
0.535
|
|
21-30
|
20(76.9)
|
6(23.1)
|
|
31-40
|
41(77.4)
|
12(22.6)
|
|
41-50
|
21(63.6)
|
12(36.4)
|
|
51-60
|
19(86.4)
|
3(13.6)
|
|
>60
|
7(77.8)
|
2(22.2)
|
Anosmia and hypogeusia were not initially recognized to be linked to COVID-19; they were mentioned to affect only about 5% of COVID-19 patients in one of the first studies from China by Butowt et al [7], but a much higher prevalence was reported in subsequent studies from other parts of the world. This study concluded that the variation in rates between populations may be due to difference in the spike protein of virus strains, or in the host proteins that enable virus entry. In the study by Von Bartheld et al., the worldwide prevalence of olfactory deficit, taste deficit and any chemosensory deficit was found to be 44.1%, 43.3% & 49% respectively [8].
There was a difference in the prevalence of chemosensory deficits between East Asian and Western populations [9]. The first report that recognized smell and taste reduction to be a much more prevalent symptom came out of Germany, and subsequent studies have confirmed a high prevalence of approximately 60%, especially outside of East Asia. The systematic review by Von Bartheld et al showed three fold higher prevalence in Western than in East Asian population [8].
In our study, Olfactory dysfunction persisted for only less than 2 weeks or less in 88 (77.2%) patients (Figure 2).
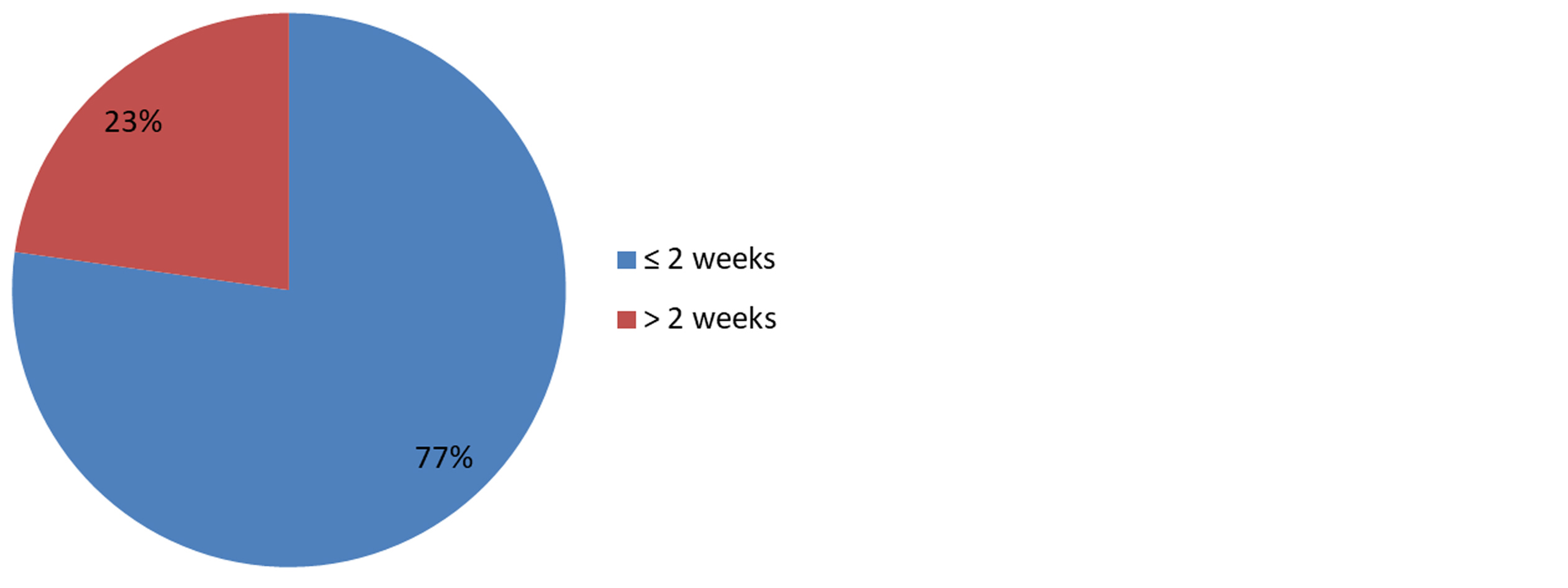
Figure 2: Duration of olfactory dysfunction.
There was no significant association between gender (Table 3) or age (Table 4) with the faster recovery of olfactory dysfunction within 2 weeks.
Table 3: Association between gender and faster recovery of olfactory dysfunction in 2 weeks.
|
Gender
|
Duration
|
Chi square value
|
p value
|
|
≤2 weeks
|
>2 weeks
|
|
Male
|
52(74.3)
|
18(25.7)
|
0.871
|
0.351
|
|
Female
|
36(81.8)
|
8(18.2)
|
Table 4: Association between age and the faster recovery of olfactory dysfunction in 2 weeks.
|
Age group
|
Duration
|
Chi square value
|
p value
|
|
≤2 weeks
|
>2 weeks
|
|
10-20
|
5(83.3)
|
1(16.7)
|
6.061
|
0.273
|
|
21-30
|
14(70)
|
6(30)
|
|
31-40
|
32(78)
|
9(22)
|
|
41-50
|
18(85.7)
|
3(14.3)
|
|
51-60
|
16(84.2)
|
3(15.8)
|
|
>60
|
3(42.9)
|
4(57.1)
|
Olfactory dysfunction persisted in 6, 4, 2, 2 patients at the end of 6 weeks, 6 months, 1 year and 2 years respectively (Table 5).
Table 5: No of patients with persisting olfactory dysfunction on follow-up.
|
Duration of follow-up in 114 patients with olfactory dysfunction
|
No of patients with persisting olfactory dysfunction
|
|
2 weeks
|
26 (22.8%)
|
|
6 weeks
|
6 (5.2%)
|
|
6 months
|
4 (3.5%)
|
|
1 year
|
2 (1.8%)
|
|
2 years
|
2 (1.8%)
|
Discussion
This study was conducted since the prevalence of olfactory dysfunction in COVID-19 infection varies from place to place and there aren’t many studies on long term follow-up from the southern part of India. Our study showed a relatively higher incidence (76%) of olfactory dysfunction among patients with COVID-19 infection. In our study, among the 114 patients who had olfactory dysfunction, it persisted after 2 weeks in only 26 (22.8%) patients. Olfactory dysfunction persisted in 6 patients at the end of 6 weeks, and in 4 patients at 6 months. At the end of 1 year, it persisted in 2 patients (1.75%), which continued even after 2 years.
A study by Reem Mohamed et al demonstrated that post COVID-19 participants with delayed onset of anosmia/hyposmia and/or longer duration of either anosmia/ hyposmia or COVID-19 symptoms were prone to have persistent olfactory dysfunction [10]. Prem et al., in their study, concluded that long-lasting olfactory dysfunction after SARS-CoV-2 infection was a common symptom [11].
The study by Tan et al showed that 5.6% of patients might develop long lasting self-reported smell dysfunction after COVID-19, which is about 15 million patients worldwide as of July 2022 [12]. Meta-analyses of reconstructed time-to-event individual patient data (IPD) showed that at 30, 60, 90, and 180 days, respectively, about 26%, 14%, 10%, and 4% of patients self-reported persistence of olfactory dysfunction.
In the study by Riestra Ayora et al, even though there was high-resolution rates of Olfactory dysfunction during the first two months after the onset of symptoms, at the 6 months follow-up, 30% of the patients had only partial resolution, and 11% of the patients showed no recovery at all [13].
Research is going on in several parts of the world to find out the aetiological and contributory factors for persistent anosmia after COVID-19 infection. A study by Meinhardt et al revealed that the virus can enter the nervous system through the neural-mucosal interface in the olfactory mucosa, due to the close vicinity of olfactory mucosa, endothelium and nervous tissue. Also, it describes the morphological changes due to COVID-19 infection such as infarctions and neurotropism, which may be contributory factors to long-standing olfactory dysfunction [14].
The biopsy-based study by Finlay et al showed infiltration of olfactory epithelium by T cells expressing interferon-gamma, enrichment of CD207+ dentritic cells and depletion of M2 macrophages [15]. Gene expression in the sustentacular cells is accompanied by reduction in the number of sensory neurons. These findings indicate that T cell–mediated inflammation persists in the olfactory epithelium long after SARS-CoV-2 has been eliminated from the tissue, suggesting an immune mechanism for long-term post–COVID-19 smell loss.
The review by Park et al also suggests compromised regenerative potential of stem cells in the olfactory epithelium contributing to permanent olfactory dysfunction, attributable to both cell-autonomous and non-cell-autonomous mechanisms [16]. They may provide a new basis for immediate and long-term translational research on various olfactory stem cells and testing their therapeutic potential. Anyhow, further in-depth research is needed to throw light on this continuing mystery regarding long-term olfactory dysfunction in COVID-19 patients.
Limitations of the study: The data from a tertiary care centre may not precisely reflect the disease profile of the community. Multicentric studies with larger sample size may provide more relevant results.
Conclusion
The prevalence of olfactory dysfunction seen among COVID 19 patients was much more than previously thought, and it supports the fact that it can be considered as a screening and diagnostic symptom for the detection of COVID-19. Olfactory dysfunction persisted for a long period in some patients, as in several other studies, which points out the need of further research in this matter.
Conflicts of interest
The authors declare no conflicts of interest.
References
[1] Li Q, Guan X, Wu P, Wang X, Zhou L, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020; 382:1199–1207.
[2] Hummel T, Whitcroft KL, Andrews P, Altundag A, Cinghi C, et al. Position paper on olfactory dysfunction. Rhinol Suppl 2017; 54:1–30.
[3] Hwang CS. Olfactory neuropathy in severe acute respiratory syndrome: report of a case. Acta Neurol Taiwan 2006; 15:26–28.
[4] Bilinska K, Jakubowska P, von Bartheld CS, Butowt R. Expression of the SARS-CoV-2 entry proteins ACE2 and TMPRSS2, in cells of the olfactory epithelium: identification of cell types and trends with age. ACS Chem Neurosci. 2020; 11:1555–1562.
[5] Bryche B, Deliot ASA, Murri S, Lacôte S, Pulido C, et al. Massive transient damage of the olfactory epithelium associated with infection of sustentacular cells by SARS-CoV-2 in golden Syrian hamsters. 2020. Preprint bioRxiv.
[6] Agyeman AA, Lee Chin K, Landersdorfer CB, Liew D, Ofori-Asenso R. Smell and taste dysfunction in patients with COVID-19: a systematic review and meta-analysis. Mayo Clin Proc. 2020; 95:1621–1631.
[7] Butowt R, von Bartheld CS. Anosmia in COVID-19: Underlying Mechanisms and Assessment of an Olfactory Route to Brain Infection Neuroscientist. 2020; 1073858420956905.
[8] Von Bartheld CS, Hagen MM, Butowt R. Prevalence of chemosensory dysfunction in COVID-19 patients: a systematic review and meta-analysis reveals significant ethnic differences. 2020. MedRxiv preprint.
[9] Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol 2020; 277:2251–2261.
[10] Mohamed R, Alsuhibani R, Almasaoud H, Alabdulazeem L, Alsubhi S, et al. Assessment of anosmia/hyposmia in post-COVID-19 patients: a cross-sectional study in an eastern province of Saudi Arabia. Acta Biomed. 2023; 94:1–11.
[11] Prem B, Liu DT, Besser G, Sharma G, Dultinger LE, et al. Long lasting olfactory dysfunction in COVID 19 patients. European Archives of Oto-Rhino-Laryngology. 2022; 279:3485–3492.
[12] Tan BKJ, Han R, Zhao JJ, Tan NKW, Quah ESH, et al. Prognosis and persistence of smell and taste dysfunction in patients with covid-19: meta-analysis with parametric cure modelling of recovery curves. BJ. 2022; 378:1–12.
[13] Riestra Ayora J, Yanes Diaz J, Esteban Sanchez J, Vaduva C, Molina Quiros C, et al. Long term follow up of olfactory and gustatory dysfunction in COVID 19: 6 months case–control study of health. European Archives of Oto-Rhino-Laryngology. 2021; 278:4831–4837.
[14] Meinhardt J, Radke J, Dittmayer C, Mothes R, Franz J, et al. Olfactory transmucosal SARS-CoV-2 invasion as port of Central Nervous System entry in COVID-19 patients. 2020. Preprint bioRxiv.
[15] Finlay JB, Brann DH, Hachem RA, Jang DW, Oliva AD, et al. Persistent post–COVID-19 smell loss is associated with immune cell infiltration and altered gene expression in olfactory epithelium. Sci Transl Med. 2022; 14:1–14.
[16] Park JW, Wang X, Xu R. Revealing the mystery of persistent smell loss in Long COVID patients. Int J Biol Sci. 2022; 18:4795–4808.